The most unstable articulation in the body, the glenohumeral joint, is subject to subluxation, dislocation, and microinstability. Instability has many etiologies, including a single or recurrent posttraumatic event, congenital ligamentous laxity or hypoplasia of the glenoid, referred to as atraumatic instability, and repetitive mechanical derangement as a consequence of labrocapsular abnormalities.
During the last 2 decades, MRI has allowed for direct visualization of many of the lesions related to instability, aiding in diagnosis as well as therapeutic planning and follow up. These include abnormalities of the labrum, the osseous and cartilaginous portions of the humerus and glenoid as well as the glenohumeral ligaments, capsule, rotator cuff tendons, and biceps tendon. Sequelae of accompanying nerve damage in the form of direct neural compression as a result of perilabral cysts or related to nerve traction caused by shoulder dislocation or traumatic stretching as well as neuritis can be well visualized by MRI.
Clinical Classification
The unstable shoulder can be classified according to etiology (traumatic versus atraumatic), severity (dislocation or subluxation), and direction of instability (unidirectional or multidirectional) (1). The temporal relationship with regard to the event (acute first time versus recurrent) is also a consideration. Ninety percent of cases of shoulder instability related to trauma are in the anterior direction. These are caused by a fall on an outstretched hand or contact and collision sports. The abducted and externally rotated shoulder undergoes a sudden external rotation or extension force.
Regarding anterior instability, there are several broad clinical categories related to the presence or absence of antecedent trauma producing the instability, and it is important to differentiate between them for successful treatment. These include the TUBS and AMBRII and AIOS classifications. Traumatic dislocations resulting in unidirectional anteroinferior instability with a Bankart lesion is referred to by the acronym TUBS—Traumatic onset of Unidirectional instability, in which a Bankart lesion is typically present, usually requiring Surgery. Conversely, atraumatic instability is often caused by congenital capsular laxity or glenoid hypoplasia and is covered by the acronym AMBRII whose onset is Atraumatic, Multidirectional, often Bilateral, often responds to Rehabilitation, and when unresponsive to nonoperative measures requires an Inferior capsular shift and rotator Interval closure (2, 3). Those with ABMRII are often young females without labroligamentous injury. The labrum is often hypoplastic and the ligaments are lax. A similar form of instability, termed Acquired Instability Overstress Surgery (AIOS), is seen in athletes who participate in throwing sports and swimming as a result of repetitive microtrauma and this form of instability tends to be multidirectional. Functional instability is a sensation of instability without a clinical demonstration of instability related to labral tears (4).
The less common posterior instability is often classified according to frequency, degree, direction, and cause, similar to anterior instability (5). The criteria include single versus multiple events; subluxation or dislocation, uni- or bi-, or multidirectional; and traumatic versus atraumatic etiologies.
Recurrent instability is often seen in patients who have their first dislocation when younger than age 20 years. Most recurrences occur within 2 years of the initial dislocation event. Recurrent instability is much less common between the ages of 30 and 40 years.
Subtle or occult glenohumeral subluxation resulting in internal impingement may present with nonspecific shoulder pain (4, 6, 7). In athletes, pain that occurs in the early cocking phase is often the result of anterior microinstability and symptoms that occur during the late cocking or acceleration phase tend to be related to posterior microinstability.
Technical Overview
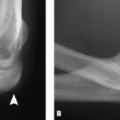
Radiographs are useful for the initial workup of shoulder instability. They can demonstrate joint space narrowing, a high-riding shoulder (suggestive of large rotator cuff tears), fractures such as Hill Sachs and Bankart lesions, dislocation, subluxation, osteophytes, erosions, sclerosis, subchondral cysts, abnormal bone density, and joint and soft tissue ossification and calcification. Before and after reduction, a true anteroposterior (Grashey view) (Fig. 5.1) and either a transscapular (Fig. 5.2) or axillary view (Fig. 5.3) are obtained to determine if there is dislocation, adequacy of reduction, and associated fractures such as the Hill Sachs or osseous Bankart. The transscapular view is also called the scapular “Y” view and it can be taken in the erect or supine position, in the posteroanterior direction, with the affected shoulder rotated anteriorly 45 degrees. The arm is positioned at the side superimposed on the scapula. The axillary projection is obtained with the patient in the supine position and the arm placed in 90 degrees of abduction. The angle of the x-ray beam is approximately 30 degrees toward the spine with the beam centered on the middle of the glenohumeral joint.
Special views can be obtained to demonstrate a Hill Sachs lesion (Stryker notch view) (Fig. 5.4) or the
osseous Bankart lesion (West Point view) (Fig. 5.5). The Stryker notch view is obtained with the patient in the supine position with the arm externally rotated and abducted and the x-ray beam angled 10 degrees cephalad and centered on the coracoid process. The patient’s hand supports the back of the head with the elbow pointed toward the ceiling. The West Point view is obtained with the patient in the prone position with the shoulder resting on a cushion. The arm is abducted 90 degrees and the patient’s forearm and hand are in pronation hanging downward off the edge of the table. The anteroinferior (arrow) portion of the glenoid is seen without overlap of the coracoid.
osseous Bankart lesion (West Point view) (Fig. 5.5). The Stryker notch view is obtained with the patient in the supine position with the arm externally rotated and abducted and the x-ray beam angled 10 degrees cephalad and centered on the coracoid process. The patient’s hand supports the back of the head with the elbow pointed toward the ceiling. The West Point view is obtained with the patient in the prone position with the shoulder resting on a cushion. The arm is abducted 90 degrees and the patient’s forearm and hand are in pronation hanging downward off the edge of the table. The anteroinferior (arrow) portion of the glenoid is seen without overlap of the coracoid.
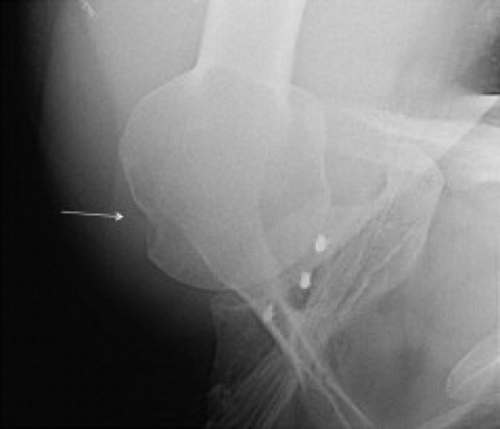 Figure 5.4 Hill Sachs on Stryker notch view (arrow). There is also a labral repair with suture anchors along the glenoid rim. |
Beyond that, the patient may need more sophisticated imaging studies to reach the diagnosis. Occasionally that may be in the form of computed tomography (CT) or CT arthrography, but most often it is the MRI that is the next step in the workup of shoulder instability.
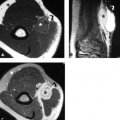
Arthro-computerized tomography (arthroCT) and MRI have been used to evaluate the capsular and labral structures (8–11). As a result of limited soft tissue contrast, arthroCT is weak for evaluation of internal characteristics of tissues, including tendon degeneration, intrasubstance tears of tendons, ligaments, hyaline and fibrocartilage, and bone marrow pathology. On occasion, small osseous fragments and cartilage lesions are better seen on CT (Fig. 5.6). ArthroCT is usually reserved for patients who cannot undergo MRI as a result of contraindications such as the presence of a cardiac pacemaker or cochlear implant.
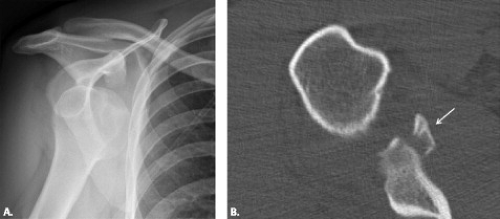 Figure 5.6 A: Anterior dislocation of the humerus seen on an anteroposterior radiograph. B: The followup computed tomography scan after reduction demonstrates an osseous Bankart lesion (arrow). |
Studies using conventional (unenhanced) MRI in the evaluation of glenohumeral instability have produced mixed results in the detection of labral tears with sensitivities and specificities ranging from 44% to 100% and 66% to 95%, respectively (4, 12–16). MR arthrography has generally produced sensitivities between 86% and 91% and specificities of 86% and 98% (11, 17–19). Although controversial and with some opposing opinions often related to workplace circumstance or lack of familiarity with MR arthrography, many believe that labral tears and ligamentous lesions are best evaluated when there is a large joint effusion or with MR arthrography (20–22). High-resolution noncontrast MR imaging can also be of value for evaluating the labrum when MR arthrography is not available (14, 16). The use of 3.0-T MRI for labral tears has also been explored. Sensitivity of MRI for detection of superior labral anterior posterior (SLAP) lesions was 90% and specificity was 100% in 67 patients in one study (23). That research showed the sensitivity for anterior and posterior labral tears to be 89% and 86% and specificity as 100% and 100%, respectively. Technical considerations regarding imaging of the shoulder with MRI are covered in the technical considerations chapter of this book.
Anatomic Considerations
The glenohumeral joint is stabilized by both static and dynamic mechanisms. The interplay between these two types of restraints allows for the wide range of motion of the joint and imbalance in this relationship can lead to shoulder instability. Static restraints include the glenohumeral articular geometry, the glenoid labrum, the glenohumeral ligaments, rotator interval, and the capsule. The static stabilizers function at the extremes of motion. Dynamic restraints include the rotator cuff muscles and tendons, the long head of the biceps tendon, and the scapular stabilizers (latissimus dorsi, trapezius, rhomboids, and serratus anterior muscles).
The anterior complex includes the supraspinatus muscle and tendon, subscapularis muscle and tendon, rotator interval between the supraspinatus and subscapularis, anterior capsule, glenohumeral ligaments, synovial membrane, anterior labrum, and osseous glenoid. The posterior complex includes the infraspinatus muscle and tendon, teres minor muscle and tendon, posterior capsule (including the posterior band of the inferior glenohumeral ligament), synovial membrane, posterior labrum, and osseous glenoid.
Glenohumeral Joint
The glenohumeral joint is formed by the humeral head and the glenoid articular surface of the scapula. The glenoid articular surface has a mean retroversion of
7 degrees (Fig. 5.7). In 25% of cases, it has a mean anteversion of 2 to 10 degrees (24). The glenoid may also be shallow or hypoplastic. These variations can predispose to glenohumeral instability. Centrally, there is thickening of subchondral bone with cartilage thinning over the region. This is called the tubercle of Assaki and it should not be mistaken for a cartilage defect (25) (Fig. 5.8).
7 degrees (Fig. 5.7). In 25% of cases, it has a mean anteversion of 2 to 10 degrees (24). The glenoid may also be shallow or hypoplastic. These variations can predispose to glenohumeral instability. Centrally, there is thickening of subchondral bone with cartilage thinning over the region. This is called the tubercle of Assaki and it should not be mistaken for a cartilage defect (25) (Fig. 5.8).
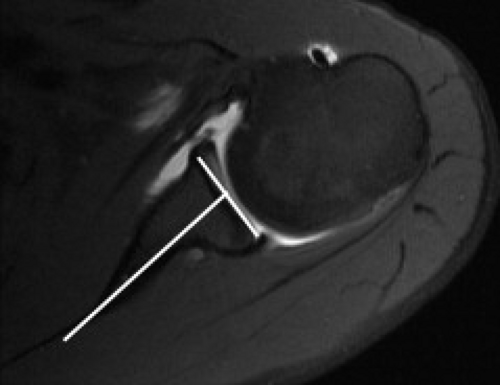 Figure 5.7 Axial fat-suppressed T1-weighted MR arthrogram at the level of the midglenohumeral joint shows normal slight retroversion of the osseous glenoid. |
Normal Labrum and Anatomic Variants
The fibrous connective tissue glenoid labrum is an important structure that provides passive stability with dispersion of strain and pressure. It completely rims and deepens the shallow glenoid fossa, increasing the contact area for the humeral head and limiting excessive translation of the joint (Fig. 5.9). The labrum doubles the anteroposterior depth of the glenoid socket from 2.5 to 5 mm and deepens the concavity to 9 mm in the superior–inferior plane (26). Labral resection or tear can decrease resistance to translation in shoulders that are subjected to a compressive load (27). The intact labrum also acts as a pressure seal, allowing negative pressure to occur within the shoulder during motion, aiding in the dynamic stabilization of the joint. In addition, the labrum serves as an anchor for some of the glenohumeral ligaments as well as the long head of the biceps tendon.
Normally, the labrum is larger in its superior and posterior regions. It can be triangular, rounded, crescent-shaped, or blunted on transverse sections. The normal labrum can vary in width and thickness from 2 to 14 mm.
