The normal voluntary movements of the hand and finger require exquisite precision and balance in both position and force generation. The very basic elements of the fine motor action elicited by the hand and finger involve flexion and extension and require the integrity and orchestration of the components of the tendon units. In the finger and hand, perhaps more than in any other location in the body, a detailed and intimate understanding of anatomy is crucial for lesion localization, directing clinical management, and predicting long-term prognosis. It is MRI that has emerged as a powerful tool in the identification and characterization of lesions of the extensor and flexor tendons of the hand and finger as a result of its excellent soft tissue contrast and multiplanar imaging capabilities. The basic MRI anatomy of the tendon units of the finger and thumb are discussed. The MRI features of common lesions of the tendons are reviewed.
Extensor Tendon Anatomy of the Finger
Extension at the metacarpophalangeal (MCP), proximal interphalangeal (PIP), and distal interphalangeal (DIP) joints is achieved through the activation of the extrinsic and intrinsic muscles of the fingers, hand, and forearm. The intrinsic muscles, which include the interosseous and lumbrical muscles, originate in the hand and are primarily responsible for extension of the interphalangeal (IP) joints. The extrinsic muscles, which include the extensor digiti minimi, extensor digitorum, and extensor indicis, originate in the elbow and forearm and serve primarily to extend the MCP and IP joints (1–3). Equilibrium and steadiness of the combined efforts of these muscle groups during finger extension is facilitated by surrounding stabilizing soft tissues such as the extensor retinaculum of the carpus, the intertendinous connections and intrinsic muscles of the hand, the extensor hood, and retinacular and triangular ligaments in the fingers (2–4).
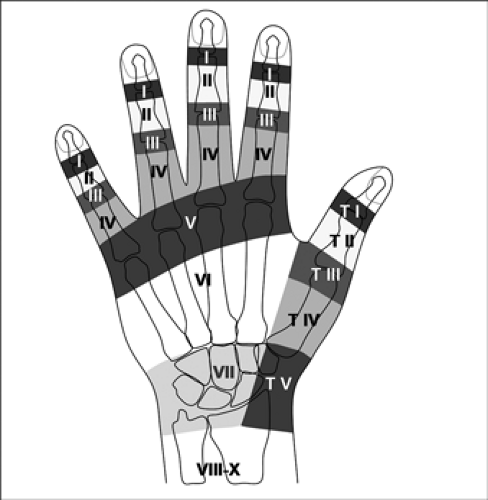
In the setting of such detailed and complex anatomy, classification systems can be helpful in establishing both a bookkeeping system for information organization as well as providing a common language for lesion localization. In the case of the extensor system, the Verdan classification is the system most commonly referred to in orthopaedics (Fig. 19.1) (2, 5). This system provides a topographic classification of zones of the extensor anatomy and includes the extrinsic extensor muscles (Zones VIII–X), the wrist extensor compartments (Zone VII), the dorsum of the hand (Zone VI), the MCP level (Zone V), the proximal phalanx (Zone IV), the PIP (Zone III), the middle phalanx (Zone II), and the DIP (Zone I).
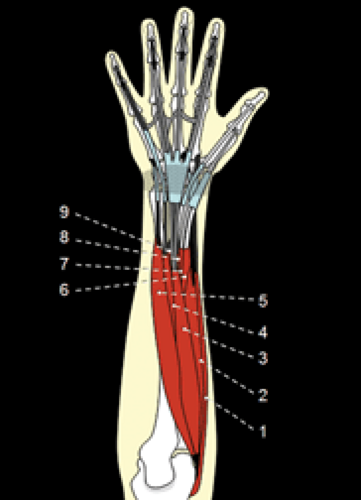
The extensor muscles of the dorsal forearm consist of a group of five superficial muscles and a group of four deep muscles (Fig. 19.2). From radial to ulnar, the superficial extensors consist of the extensor carpi radialis longus, extensor carpi radialis brevis, extensor digitorum, extensor digiti minimi, and extensor carpi ulnaris. These muscles originate from the posterior side of the lateral epicondyle and from the intermuscular septum. The extensor carpi radialis longus inserts on the dorsum of the base of the second metacarpal, the extensor carpi radialis brevis inserts on the dorsum of the base of the third metacarpal, and the extensor digitorum inserts primarily on the dorsal side of the fingers. The extensor digiti minimi inserts on the small finger and the extensor carpi ulnaris inserts on the dorsoulnar side of the base of the fifth metacarpal.
The deep extensors, from radial to ulnar, include the abductor pollicis longus, extensor pollicis brevis, extensor pollicis longus, and extensor indicis. These muscles originate primarily from the interosseous membrane in the midforearm and cross it in an oblique fashion as they move distally to the radial aspect of the wrist. The abductor pollicis longus inserts on the radial base of the first metacarpal, the extensor pollicis brevis inserts on the base of the proximal phalanx of the thumb, the extensor pollicis longus inserts on the dorsal base of the distal phalanx of the thumb, and the extensor indicis inserts on the dorsal side of the index finger.
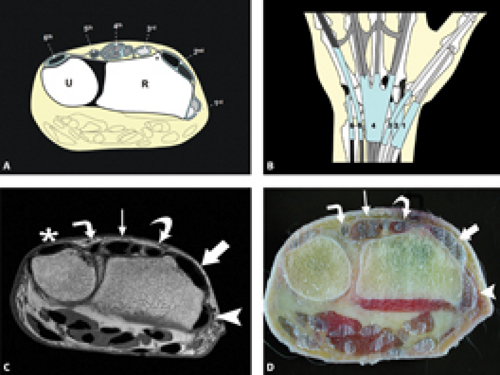
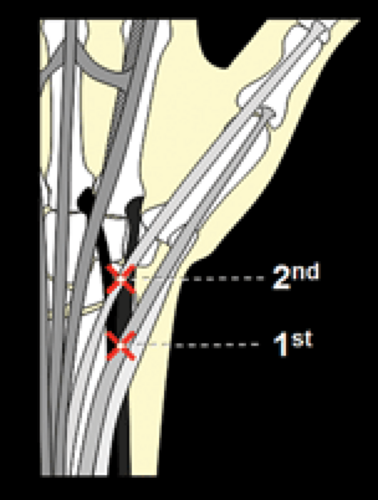
In Zone VII, the wrist extensor compartments are six in number with their corresponding tendons invested within the extensor retinaculum, a strong fascial envelope derived from the antebrachial fascia that anchors the tendons in place and restricts their motion (Fig. 19.3). This retinaculum is derived from the deep parts of the antebrachial fascia and consists of a supra- and infratendinous layer. The infratendinous layer is limited to the most ulnar area, whereas the supratendinous layer forms six septa that insert onto the radius producing the extensor compartments. The tendons are lined by a synovial sheath allowing them to glide easily within their respective compartments. The first compartment contains the abductor pollicis longus and extensor pollicis brevis tendons with the floor comprised of the radial styloid process and insertion of the brachioradialis muscle. In Zone VIII, the first extensor compartment tendons reside in a position ulnar to the tendons of the second extensor compartment. At the junction of Zones VII and VIII, the first compartment tendons cross over those of the second compartment, forming the first intersection between the deep and superficial extensor layers (Fig. 19.4). The second compartment contains the extensor carpi radialis longus and extensor carpi radialis brevis tendons. The third compartment, separated from the
second compartment by Lister’s tubercle, contains the extensor pollicis longus tendon before it crosses over the tendons of the second compartment en route to its final attachment site on the thumb. This represents the second intersection between the deep and superficial extensor layers. The fourth compartment is quite wide and contains the extensor digitorum tendons and, deep to it, the extensor indicis tendon. The fifth compartment is located above the distal radioulnar joint and houses the extensor digiti minimi tendon (usually comprised of two slips). The sixth compartment contains the extensor carpi ulnaris tendon and is located within an indentation along the dorsal aspect of the distal ulnar epiphysis.
second compartment by Lister’s tubercle, contains the extensor pollicis longus tendon before it crosses over the tendons of the second compartment en route to its final attachment site on the thumb. This represents the second intersection between the deep and superficial extensor layers. The fourth compartment is quite wide and contains the extensor digitorum tendons and, deep to it, the extensor indicis tendon. The fifth compartment is located above the distal radioulnar joint and houses the extensor digiti minimi tendon (usually comprised of two slips). The sixth compartment contains the extensor carpi ulnaris tendon and is located within an indentation along the dorsal aspect of the distal ulnar epiphysis.
Zone VI, the dorsum of the hand, shows extensive anatomic variability resulting from tendon multiplicity and the presence of connections between the different tendons. In most cases, there is more than one tendon for each finger between the wrist and the MCP joints (2, 6). The most frequent distribution pattern includes a single extensor indicis tendon located ulnar to the extensor digitorum tendon of the index finger in the MCP joint, a single thick extensor digitorum tendon for the middle finger, a double extensor digitorum tendon for the ring finger, no extensor digitorum tendon for the little finger, and a double extensor digiti minimi tendon for the little finger. In each case, the insertion of the tendon is to the sagittal band of the extensor hood; the latter is also referred to as the dorsal aponeurosis. As noted by the aforementioned distribution pattern, multiple tendons are present more commonly toward the ulnar side of the hand.
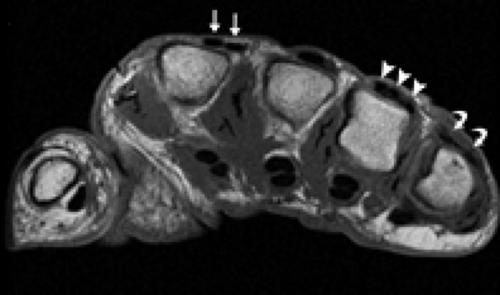
Regarding tendon multiplicity, the most common variations that occur include a double extensor indicis tendon (occurs in over 10% of the population), a double (28%) or triple (16%) extensor digitorum tendon for the middle finger, a single (12%) or triple (16%) extensor digitorum tendon for the ring finger, and a single (19%) or double (26%) extensor digitorum tendon for the little finger (Fig. 19.5) (2, 3, 7). Awareness of the multiplicity of the extensor tendons at the dorsum of the hand is important for the assessment of tendon lesions.
The extensor tendons can show variation in their insertion sites. At the index finger, the extensor indicis may split inserting on both the index and long fingers (8, 9). Slips from the extensor indicis may also insert at the ring finger or thumb (8, 10). At the point of attachment, the extensor indicis has been reported to insert ulnar to the extensor digitorum in greater than 80% of specimens in one study but was directly palmar to the extensor digitorum in approximately 10% and radial to the extensor digitorum in 3% to 8% of specimens (4, 6). Variations in insertion are particularly important in consideration of harvest of the extensor indicis in the setting of tendon transfer.
The extensor tendons are interconnected on the dorsum of the hand by the juncturae tendinum and intertendinous fascia. The former consist of narrow connective
tissue bands extending between the extensor digitorum tendons and the extensor digiti quinti (11). These bands may play a role in spacing the extensor digitorum tendons, serving to redistribute force, coordinate extension, and stabilize the metacarpophalangeal joints (4, 12). They prevent independent extension of the digits and, by bridging the tendons, may mask the clinical presentation of tendon laceration (13). They can sublux across the metacarpal head resulting in a snapping sensation that can mimic trigger finger (14). Of note, this structure can be used in the repair of the dorsal aponeurosis.
tissue bands extending between the extensor digitorum tendons and the extensor digiti quinti (11). These bands may play a role in spacing the extensor digitorum tendons, serving to redistribute force, coordinate extension, and stabilize the metacarpophalangeal joints (4, 12). They prevent independent extension of the digits and, by bridging the tendons, may mask the clinical presentation of tendon laceration (13). They can sublux across the metacarpal head resulting in a snapping sensation that can mimic trigger finger (14). Of note, this structure can be used in the repair of the dorsal aponeurosis.
The juncturae tendinum are reported to become progressively thicker from the radial to the ulnar aspect of the hand (15). Three distinct types have been described (Fig. 19.6) (4, 11). The Type 1 juncturae are thin and filamentous and are found primarily between the extensor tendons to the index and middle fingers and between the tendons to the middle and ring finger. The Type 2 juncturae are thicker, well defined, and present between extensor tendons to the long and ring fingers and between the tendons to the ring and small fingers. The Type 3 juncturae consist of actual tendon slips that extend between the extensor tendons to the middle and ring fingers and between the tendons to the ring and small fingers.
The intertendinous fascia is distinguished from the juncturae in that it attaches to the tendon sheath, not to the tendons. It is present between all the extensor tendons of the fourth compartment regardless of the presence of the juncturae. The intertendinous fascia and the juncturae tendinum allow the extensor tendons to function as a unit and actually impair independent digit extension.
Anomalous muscles occur at the dorsum of the hand. The extensor digitorum brevis manus is a muscle that originates from the dorsum of the carpus or the distal forearm and inserts into the index finger or, less commonly, into the long finger. Its reported prevalence is from 1.1% to 4.7% (8, 16, 17). It may present clinically as a mass on the dorsum of the hand and can become symptomatic in the setting of chronic repetitive trauma as a result of its intimate spatial relationship to the superfi
cial extensor retinaculum (Fig. 19.7). The extensor medii proprius, also known as the extensor medii digiti, is a muscle that can be encountered in up to 10% of hands (6, 9). It is a deep muscle analogous to the extensor indicis but inserts into the dorsal aponeurosis or sagittal band of the long finger.
cial extensor retinaculum (Fig. 19.7). The extensor medii proprius, also known as the extensor medii digiti, is a muscle that can be encountered in up to 10% of hands (6, 9). It is a deep muscle analogous to the extensor indicis but inserts into the dorsal aponeurosis or sagittal band of the long finger.
At the level of the MCP, Zone V, the extensor tendon is invested by the soft tissue network of the extensor hood, also called the dorsal aponeurosis (Fig. 19.8). In combination, these soft tissues serve to extend the finger to the level of the proximal phalanx to stabilize the extensor tendon and to limit its proximal excursion. An important component of the extensor hood is the sagittal band, a capsular fibrous sheet that surrounds the MCP joint in an axial orientation with a volar point of attachment adjacent to the palmar plate and a dorsal point of attachment into the extensor tendon (Fig. 19.9). The sagittal band fibers prevent the extensor tendon from bowstringing with extension, similar to the function of the pulleys of the flexor tendon, and prevent the extensor tendon from subluxing into the trough between the metacarpal heads with flexion. This is discussed in greater detail in the Chapter dedicated to finger ligament anatomy and pathology. Distal to the sagittal bands are transverse and oblique fibers that represent the initial contributions of the intrinsic muscles to the dorsal aponeurosis(18). The intrinsic muscles of the hand, the lumbricals and interosseous muscles, have an intimate relationship with the MCP and the extensor hood (Fig. 19.10). Of seven interosseous muscles in the hand, four are dorsal in location located on the radial side of the second and third metacarpals, the ulnar side of the third and fourth metacarpals. They serve to abduct the fingers, flex the MCP joints, and extend the IP joints. It is the interosseous muscles, located palmar to the deep transverse metacarpal ligament, that contribute both transverse and oblique fibers to the highly vascular soft tissue network
of the extensor hood. These fibers also extend to the region of the lateral tubercle of the proximal phalanx, Zone IV. The multidirectional fibers of the aponeurosis provide a complex plexiform structure with regions of
different mechanical properties that has been compared with a Chinese finger trap (19, 20).
of the extensor hood. These fibers also extend to the region of the lateral tubercle of the proximal phalanx, Zone IV. The multidirectional fibers of the aponeurosis provide a complex plexiform structure with regions of
different mechanical properties that has been compared with a Chinese finger trap (19, 20).
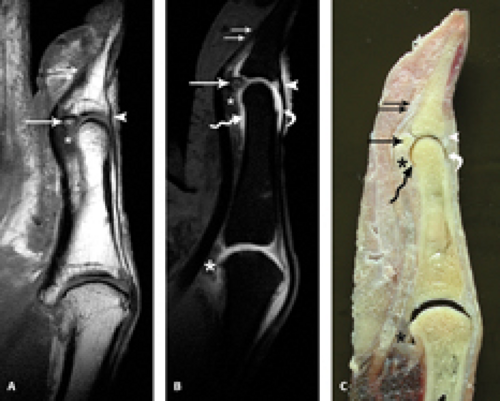
In the region of the proximal phalanx (Zone IV) and the PIP joint (Zone III), the extrinsic extensor tendon divides into central and lateral bands or slips (Fig. 19.8). The central slip inserts on the base of the middle phalanx, whereas the lateral slips merge with the intrinsic tendons of the lumbricals and interosseous muscles to form the conjoined tendons (Fig. 19.11). The conjoined tendons are located at the radial and ulnar aspect of the middle phalanx (Zone II) and converge distally to form the terminal tendon, which inserts on the dorsum of the base of the distal phalanx (Zone I) (Fig. 19.12). The tissue located between the conjoined tendons keeping these structures in a position dorsal to the middle phalanx is called the triangular ligament.
Flexor Tendon Anatomy of the Finger
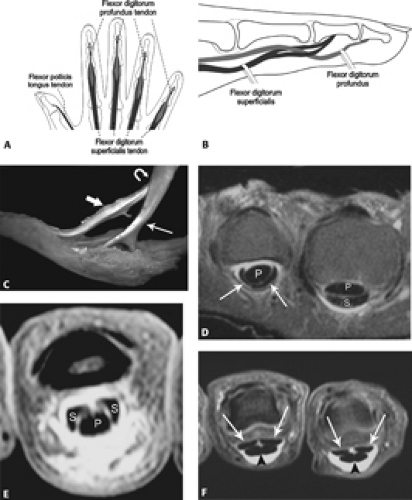
The flexor tendons of the hand and fingers pass through the carpal tunnel of the wrist before separating in the palm and moving toward their ultimate attachment sites in the fingers. Each finger has two flexor tendons, the flexor digitorum superficialis (FDS) and the flexor digitorum profundus (FDP) (Fig. 19.13). The FDS inserts on the midportion of the middle phalanx. Proximal to the
metacarpal head, it lies palmar to the FDP. At the level of the metacarpal, however, it is fenestrated and splits to pass around the FDP forming a ring aperture. Distal to this point, the FDS lies dorsal to the FDP and extends to its attachment on the middle phalanx as previously noted. The FDP passes through the FDS fenestration to become the superficial tendon at the level of the proximal phalanx and inserts distally on the volar base of the distal phalanx.
metacarpal head, it lies palmar to the FDP. At the level of the metacarpal, however, it is fenestrated and splits to pass around the FDP forming a ring aperture. Distal to this point, the FDS lies dorsal to the FDP and extends to its attachment on the middle phalanx as previously noted. The FDP passes through the FDS fenestration to become the superficial tendon at the level of the proximal phalanx and inserts distally on the volar base of the distal phalanx.
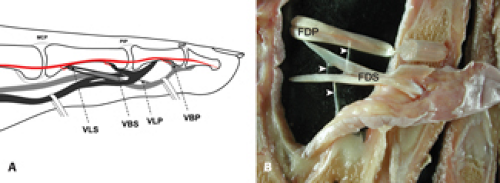
As the flexor tendons approach their osseous attachments, they are connected to the dorsal parts of the enclosing synovial sheaths by triangular or thread-like bands of synovial membrane termed the vincula tendinum. This structure conveys minute vessels to the
tendon attachment site. There are two kinds, the vincula brevia and vincula longa. There are two vincula brevia per finger, one attaching the FDS to the proximal IP joint and adjacent proximal phalanx, the other attaches the FDP to the distal IP joint and adjacent middle phalanx (Fig. 19.14). There are two vincula longa per FDS connected to the tendon slips that pass over the FDP, one on each side of the latter tendon. The vincula in this setting attach to the proximal end of the proximal phalanx. There is one vincula longa associated with the FDP; it is fixed to its tendon just distal to the region where the FDP pierces the FDS. It blends with the vincula brevia of the FDS and attaches to the proximal phalanx.
tendon attachment site. There are two kinds, the vincula brevia and vincula longa. There are two vincula brevia per finger, one attaching the FDS to the proximal IP joint and adjacent proximal phalanx, the other attaches the FDP to the distal IP joint and adjacent middle phalanx (Fig. 19.14). There are two vincula longa per FDS connected to the tendon slips that pass over the FDP, one on each side of the latter tendon. The vincula in this setting attach to the proximal end of the proximal phalanx. There is one vincula longa associated with the FDP; it is fixed to its tendon just distal to the region where the FDP pierces the FDS. It blends with the vincula brevia of the FDS and attaches to the proximal phalanx.
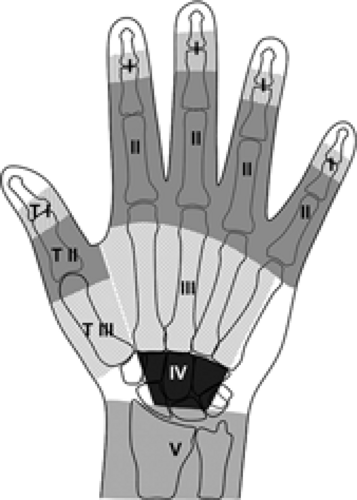
Like in the case of the extensor tendons, a division of the flexor tendons into multiple zones has been established (Fig. 19.15) (1, 5). The flexor tendons are divided into five zones. Zone I extends from the distal insertion of the FDP tendon (distal phalanx) to the distal insertion
of the FDS tendon (middle phalanx). Zone II (the so-called no man’s land) extends from the distal insertion of the FDS tendon to the distal palmar fold. Zone III extends from the proximal part of the A1 pulley (level of the MCP joint) to the distal part of the flexor retinaculum of the carpal tunnel. Zone IV consists of the carpal tunnel, and Zone V includes everything proximal to the carpal tunnel.
of the FDS tendon (middle phalanx). Zone II (the so-called no man’s land) extends from the distal insertion of the FDS tendon to the distal palmar fold. Zone III extends from the proximal part of the A1 pulley (level of the MCP joint) to the distal part of the flexor retinaculum of the carpal tunnel. Zone IV consists of the carpal tunnel, and Zone V includes everything proximal to the carpal tunnel.
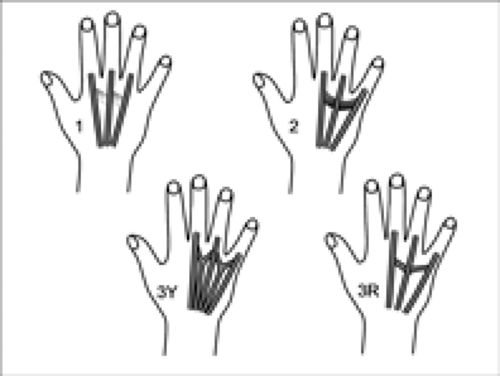
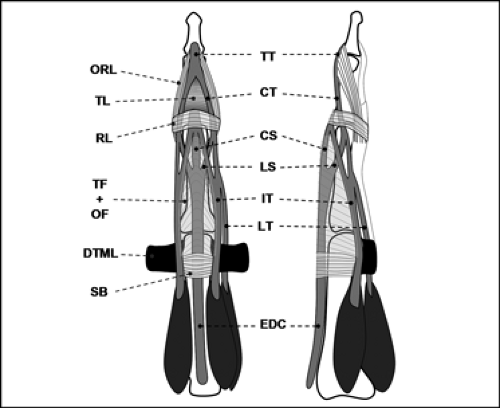
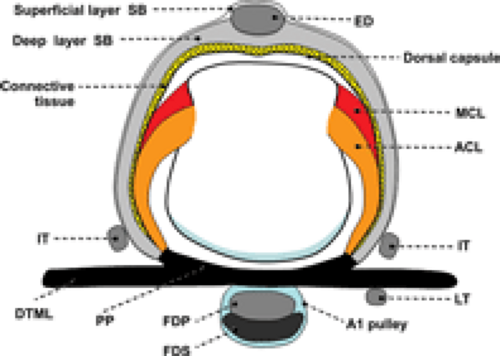
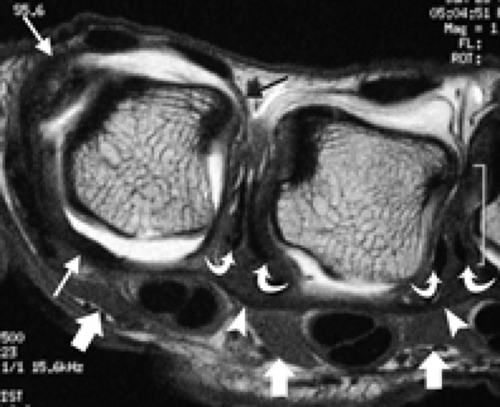
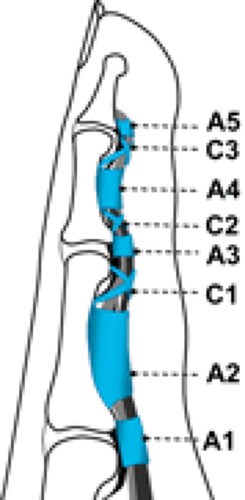
From the neck of the metacarpal to the DIP joint, the flexor tendons run along fibro-osseous canals lined by synovial sheaths that provide nutrients and lubrication to the tendons. The floor of these fibro-osseous canals is formed by the palmar surface of the phalanges and their respective articulations. The fibrous anchors that tether the tendons to the osseous finger are referred to as the pulley system, a network of focal areas of thickening of the flexor tendon sheaths that are required for accurate tendon tracking and serve to facilitate finger flexion by maintaining close apposition of tendon to bone (Fig. 19.16) (21–25). The fibrous portion of the canal consists of five annular pulleys (A1–A5), which are transverse, well-defined areas of thickening of the tendon sheath, and three cruciform pulleys (C1–C3), which are formed by crisscrossing fibers of the components of the annular pulleys.
The first annular pulley (A1) begins in the palmar plate of the MCP joint and extends to the base of the proximal phalanx. The second annular pulley (A2) arises from the volar aspect of the proximal portion of the proximal phalanx and extends to the distal third of the proximal phalanx. The third annular pulley (A3) is diminutive in nature and extends over the region of the PIP joint. The fourth annular pulley (A4) lies in the midportion of the middle phalanx. The fifth annular pulley (A5) is located in the region of the DIP joint. The pulleys can be readily identified on axial MR images as regions of linear low signal intensity that extend from the flexor tendon to the adjacent bone (Fig. 19.17). The A2 and A4 pulleys
are the largest and most substantial of all the annular pulleys. The cruciform pulley system is quite variable in shape and prevalence. These structures, in contradistinction to the annular pulleys, are quite delicate in nature and comprised of a web-like network of fibrous tissue that extends between the annular pulleys. The first cruciform pulley (C1) is located between the A2 and A3 pulleys, the second cruciform pulley (C2) between the A3 and A4 pulleys, and the third and final cruciform pulley (C3) between the A4 and A5 pulleys (Fig. 19.18). Although the annular pulley system functions to stabilize the tendon during flexion as previously noted, the cruciform pulleys are designed to permit deformation of the tendon sheath during flexion without impingement on the tendon proper (21, 22).
are the largest and most substantial of all the annular pulleys. The cruciform pulley system is quite variable in shape and prevalence. These structures, in contradistinction to the annular pulleys, are quite delicate in nature and comprised of a web-like network of fibrous tissue that extends between the annular pulleys. The first cruciform pulley (C1) is located between the A2 and A3 pulleys, the second cruciform pulley (C2) between the A3 and A4 pulleys, and the third and final cruciform pulley (C3) between the A4 and A5 pulleys (Fig. 19.18). Although the annular pulley system functions to stabilize the tendon during flexion as previously noted, the cruciform pulleys are designed to permit deformation of the tendon sheath during flexion without impingement on the tendon proper (21, 22).
Thumb Anatomy
In the thumb, the active movements that can be carried out include flexion–extension, abduction–adduction, rotation, and circumduction. Owing to the geometry of the osseous articulation, flexion and extension take place in a plane parallel to the plane of the palm, whereas abduction and adduction occur in a plane at a right angle to the palm. Although thumb movement is broken down into uniplanar directional components, most intentional motion involves combinations of action. Thumb flexion, except in the earliest stages, is always accompanied with medial rotation. Full thumb extension is generally accompanied by slight lateral rotation.
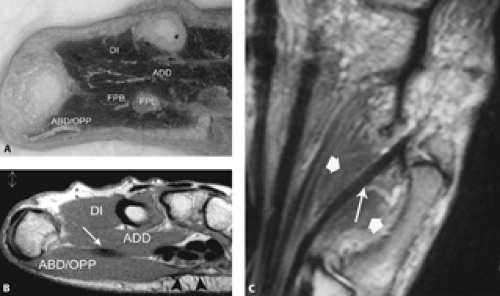
Although thumb extensors and flexors of the thumb are discussed in greater detail, a brief summary of the muscles of the hand facilitating other thumb movement are addressed (Fig. 19.19). Muscles involved will include both extrinsic and intrinsic muscles of the hand. Although not all pertinent to thumb movement, the latter is conveniently organized into three groups: the three muscles of the thenar eminence (abductor pollicis brevis, opponens pollicis, flexor pollicis brevis), the four muscles of the hypothenar eminence (palmaris brevis, abductor digiti minimi, flexor digiti minimi brevis, and opponens digiti minimi), and the central palmar and interosseous muscles in combination with the adductor pollicis longus.
Thumb abduction is elicited by the abductor pollicis brevis and abductor pollicis longus. The abductor pollicis brevis is a thin subcutaneous muscle comprising the radial aspect of the thenar eminence. Its chief origin is from the flexor retinaculum and attaches the radial aspect of the proximal phalanx of the thumb as well as the extensor hood. The abductor pollicis longus is housed within the first extensor compartment. The adductor pollicis is responsible for thumb adduction. It has both oblique and transverse heads that attach to the ulnar side of the base of the proximal phalanx of the thumb with an intimate relationship to the ulnar collateral ligament of the thumb. The opponens pollicis and flexor pollicis brevis simultaneously flex and medially rotate the thumb resulting in opposition. The opponens pollicis is deep to the abductor pollicis brevis and attaches to the lateral aspect of the palmar surface of the first metacarpal bone. The flexor pollicis brevis is medial to the abductor pollicis brevis and attaches by a tendon to the radial side of the proximal phalanx of the thumb (Fig. 19.20). The pressure that the opposed thumb can exercise can be reinforced by recruiting the adductor pollicis and the flexor pollicis longus. Circumduction is the result of sequential activation of the thumb extensors, abductors, flexors, and adductors in that order.
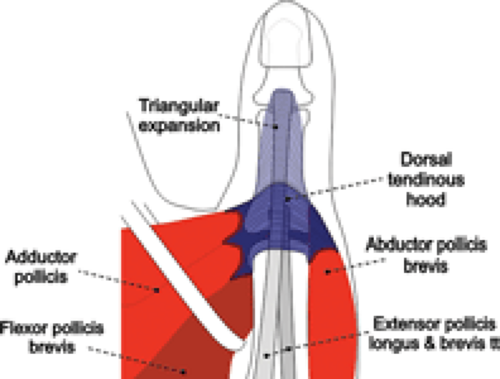
Extension of the thumb differs significantly from the fingers with a somewhat simplified version of the extensor hood composed of the tendons of the extensor pollicis longus and brevis, the dorsal aponeurotic hood, and the triangular expansion. The primary extensors of the thumb are the extensor pollicis brevis and extensor pollicis longus muscles. The abductor pollicis longus also has a small contribution to extension. The thenar muscles (abductor pollicis brevis, flexor pollicis brevis, opponens
pollicis, and adductor pollicis) insert into the extensor hood and contribute to extension of the thumb.
pollicis, and adductor pollicis) insert into the extensor hood and contribute to extension of the thumb.
The extensor pollicis brevis muscle originates from the radius and interosseous membrane on the dorsum of the forearm. Its tendon, with the tendon of abductor pollicis longus, is located in the first dorsal compartment at the wrist. The extensor pollicis brevis inserts into the proximal portion of the dorsum of the proximal phalanx
of the thumb and makes a contribution to the extensor hood of the thumb radial to the attachment of the extensor pollicis longus tendon. These tendinous fibers may form a slender tendon to insert at the base of the distal phalanx deep to the insertion of the extensor pollicis longus (Fig. 19.21). It may, occasionally, be the same size as the extensor pollicis longus. The extensor pollicis brevis extends and abducts the thumb and carpometacarpal joint, extends the MCP joint, and contributes to IP extension. It is innervated by the posterior interosseous nerve. Variations in this muscle anatomy include multiple tendon slips, fusion with the abductor pollicis longus tendon, or absence (5%) (4).
of the thumb and makes a contribution to the extensor hood of the thumb radial to the attachment of the extensor pollicis longus tendon. These tendinous fibers may form a slender tendon to insert at the base of the distal phalanx deep to the insertion of the extensor pollicis longus (Fig. 19.21). It may, occasionally, be the same size as the extensor pollicis longus. The extensor pollicis brevis extends and abducts the thumb and carpometacarpal joint, extends the MCP joint, and contributes to IP extension. It is innervated by the posterior interosseous nerve. Variations in this muscle anatomy include multiple tendon slips, fusion with the abductor pollicis longus tendon, or absence (5%) (4).
The extensor pollicis longus arises from the dorsum of the interosseous membrane and ulna. The tendon is within the third dorsal compartment. After passing around Lister’s tubercle, it runs along the ulnar side of the dorsum of the first metacarpal to the dorsum of the MCP joint. There, it joins the extensor apparatus as a principal component, continuing over the proximal phalanx and inserting widely at the dorsal base of the distal phalanx. It functions to extend the IP joint as well as the MCP joint. It also serves to rotate the first metacarpal laterally, adducts the thumb, and assists in wrist extension and supination. It is innervated by the posterior interosseous nerve.
The dorsal tendinous hood is similar to the sagittal band in the extensor apparatus of the finger (Fig. 19.22). In the thumb, it is attached to the lateral edges of the palmar plate of the MCP joint and dorsally attached to the edges of the extensor pollicis longus and brevis tendons. The fibers of the ulnar part of the dorsal aponeurotic hood are contributed by the tendon of the adductor pollicis, also called the dorsal adductor aponeurosis. The fibers of its radial extent are contributed by the tendons of the flexor pollicis brevis and abductor pollicis brevis, the so-called dorsal thenar aponeurosis. The dorsal tendinous hood functions to maintain the tendons of the ex
tensor pollicis longus and brevis in a stable dorsal position and stabilizes the dorsal MCP joint of the thumb. In addition, it may have some role in extension of the thumb. The fibers of the dorsal tendinous hood extend distally from both the radial and ulnar aspects of the joint in a triangular fashion to form the triangular expansion.
tensor pollicis longus and brevis in a stable dorsal position and stabilizes the dorsal MCP joint of the thumb. In addition, it may have some role in extension of the thumb. The fibers of the dorsal tendinous hood extend distally from both the radial and ulnar aspects of the joint in a triangular fashion to form the triangular expansion.
The abductor pollicis longus muscle originates from the radius, interosseous membrane, and ulna on the dorsum of the forearm. Its tendon travels with the extensor pollicis brevis in the first dorsal compartment. Its primary insertion is into the radial side of the base of the first metacarpal. There are multiple additional slips of insertion, including the trapezium, extensor hood, thenar musculature, and flexor retinaculum. It abducts not only the thumb, but also the wrist. It is innervated by the posterior interosseous nerve.
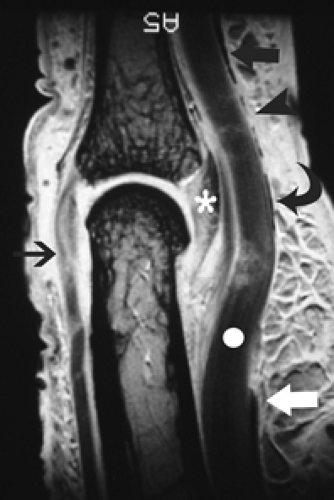
The flexor pollicis longus is the primary flexor of the phalanges of the thumb. It arises from the anterior surface of the radius and from the interosseous membrane. The fibers end in a flattened tendon that passes behind the flexor retinaculum between the opponens pollicis and the adductor pollicis. The tendon then enters a fibro-osseous canal similar to those of the flexor tendons of the fingers. In the thumb, however, there are only two annular pulleys, A1 located at the MCP joint and A2 located at the IP joint. Between the A1 and A2 pulleys, there is an oblique pulley that resides along the course of the proximal phalanx (Fig. 19.23). Of note, the flexor pollicis tendon lacks a vinculum and does not have a lumbrical muscle. This is important because a distal injury to the tendon can lead to retraction of the flexor pollicis longus to the level of the wrist.
Like with the flexors of the fingers, the flexor pollicis longus of the thumb can be arbitrarily divided into zones (Fig. 19.15). Zone I includes the area at the IP joint and the insertion of the flexor pollicis longus. Zone II includes the fibro-osseous sheath that extends along the course of the proximal phalanx to a point just proximal to the metacarpal head and the MCP joint. Zone III includes the area of the metacarpal beneath the thenar muscles, Zone IV corresponds to the carpal tunnel, and Zone V corresponds to the distal forearm just proximal to the wrist.
Extensor Tendon Injuries
Injuries to the extensor tendons of the fingers are common as a result of their superficial location. As a result of the limited excursion of the extensor tendons over the fingers, preservation of tendon length in the setting of injury is crucial for the maintenance of normal tendon function. In addition, lesion location plays an important role in determining the potential deformity that could result from injury as well as the surgical outcome in the setting of repair. It is for this reason that accurate and concise characterization of finger tendon lesions proves crucial with regard to diagnostic considerations.
Although traumatic injury predominates in the fingers, chronic repetitive microtrauma in the form of overuse-type syndromes are experienced in the more proximal zones of the extensor apparatus. Commonly encountered extensor tendon pathology is reviewed.
Overuse Syndromes
de Quervain’s Disease
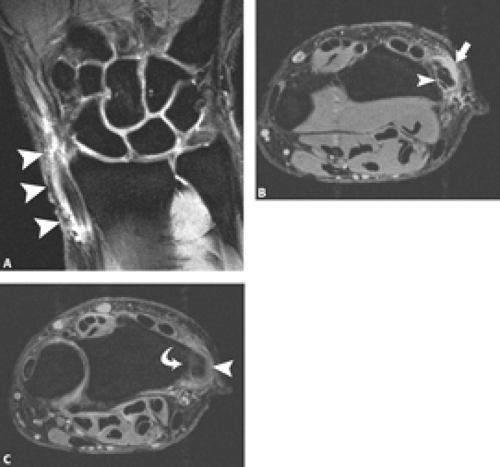
de Quervain’s disease is characterized by tendinopathy and stenosing tendovaginitis of the first extensor compartment and its contents, the abductor pollicis longus and the extensor pollicis brevis tendons. Typically the
inflammation associated with this entity occurs at the level of the radial styloid process, Zone VII. On physical examination, a focal area of swelling can be palpated in the region of the radial styloid process. Pain at the area of palpable abnormality with (a) ulnar deviation of the wrist with the thumb adducted or (b) active extension and abduction of the thumb against resistance is considered pathognomonic for de Quervain’s disease.
inflammation associated with this entity occurs at the level of the radial styloid process, Zone VII. On physical examination, a focal area of swelling can be palpated in the region of the radial styloid process. Pain at the area of palpable abnormality with (a) ulnar deviation of the wrist with the thumb adducted or (b) active extension and abduction of the thumb against resistance is considered pathognomonic for de Quervain’s disease.
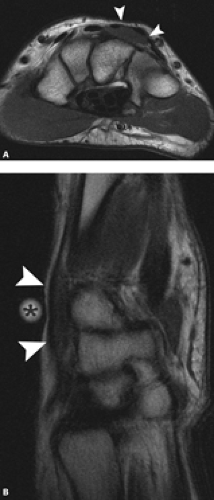
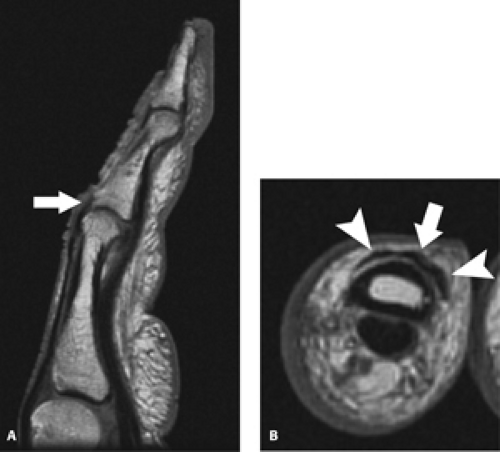
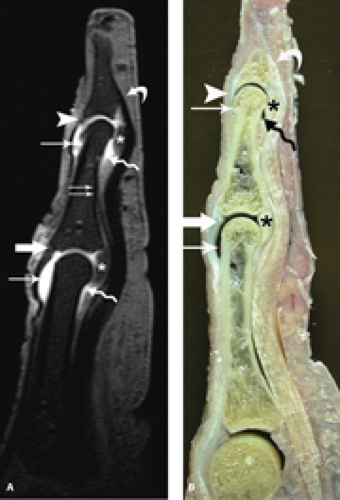
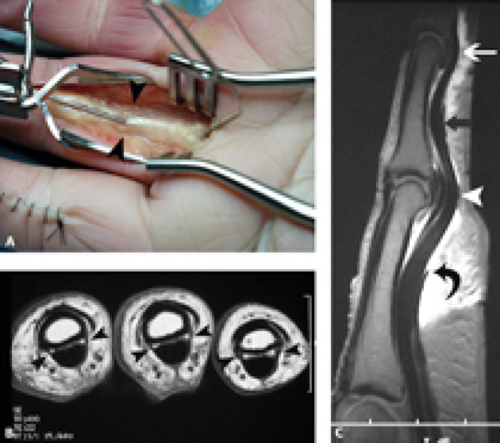
The MRI findings include those of tendinosis. The diagnosis of tendinosis is characterized by abnormal morphology in the form of thickening (can be determined by comparing with the relative size of the tendons in Compartments 2 through 6) or abnormal signal intensity characterized by increased signal intensity on T1-weighted images that does not brighten to the level of simple fluid on fluid-sensitive sequences. Tears of the tendons superimposed on tendinosis can also be encountered (Fig. 19.24). The presence of fluid localized to the tendon sheath or compartment as well as surrounding soft tissue edema with loss of adjacent fat
planes and adjacent bone marrow edema at the radial styloid can also help to establish this diagnosis (Fig. 19.25). It has been reported in the literature that the isolated finding of increased signal intensity within the tendon substance is an unreliable sign of de Quervain’s disease (26, 27).
planes and adjacent bone marrow edema at the radial styloid can also help to establish this diagnosis (Fig. 19.25). It has been reported in the literature that the isolated finding of increased signal intensity within the tendon substance is an unreliable sign of de Quervain’s disease (26, 27).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree