CHAPTER 1 MRI of the Head and Neck
Important considerations for scan acquisition
Scan Considerations
• Refer to all vendor specific safety parameters.
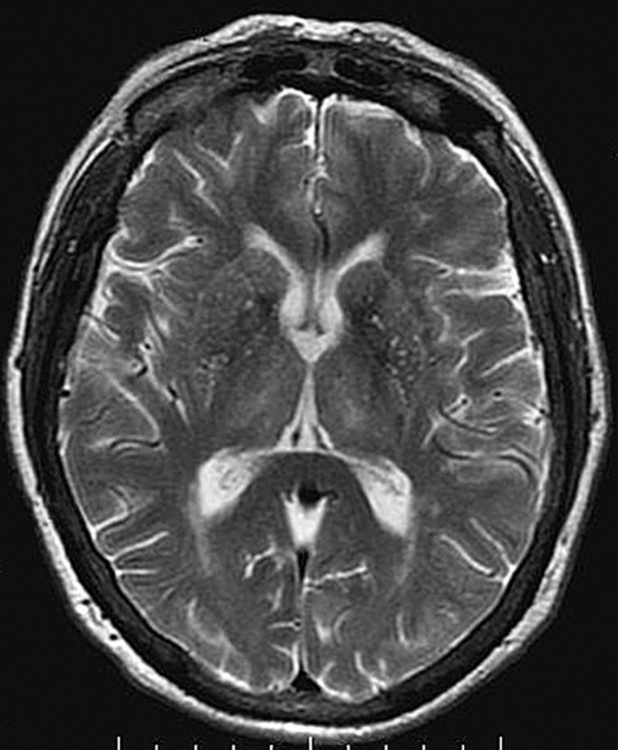
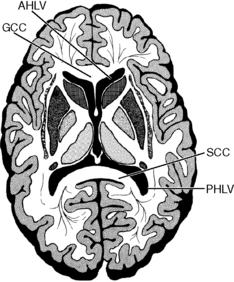
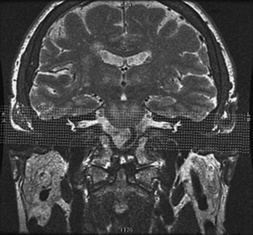
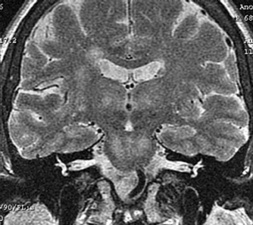
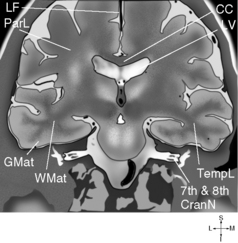
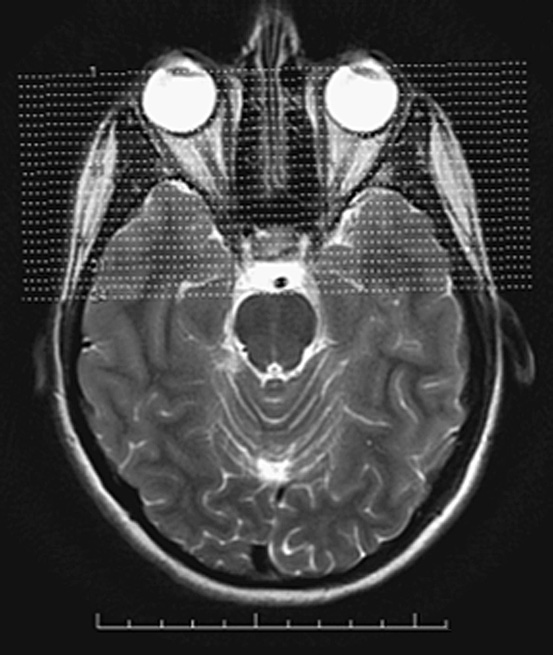
• When scanning the brain, the most advantageous scan plane to cover the entire brain is the axial. Axial scans of the brain should be acquired with slices angled parallel to the genu and splenium of the corpus callosum. This enables duplication for subsequent exams of the brain.
• Be consistent when prescribing scans, i.e., put all axial slices in identical positions for each scan so the radiologist can compare one sequence with another.
• Learn to compare the hemispheres of the brain to identify pathology, paying close attention to symmetry.
• When contrast of the brain is indicated, allow adequate time before scanning. Contrast enhancement can take several minutes for maximum visualization. Today’s sequences are very short and scanning too quickly after the injection will cause loss of contrast effectiveness. A radiologist may perform the T2 fluid-attenuated inversion recovery (FLAIR) or another pulse sequence after contrast to wait for the gadolinium to become more effective. Others wait a few minutes and then scan the coronal and sagittal before the axial scan. Other methods may be used as well.
Coils
• A multi-channel HD head coil or multi channel HNS (head, neck, spine) coil is recommended.
• A head or neurovascular coil can be used when necessary, i.e., some patients cannot fit in the multi-channel HD head coil.
• All multi-channel coils produce excessive signal adjacent to the coil. This can be compensated for by using vendor-specific coil intensity correction options to provide uniform signal intensity.
Pulse Sequences
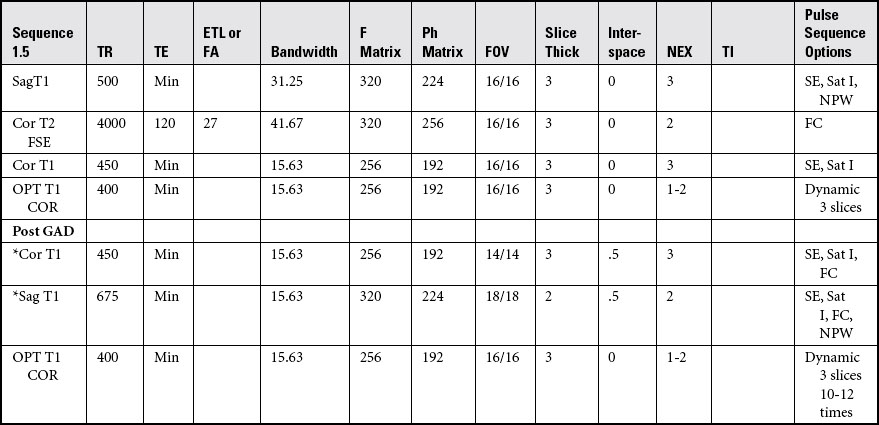
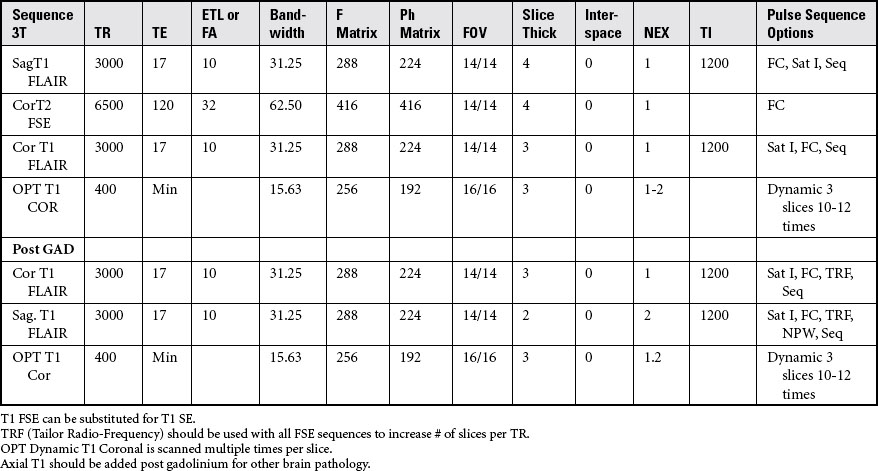
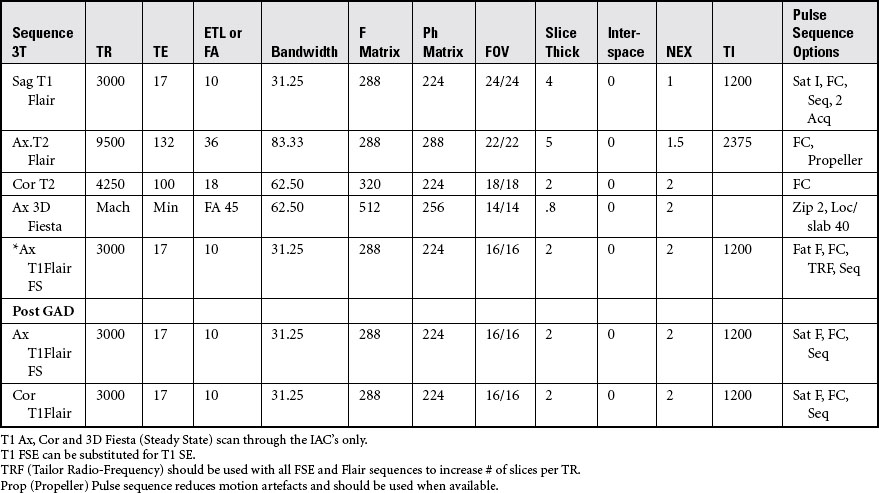
• At 3T, T1 FLAIR is substituted for T1 spin echo (SE) or fast spin echo (FSE), to compensate for long T1 relaxation times at 3T.
• T1 FLAIR best differentiates gray and white mater details of the brain at 3T.
• T1 spin echo and fast spin echo, and T1 FLAIR imaging is used to best identify anatomical structure, whereas T2 and T2 FLAIR imaging provide detailed evidence of pathology.
• On T1 FLAIR and T1 sequences, cerebrospinal fluid (CSF) produces dark or hypo-intense signal. T1 FLAIR uses an inversion pulse to produce dark or hypo-intense signal.
• On T2 sequences, CSF produces bright or hyper-intense signal. T2 FLAIR uses an inversion pulse to produce dark or hypo-intense CSF signal, whereas all other abnormal fluid appears bright.
• BRAVO (BRAin VOlume imaging) are high resolution sub-millimeter isotropic T1 SPGR sequences that use an IR pulse to obtain superior gray/white matter differentiation. These can be acquired in any plane and reformatted.
• IDEAL (GE) is a fat/water separation technique (previously called 3-point Dixon technique) that can also be used to eliminate fat or water from the image. A “water image” eliminates fat; a “fat image” eliminates water. An “in-phase image” can resemble either T1, T2, and SPGR sequences. IDEAL performs all of these options in one acquisition. Applications include orbits, pituitary, and IACs.
• CUBE (GE) is an isotropic T2 or T2 FLAIR imaging option with sub-millimeter slices and isotropic pixels, which are acquired in the sagittal or coronal plain. These isotropic images can be reformatted into other planes post acquisition. For MS of the brain, the sagittal plane is performed and reformats are acquired in the axial and coronal plane.
• Two-dimensional SWI and three-dimensional SWAN are “susceptibility-weighted imaging,” which are more susceptible to blood and or blood vessels. These may replace routine GRE imaging for blood or trauma. They should be reformatted in the axial plane, with minimal rendering, to increase visualization of vessels and blood products.
• Contrast is predominantly used with T1 FSE, T1 FLAIR, BRAVO, and other T1 SPGR sequences because it shortens the T1 relaxation rate and T1 effects are maximized.
• MRA (magnetic resonance angiography) are spoiled gradient and gradient echo sequences that suppress background tissue while enhancing vascular structures by using low TR, low TE, and low flip angles (FA). Saturation bands are used to distinguish between arteries and veins. Above the heart, superior (S) sat bands visualize arteries and inferior (I) sat bands visualize veins. For suspected dissection, always add an axial T1 fat-saturated sequence.
• TOF (time of flight) sequences are 2D or 3D imaging techniques that rely primarily on flow-related enhancement to distinguish moving spins from stationary tissue. Blood that flows into the slice will not have experienced RF pulses saturation and will therefore appear much brighter than stationary tissue.
• PC (phase contrast) imaging sequences use gradient directions and flow Velocity ENCoding (VENC) to visualize arteries and veins based on their speed of flow in cm/sec. Because stationary tissue does not move, it is automatically suppressed. Vessels are always flowing so they are bright on phase contrast scans. Veins flow slower then arteries at approximately 15-20 cm/sec, whereas arteries flow at approx 50-70 cm/sec.
• Enhanced MRA and MRV are high-resolution PC sequences that can be used to replace TOF imaging. It has the ability to eliminate vascular susceptibility issues that occur with TOF sequences, because it uses the velocity of the flow instead of flow-related enhancement.
Options
• Inferior (I) saturation (sat) band can help to compensate for CSF and vascular pulsation. Vascular structures should have a flow void (appear dark) on T1 and T2 pulse sequences. Saturation bands can be used on all pulse sequences.
• Flow compensation (FC) or gradient nulling should be used on T2 images to help compensate for CSF flow and vascular motion. FC should never be used on T1 pre-contrast because it can cause vessels to appear bright and mimic pathology. It is often used post gadolinium (GAD) on T1 sequences to compensate for flow artefacts.
• Fat saturation (FS) options and terminology are vendor specific. For GE systems, use “fat classic” for fat saturation of the orbits and internal auditory canals.
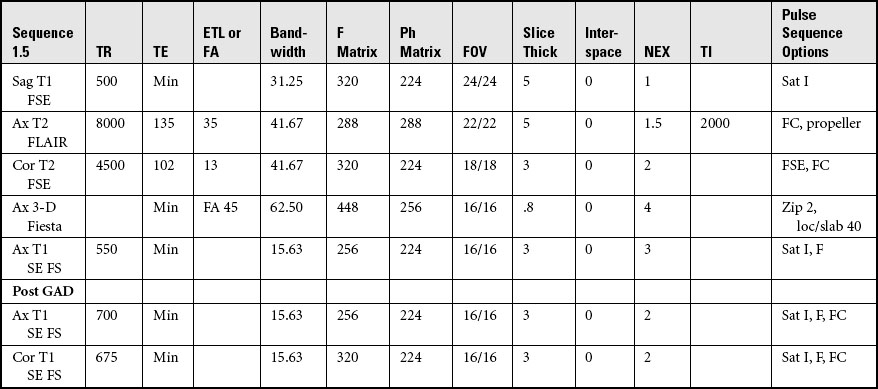
Routine brain scan
Acquire three-plane pilot per site specifications.
COIL: Multi-channel head or neurovascular*
POSITION: Supine, head first, cushion under knees
IMMOBILIZATION: Secure head with sponges. Shield patient from touching sides of magnet
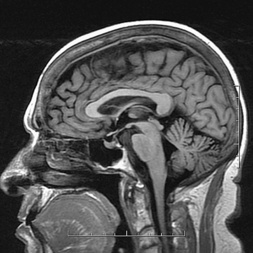
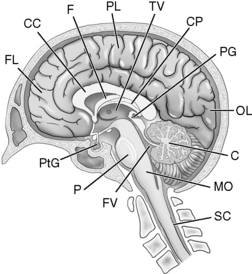
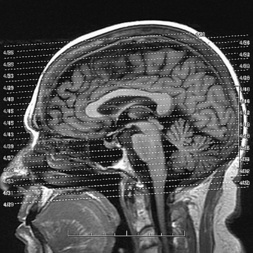
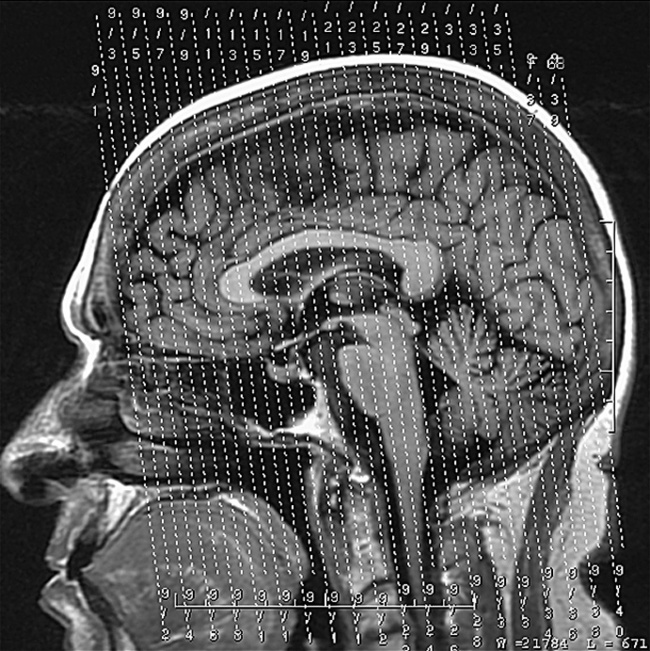
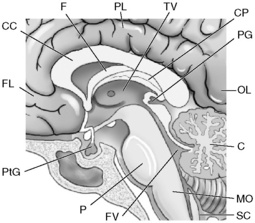
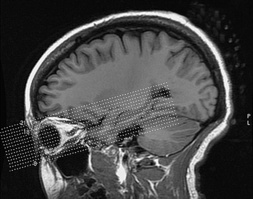
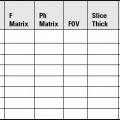
Acquisition of Sagittal Images of the Brain
SLICE ACQUISITION: Plot left to right covering both temporal margins
SLICE ALIGNMENT: Parallel to third ventricle and midsagittal fissure
ANATOMIC COVERAGE: C2 to convexity, anterior to posterior cranial margins
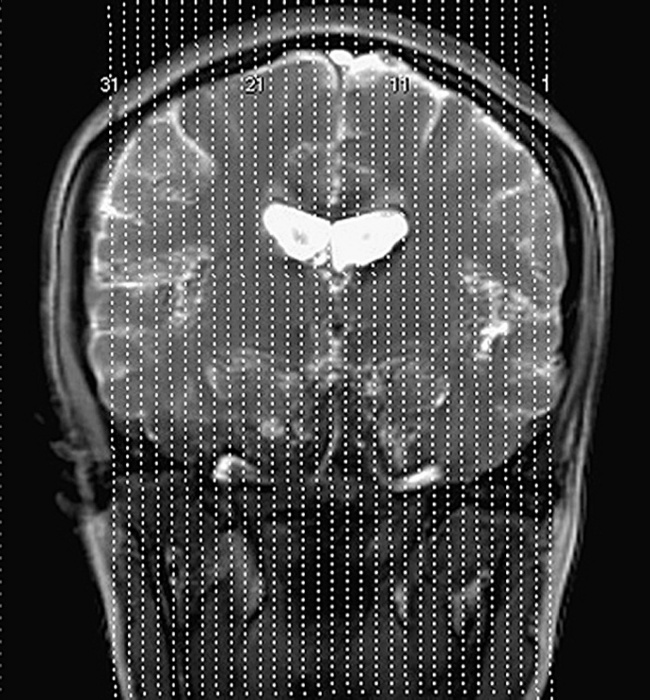
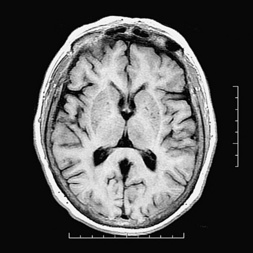
Acquisition of Axial Images of the Brain
Brain for pituitary
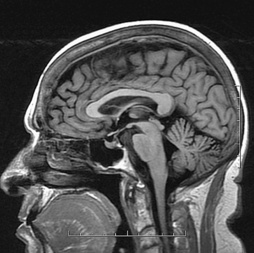
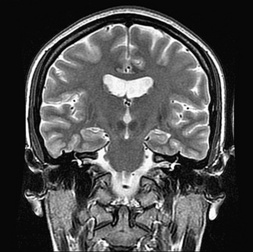
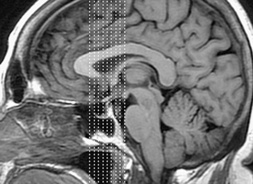
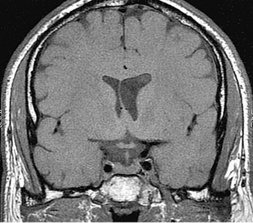
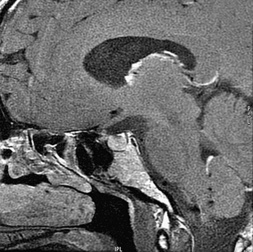
Acquire three plane pilot per site specifications (see Figs. 1-1 through 1-3).
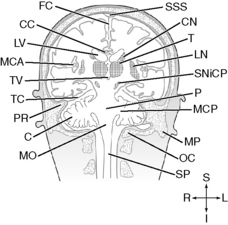
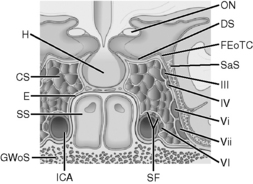
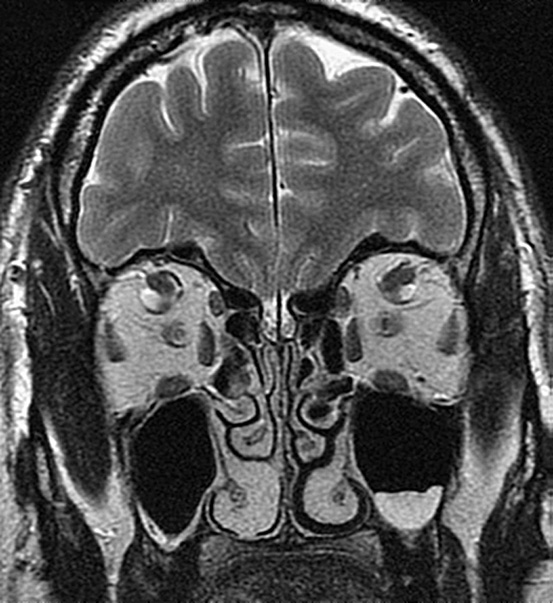
Acquisition of Coronal Images, Thin Slices Through Pituitary
SLICE ACQUISITION: Plot anterior to posterior
SLICE ALIGNMENT: Parallel to sella turcica
ANATOMIC COVERAGE: From anterior corpus callosum through pons, cerebellum to vertex
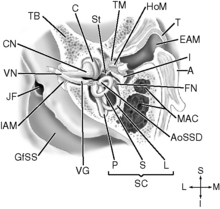
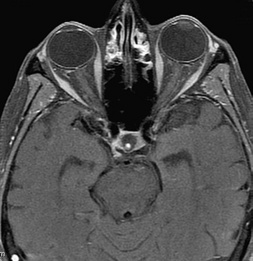
Brain for internal auditory canals (IACs)
Acquire three-plane pilot per site specifications (see Figs. 1-1 through 1-3).
Acquisition of Thin-Sliced Axial Images of the IACs
SLICE ACQUISITION: Plot inferior to superior
SLICE ALIGNMENT: Parallel to acoustic nerves
ANATOMICAL COVERAGE: From inferior to superior through bony mastoid region
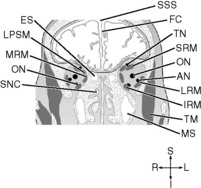
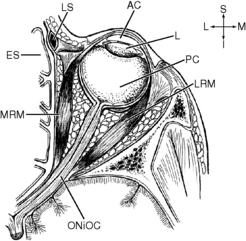
Brain for orbits—optic nerves
Acquire three-plane pilots per site specifications (see Figs. 1-1 through 1-3).