Normally, the labrum is larger in its superior and posterior regions. It can be triangular, rounded, crescent-shaped, or blunted on transverse sections. The normal labrum can vary in width and thickness from 2 to 14 mm.
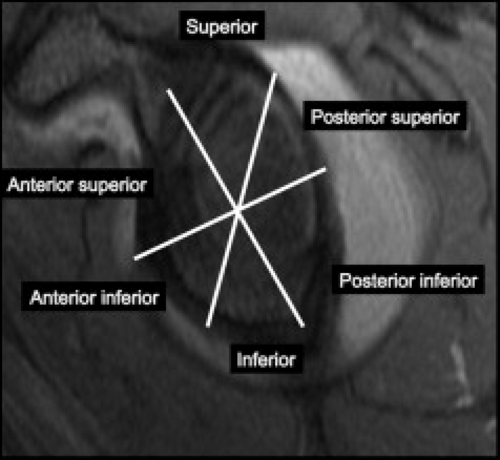
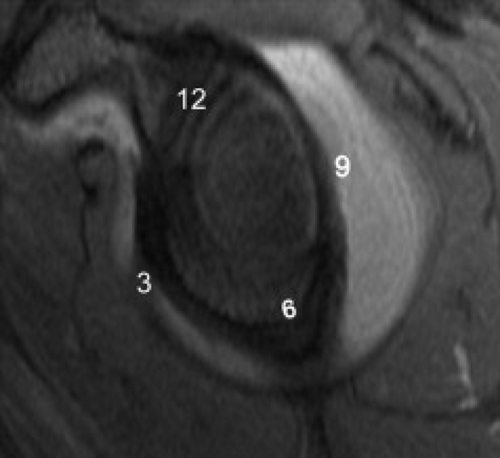
It is helpful to divide the labrum into various regions (Fig. 5.10). This can be accomplished by dividing the labrum anatomically into six segments that include the superior, posterior–superior, posterior–inferior, inferior, anterior–inferior, and anterior–superior regions. Alternatively, one can use the face of a clock to describe the location of abnormalities. With this method, 12 o’clock is at the top under the coracoid and 6 o’clock is 180 degrees from the top at the inferior labrum. The latter method works when 3 o’clock is considered the midportion of the anterior labrum and 9 o’clock is at the midportion of the posterior labrum (Fig. 5.11). This method is plagued by the fact that some surgeons change the clock face so that 3 and 9 o’clock are different for left and right shoulders. Still, most use these criteria and do not have a problem with the clock face description, which can be quite accurate. In this book, we use both descriptions and assume that 3 o’clock is the anterior labrum.
The usually low-signal–intensity labrum lies on a fibrocartilage transition to hyaline articular cartilage (Fig. 5.9). The hyaline cartilage is higher signal intensity than the labrum on all imaging sequences and should not be mistaken for a tear at the base of the labrum.
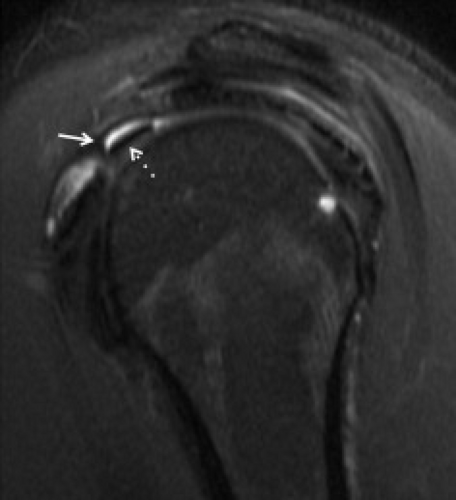
The labrum is best seen when there is fluid in the joint in the form of an effusion or arthrogram. First-time dislocators often have some effusion in the initial few weeks after trauma and an arthrogram may not be necessary to outline the labrocapsular structures. Otherwise, if the dislocation is more than a few weeks, it is recommended that the patient have a direct MR arthrogram. If that is not available, a high-resolution MRI or an indirect (intravenous) MR arthrogram would be suggested (16, 28–31). Abduction and external rotation (ABER) imaging can aid in evaluation of the anterior–inferior and posterior–superior labrum (Fig. 5.12). The ABER sequence obtained during an MR arthrogram improves
the accuracy of interpretation of the labral lesion and can bring out associated articular surface supraspinatus and infraspinatus tears as described in the rotator cuff Chapter (32–34).
the accuracy of interpretation of the labral lesion and can bring out associated articular surface supraspinatus and infraspinatus tears as described in the rotator cuff Chapter (32–34).
Ligaments and Joint Capsule
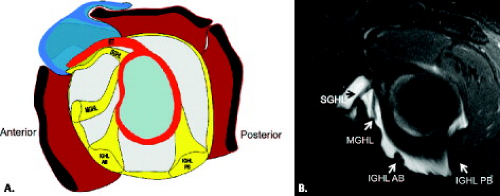
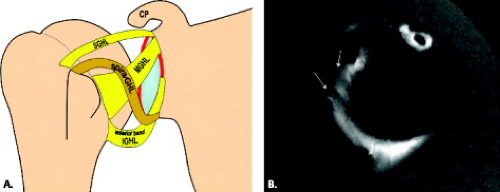
The superior, middle, and inferior glenohumeral ligaments (Fig. 5.13) and the coracohumeral ligament contribute to shoulder stability. Besides serving as static stabilizers, the ligaments can stabilize a joint by proprioception, providing neurologic feedback that senses position and affects muscular reflexes (35). When injured, these proprioceptive mechanisms can be disturbed, but they can be restored after shoulder reconstruction.
Two ligaments are located at the top of the joint in the rotator interval. These are the coracohumeral ligament (CHL) and superior glenohumeral ligament (SGHL). The CHL and SGHL ligaments limit inferior translation and external rotation of the adducted shoulder as well as posterior translation of the flexed, adducted, and internally rotated shoulder. The CHL originates on the lateral surface of the base of the coracoid process and inserts on the lesser and greater tuberosities, crossing the bicipital groove. The pectoralis minor tendon may insert on the coracohumeral ligament. The CHL is an extra-articular bursal-sided structure that is not seen during arthroscopy. It joins with the SGHL ligament laterally, forming a sling around the intra-articular portion of the biceps tendon in the rotator interval. The SGHL originates from the labrum, biceps tendon, or in common with the middle glenohumeral ligament in the region of the superior glenoid tubercle. It inserts into the fovea capitis line just superior to the lesser tuberosity of the humerus. It lies parallel to the lateral aspect of the coracoid process and is present in more than 90% of cases (36). It restrains external rotation below 60 degrees of abduction and limits inferior subluxation.
The middle glenohumeral ligament (MGHL) has a variable origin from the glenoid, scapula, anterior–superior labrum, biceps tendon, inferior glenohumeral ligament (IGHL), or superior glenohumeral ligament (37). It merges with the anterior capsule along the subscapularis muscle and tendon, continuing with the subscapularis tendon to the anterior aspect of the proximal humerus just below the attachment of the SGHL on the lesser tuberosity. It is the most variable of the ligaments as delineated in the next section. The position of the MGHL will vary with the degree of rotation of the glenohumeral joint. In external rotation, it becomes stretched and blends with the capsule. In internal rotation, the ligament becomes redundant and moves medially, anterior to the scapular neck. The MGHL limits anterior translation of the humeral head when the arm is abducted between 60 and 90 degrees (38, 39). The MGHL can be absent in up to 27% of individuals, and in those cases, large communication can be seen between the joint and the subscapular recess (38, 40, 41).
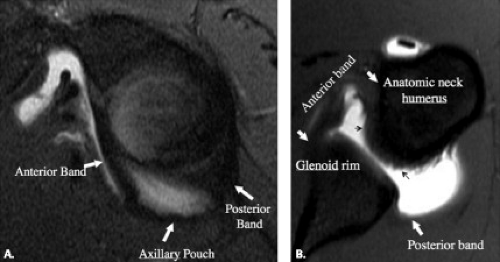
The IGHL, considered the most important stabilizer of the glenohumeral joint, is a complex that originates at the mid- to inferior portion of the anterior glenoid labrum. It drapes for a variable distance from anterior to posterior and inserts on the anatomic neck of the humerus. This ligament is usually inseparable from the labrum, forming a labroligamentous complex. It is composed of strong collagenous thickenings at its anterior and posterior margins—the anterior and posterior bands—joined by a fibrous thickening of the capsule
called the axillary pouch or recess. The anterior band of the IGHL reinforces the anterior capsule between the subscapularis muscle and the inferior aspect of the glenoid at or near the origin of the long head of the triceps.
called the axillary pouch or recess. The anterior band of the IGHL reinforces the anterior capsule between the subscapularis muscle and the inferior aspect of the glenoid at or near the origin of the long head of the triceps.
The posterior band of the IGHL is less consistent than the anterior band and axillary pouch (42). It is also the thinnest part of the inferior glenohumeral ligament and guards against posterior subluxation of the humeral head. The posterior band arises from the 7 o’clock to 9 o’clock position of the glenoid rim. The IGHL functions as a sling to support the humeral head and prevents abnormal translation of the humeral head on the glenoid. The IGHL is a major stabilizer of the joint in 90 degrees of abduction and full external rotation, limiting anterior rotation, and is lax when the shoulder is adducted. With internal rotation, the complex moves posteriorly and limits posterior translation. On MRI, the glenohumeral ligaments are best assessed in the presence of capsular distension, which is produced if there is a large amount of joint fluid or contrast in the shoulder joint (22, 37, 43, 44). The addition of ABER or ADIR postioning optimizes visualization of portions of the anterior–inferior labroligamentous complex, including the anterior labrum and inferior glenohumeral ligament (32, 45, 46).
The CHL can be seen on coronal and axial MR images extending anteriorly across the rotator interval between the coracoid and the humerus (Fig. 5.14). The SGHL is best seen on axial images obtained directly beneath or adjacent to the origin of the long head of the biceps tendon at the level of the coracoid (Fig. 5.13). The SGHL lies just lateral and parallel to the coracoid and is located in the rotator interval, just underneath the extra-articular coracohumeral ligament. The SGHL is usually thin, but it can become thick in the presence of an absent or underdeveloped MGHL (47).
The MGHL is usually seen as a round or linear low-signal–intensity structure between the anterior labrum and the subscapularis muscle on axial images as it takes an oblique course from the glenoid to the subscapularis. It forms a linear band in front of the glenoid on oblique sagittal images (Fig. 5.15).
The components of the IGHL are well seen with MRI (Fig. 5.16). The anterior band extends across the anterior inferior aspect of the joint, forming a “U” shape between the glenoid and humerus on coronal and axial images (Figs. 5.16 and 5.17). The anterior band extends inferiorly from the inferior labrum in the front of the joint on sagittal MR images (Fig. 5.14). The axillary pouch forms the inferior aspect of the hammock of the IGHL ligaments on all imaging sequences. Its attachment to the humerus forms a jagged appearance on axial MR images (Fig. 5.16). The posterior band usually merges with the posterior capsule on coronal and axial images and is seen as a posterior linear structure on sagittal images. Occasionally, it presents as a small, round structure in the posterior capsule.
A new extra-articular anterior glenohumeral ligament has been described called the spiral ligament (48). It is also known as the “fasciculus obliquus.” This ligament is located in the anterior shoulder capsule and extends from the axillary component of the IGHL and the infraglenoid tubercle to the MGHL superiorly in a spiral pattern (Fig. 5.18). The clinical importance of this ligament is not known.
The glenohumeral joint capsule extends from the glenoid rim to the humeral neck. Three types of anterior capsular insertions have been described. These include type 1, which inserts into the glenoid rim; type 2, which inserts into the scapular neck; and type 3, which inserts further medially into the scapula (Fig. 5.19). Although a lax type 3 capsule may predispose to instability or can be the result of instability (capsular stripping), many shoulders with this configuration have no instability. The degree of medial capsular attachment can also vary with the amount of capsular distention by effusion or contrast as well as the position of the shoulder. The anterior capsule is redundant in internal rotation and tightens up with external rotation. The posterior capsule should always insert on the glenoid rim (Fig. 5.19), although it may be redundant in its course behind the scapula. Internal rotation will tighten the posterior capsule and external rotation will make it lax, but it should normally insert on the glenoid rim in either case. If it attaches medial to the rim, it is stripped and posterior instability should be considered.
The rotator interval, also discussed in other shoulder chapters in this book, is a triangular-shaped area marked by the anterior border of the supraspinatus tendon superiorly, the subscapularis tendon inferiorly, and the coracoid base laterally. The rotator interval capsule is reinforced superiorly by the coracohumeral ligament and the superior glenohumeral ligament. These two ligaments merge laterally at the superior margin of the bicipital groove to form a pulley around the tendon of the long head of the biceps (Fig. 5.20). The rotator interval plays a significant role in glenohumeral stability (49). The function of the rotator interval is to limit inferior
translation of the glenohumeral joint in the adducted shoulder and to provide stability against posterior dislocation in flexion or abduction–external rotation. It also limits the range of flexion, extension, adduction, and external rotation.
translation of the glenohumeral joint in the adducted shoulder and to provide stability against posterior dislocation in flexion or abduction–external rotation. It also limits the range of flexion, extension, adduction, and external rotation.
Normal Variations in the Capsulolabral Structures
Normal variations of the capsulolabral complex are often seen and can be mistaken for pathologic lesions (50). These normal variants are seen in the superior and anterior–superior aspects of the glenoid. Superior labral normal variants and their distinction from SLAP lesions are covered elsewhere in this book.
The normal labral variants in the anterior–superior region of the glenoid include the Buford complex and the sublabral foramen or hole. These can be confused with labral tears by those who are not aware of their existence. In distinguishing these normal variants from labral tears, it is helpful to know that isolated tears are uncommon in the anterior–superior segment of the labrum. Usually tears in the anterior–superior region of the glenoid are associated with SLAP lesions or tears that extend down to the anterior–inferior labrum.
Absence of the anterior–superior labrum associated with a rounder and larger “cord-like” MGHL may be congenital, and this has been termed the Buford complex (Fig. 5.21). This variant of normal is seen in up to 6% of shoulder arthroscopies (50–52). The cord-like MGHL originates from the superior labrum anterior to the biceps and can be differentiated from a labral tear by following it on consecutive axial images from its origin to its confluence with the anterior joint capsule and subscapularis tendon. It can also be seen on the oblique
sagittal images as a band in front of the glenoid (Fig. 5.21). An increased association of the Buford complex with SLAP lesions has been shown (53).
sagittal images as a band in front of the glenoid (Fig. 5.21). An increased association of the Buford complex with SLAP lesions has been shown (53).
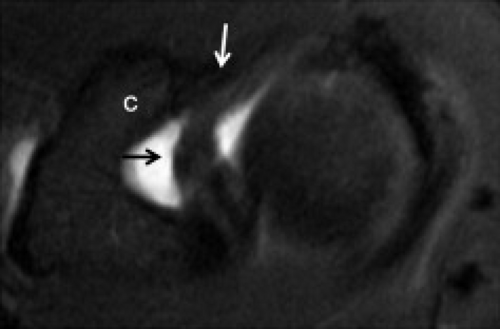
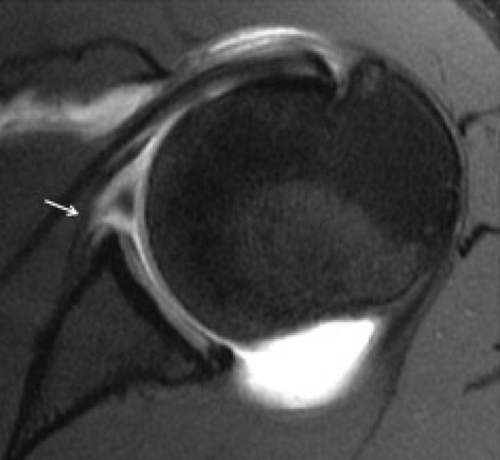
Another labral variant seen in 11% to 15% of shoulders in the anterior–superior region of the glenoid labrum is the sublabral foramen or hole (50) (Fig. 5.22). The foramen occurs when the anterior–superior portion of the labrum is not attached to the glenoid rim. There may be an associated small osseous indentation along the anterior border of the glenoid fossa. This foramen or hole can be associated with a “cord-like” MGHL in 75% of cases (50). One should not mistake the “cord-like” middle glenohumeral ligament for a labral detachment. The attachment of the sublabral foramen to the anterior–inferior labrum near the midportion of the anterior glenoid is termed the “labral slip.” Infrequently, both the Buford complex and the sublabral foramen can extend into the anterior–inferior portion of the labrum (54). In addition, it is interesting to note that a sublabral foramen may coexist with a superior sublabral recess.
The sublabral recess, discussed more completely in the chapter on SLAP lesions, is a normal recess that can exist between the superior labrum and the glenoid articular cartilage (44, 55, 56) (Fig. 5.23). This anatomic variant is smooth, 1 to 2 mm in width, and does not extend to the top of the labrum. It is not associated with a perilabral cyst as are some superior labral tears. Although many have written that this recess does not extend posterior to the long head of the biceps attachment to the superior labrum (47), it has been our experience and that of others that this recess can do so in the absence of a tear (57).
The MGHL may have some interesting variants that simulate pathology. Absence of the MGHL is a congenital variant with no associated pathology, seen in approximately a third of shoulders. The absent MGHL is associated with a prominent subscapular recess. In that situation, the inferior glenohumeral ligament may be
larger and originate more superiorly. The MGHL may be attenuated or thin in 5% and more rounded and cord-like in 19% of cases. A filamentous structure may bridge the gap between the anterior labrum and the cord-like MGHL. Occasionally, a variant in the form of a duplicate MGHL with a longitudinal split may be seen (37) (Fig. 5.24). It is difficult to distinguish this variant from a longitudinal tear. Some shoulders contain a combined MGHL and IGHL and, rarely, a glenohumeral joint may be devoid of glenohumeral ligaments.
larger and originate more superiorly. The MGHL may be attenuated or thin in 5% and more rounded and cord-like in 19% of cases. A filamentous structure may bridge the gap between the anterior labrum and the cord-like MGHL. Occasionally, a variant in the form of a duplicate MGHL with a longitudinal split may be seen (37) (Fig. 5.24). It is difficult to distinguish this variant from a longitudinal tear. Some shoulders contain a combined MGHL and IGHL and, rarely, a glenohumeral joint may be devoid of glenohumeral ligaments.
The anterior band of the IGHL may be congenitally prominent and extend above the equator of the glenoid, even to the bicipitolabral complex at the superior labrum. The anterior–superior labrum is attenuated or absent in this setting. In addition, a cord-like MGHL may be seen in some of these prominent IGHL cases.
The “magic angle” phenomenon has been seen in the posterior superior labrum similar to tendons, ligaments, and cartilage (58, 59). This occurs when the organized collagen of the labrum lies at an angle 55 ± 10 degrees to the main magnetic field B0. The magic angle phenomenon produces intermediate signal intensity in the labrum that must be distinguished from a tear.
Labral Pathology
Tears of the labrum are common in athletes with instability, especially those participating in sports that require forceful and repetitive abduction and overhead rotation of the humerus. Tears can also be seen after routine or repetitive trauma, microtrauma as well as and with aging and degeneration.
Degenerative lesions present with fraying and attenuation of the labrum. There can be signal intensity changes as well. The transitional zone between the labrum and the articular cartilage may have areas of intermediate signal intensity beneath the labrum (60). Fibrovascular tissue, eosinophilic or mucoid degeneration, synovialization, calcification, ossification, or combinations of these tissue types can be seen with labral degeneration and lead to alterations in morphology and signal intensity of the labrum (60).
When describing a labral tear, it is best to mention the location(s) of the tear on the glenoid rim as described in the normal labral anatomy section of this chapter. Morphologic criteria such as absence, fraying, detachment, displacement, fragmentation, or deformity are used to describe labral pathology. Fluid or contrast within the labral substance or at the interface between the labrum and the bone/cartilage substance (if not one of the described normal variants) is also a good indication of a labral tear.
The torn labrum may be unstable with a flap component with an attached piece separated from the main structure or the labrum can have a vertical split, which, if complete, is called a bucket handle tear. Both of these types of labral tears cause mechanical symptoms such as locking, catching, clicking, and popping and are treated with surgical resection or repair.
Anterior Instability
Labral Lesions Associated With Anterior Instability
The anterior–inferior labrum is the most frequently affected site of labral pathology related to anterior instability. Injury to the anterior–inferior labrum may demonstrate findings mentioned for routine tears of the labrum, but often reach predictable patterns in the form of a Bankart lesion or its variants—the anterior labroligamentous periosteal sleeve avulsion (ALPSA) or Perthes lesion. Sometimes one may see that these lesions change with time. For example, a Perthes lesion may turn into a Bankart or ALPSA lesion. Some surgeons believe that differentiating these lesions is important for proper management, whereas others do not. To serve all of the referring physicians, we make a point of differentiating them or at least describing the distinctions between the Bankart lesion and its variants. What is important is that these labral tears are associated with inferior glenohumeral ligament complex pathology and that the entire labroligamentous complex is involved in the instability and needs to be treated with attention to the labrum and the anterior band of the inferior glenohumeral ligament.
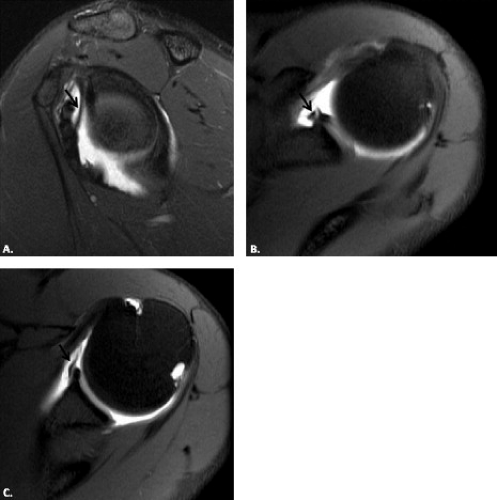
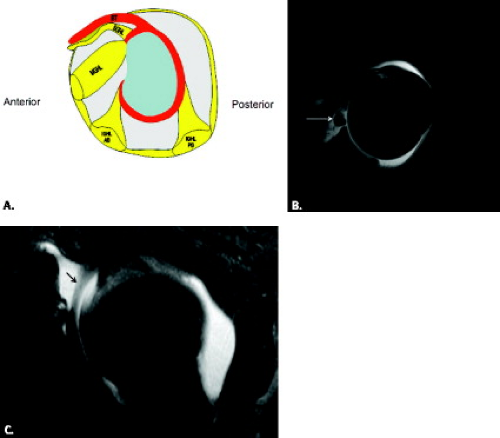
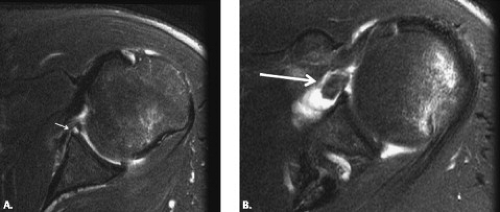
The most common lesion resulting from an anterior dislocation is the Bankart lesion. This represents a detachment of the anteroinferior labrum and glenohumeral
ligament from the glenoid rim (Figs. 5.25 and 5.26). The avulsed labrum is no longer attached to the scapular periosteum. The labrum may be hemorrhagic, fragmented, or pulled away from the glenoid. The detached labrum may float upward in the joint, producing a glenoid labrum ovoid mass (GLOM sign) (Fig. 5.27). The rounded low-signal–intensity labrum that makes the GLOM lies in the region of the coracoid and can simulate a dislocated biceps tendon, intra-articular body, cord-like MGHL, combined MGHL and IGHL, SLAP lesion, or air bubble, so it is important to visualize the Bankart defect inferiorly to make the correct diagnosis.
ligament from the glenoid rim (Figs. 5.25 and 5.26). The avulsed labrum is no longer attached to the scapular periosteum. The labrum may be hemorrhagic, fragmented, or pulled away from the glenoid. The detached labrum may float upward in the joint, producing a glenoid labrum ovoid mass (GLOM sign) (Fig. 5.27). The rounded low-signal–intensity labrum that makes the GLOM lies in the region of the coracoid and can simulate a dislocated biceps tendon, intra-articular body, cord-like MGHL, combined MGHL and IGHL, SLAP lesion, or air bubble, so it is important to visualize the Bankart defect inferiorly to make the correct diagnosis.
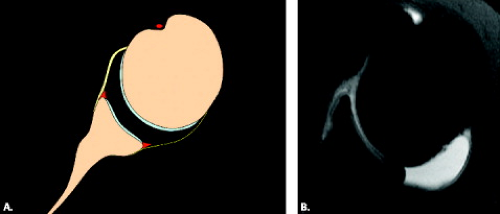
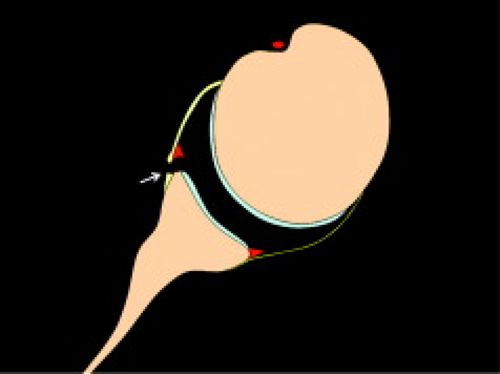 Figure 5.25 Diagram of the Bankart lesion in the axial plane. The anterior–inferior labrum displaces from the glenoid rim and the scapular periosteum is disrupted. |
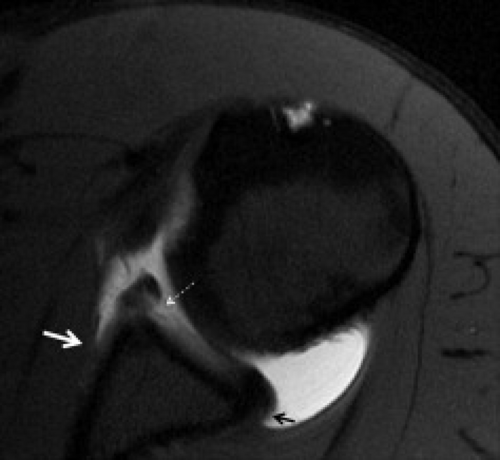
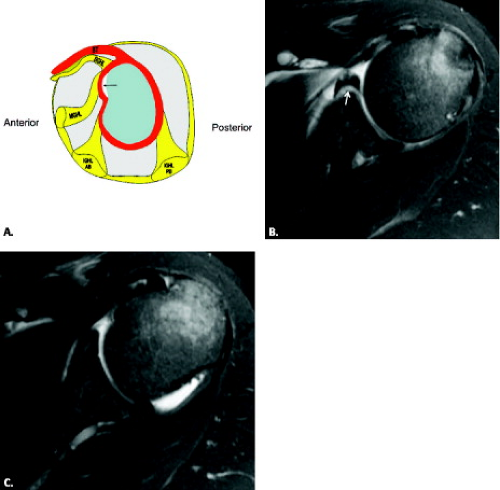
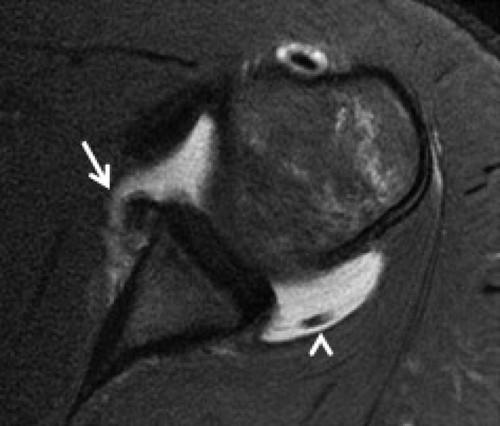
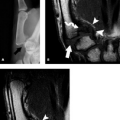
Neviaser (61) described a variant of the Bankart lesion known as the ALPSA lesion (61) (Figs. 5.28–5.30). This represents an avulsion of the inferior glenohumeral ligament complex from the anterior–inferior glenoid with an intact periosteum. The avulsed anterior–inferior labrum displaces medially and rotates inferiorly along the denuded anterior scapular neck. These lesions eventually heal in this medially displaced position, leading to recurrent anterior instability because of persistent incompetence of the inferior glenohumeral ligament labral complex. With time, the detached labrum and glenohumeral ligament become synovialized and enlarge, creating a chronic mass lesion in that location (Fig. 5.31). This lesion has the best surgical outcome when it is dissected from the scapular neck and repaired laterally to the level of the glenoid rim. ALPSA lesions can also involve the inferior labrum near the 6 o’clock location.
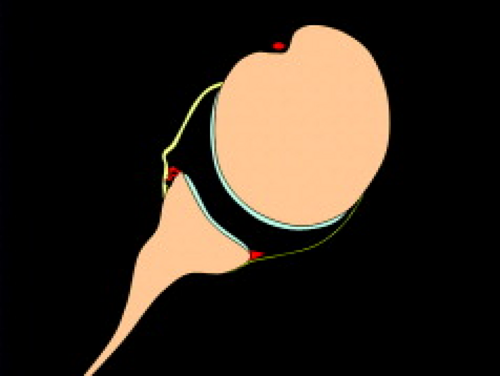 Figure 5.28 Anterior labroligamentous periosteal sleeve avulsion (ALSPA lesion). This diagram shows the inferomedial displacement of the labrum, which is still attached to scapular periosteum. |
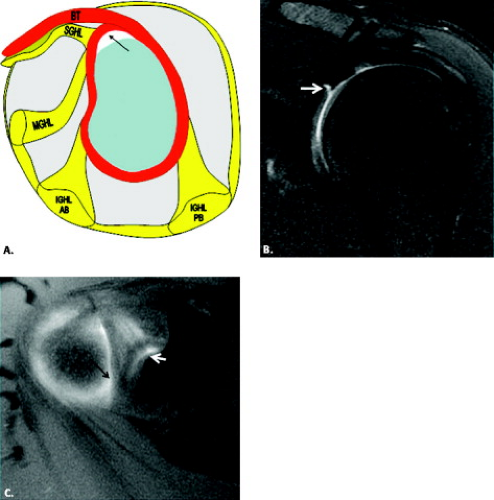
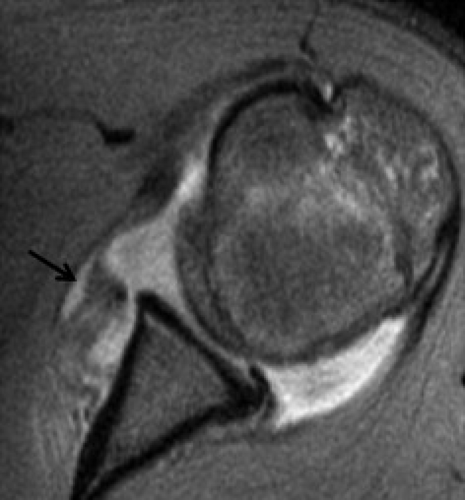
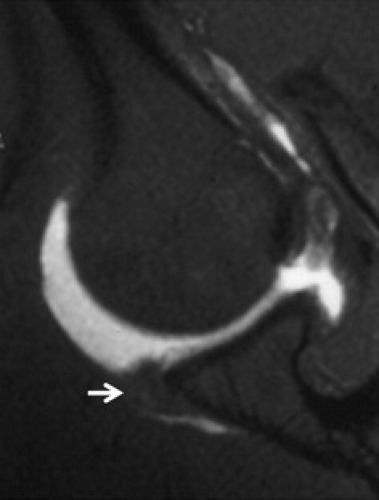
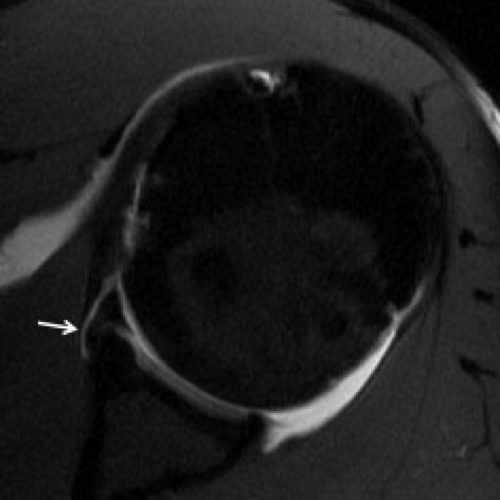
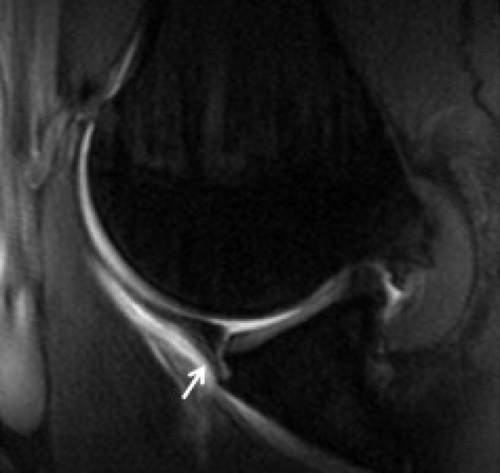
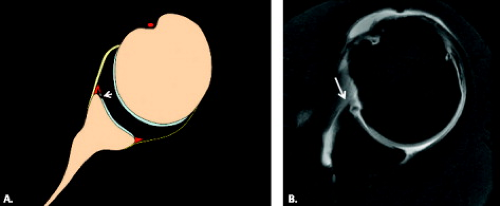
The third variant in this location is termed the Perthes lesion, named after a German physician who described it in the early 1900s (62). This lesion is an
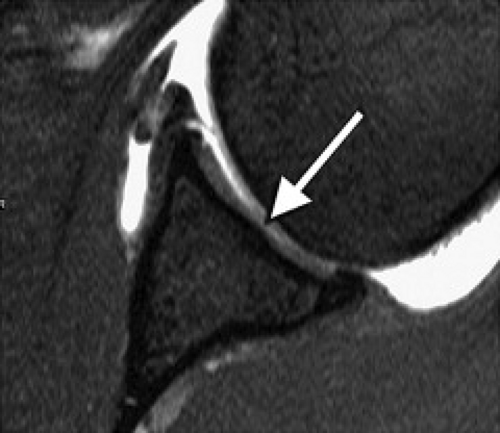
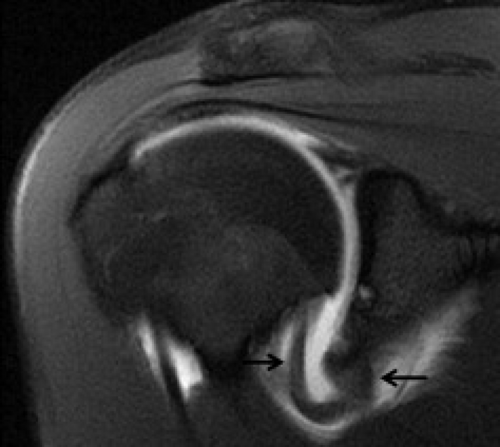
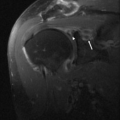
avulsion of the anterior–inferior labrum and IGHL with an intact scapular periosteum that connects to the IGHL but is stripped from the glenoid (Figs. 5.32 and 5.33). The Perthes lesion is not as easily identified on MR arthrography as the other Bankart-type lesions (19), but it is well visualized with the addition of ABER positioning of the shoulder (Fig. 5.34).
avulsion of the anterior–inferior labrum and IGHL with an intact scapular periosteum that connects to the IGHL but is stripped from the glenoid (Figs. 5.32 and 5.33). The Perthes lesion is not as easily identified on MR arthrography as the other Bankart-type lesions (19), but it is well visualized with the addition of ABER positioning of the shoulder (Fig. 5.34).
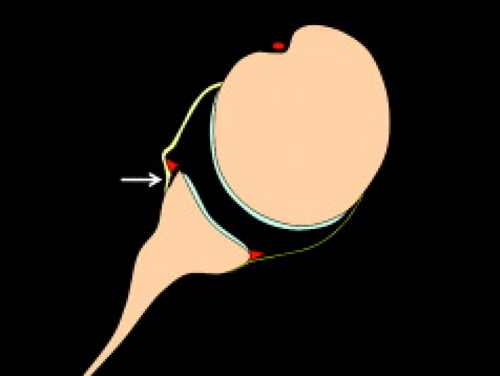 Figure 5.32 Perthes lesion. A Bankart variant in which the anterior–inferior labrum is detached from the glenoid but still attached to scapular periosteum (arrow). |
Occasionally related to instability, but more often caused by forced adduction injury to the shoulder with the arm in abduction and external rotation, a glenolabral articular disruption (GLAD) lesion is a nondisplaced superficial tear of the anterior–inferior labrum that is accompanied by fibrillation and erosion of the adjacent articular cartilage (63, 64) (Fig. 5.35). Because the anterior fibers of the IGHL are not disrupted and the labrum is not displaced, the GLAD lesion does not predispose to anterior instability. The GLAD lesion can progress to rapid degenerative joint disease and intra-articular bodies. GLAD lesions are treated with arthroscopic débridement of the labrum and chondral injury without the need for a stabilization procedure (64).
Glenohumeral Ligament and Capsular Lesions Associated With Anterior Instability
The anterior–inferior and inferior portions of the shoulder capsule may be enlarged in up to 19% of shoulders with recurrent anterior dislocation (65




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree