, Joungho Han2, Man Pyo Chung3 and Yeon Joo Jeong4
(1)
Department of Radiology Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(2)
Department of Pathology Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(3)
Department of Medicine Division of Pulmonary and Critical Care Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea, Republic of (South Korea)
(4)
Department of Radiology, Pusan National University Hospital, Busan, Korea, Republic of (South Korea)
Abstract
When the lesions of lung opacification appear with discrete margin, we call them multiple nodules or masses (please also note section “Patchy and Nodular Consolidation” in Chap. 3) (Figs. 19.1 and 19.2).
Definition
When the lesions of lung opacification appear with discrete margin, we call them multiple nodules or masses (please also note section “Patchy and Nodular Consolidation” in Chap. 3) (Figs. 19.1 and 19.2).
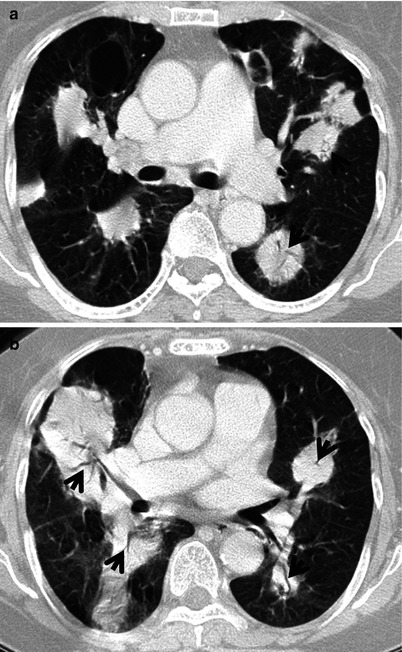
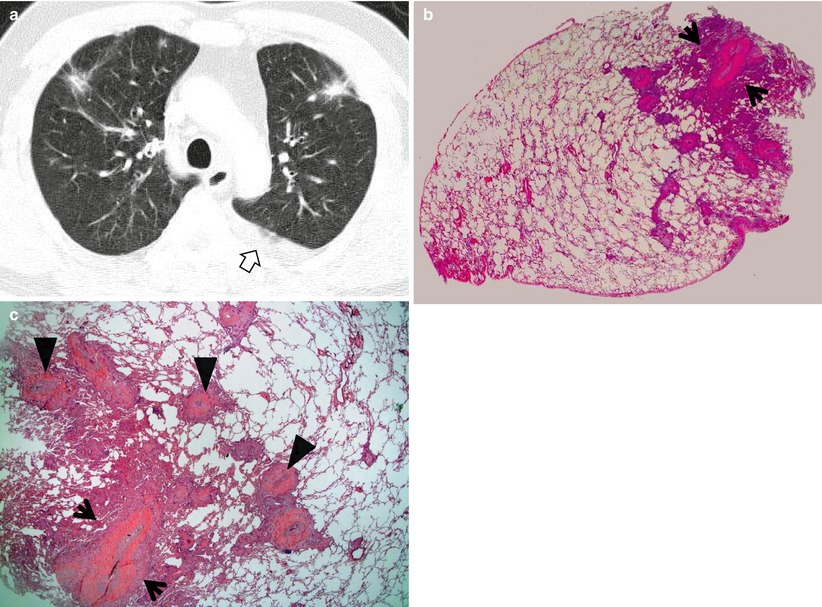
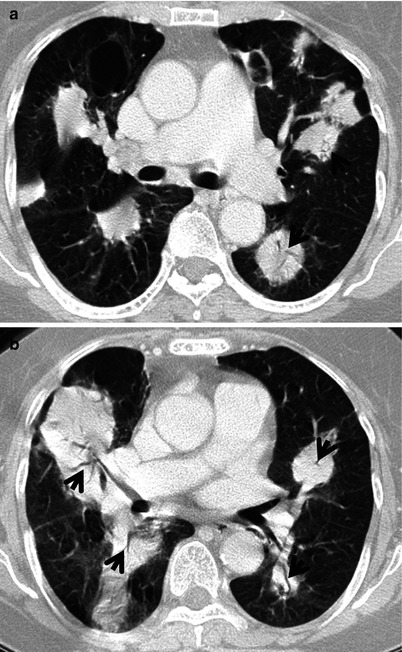
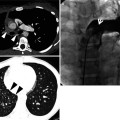
Fig. 19.1
Marginal zone B-cell lymphoma manifesting as multiple masses in both lungs in a 73-year-old woman. (a, b) Lung window images of CT scans (2.5-mm section thickness) obtained at levels of distal main bronchi (a) and right middle lobar bronchus (b), respectively, show multiple masses in both lungs. Mass contain internal CT air-bronchogram sign (arrows). Also note thin-walled air-filled cyst in bottom of right upper lobe. Histopathologic evaluation of ore biopsy obtained from a mass suggested extranodal marginal zone lymphoma or lymphoplasmacytic lymphoma
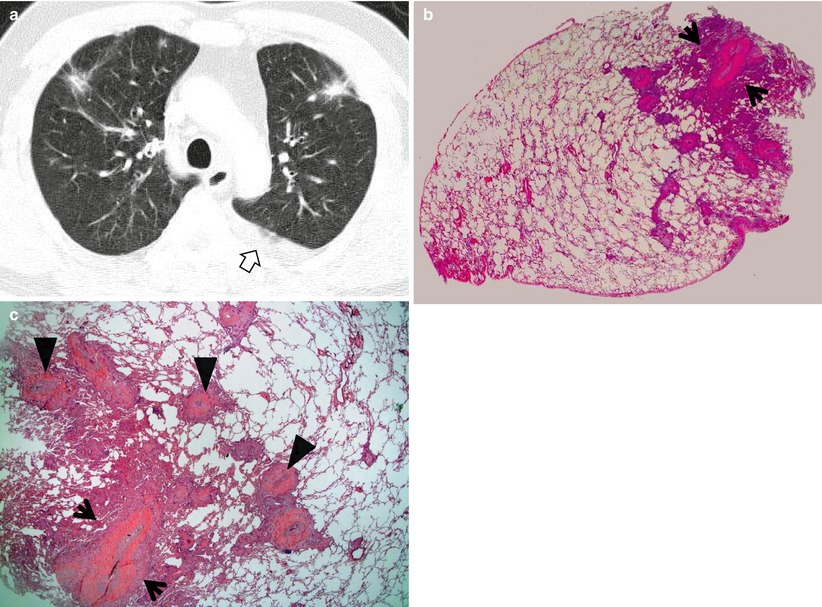
Fig. 19.2
Pulmonary metastases from a breast cancer in a 62-year-old man. (a) Lung window of CT scan (5.0-mm section thickness) obtained at level of aortic arch shows multiple variable-sized poorly defined nodules in both upper lobes. Also note left pleural effusion (open arrow). (b) Low-magnification (×40) photomicrograph of pathologic specimen obtained from right upper lobe with wedge resection demonstrates a predominant nodule (arrows) and surrounding malignant satellite nodules. (c) High-magnification (×100) photomicrograph discloses duct-forming adenocarcinoma (arrows) with lymphangitic tumor spread. Also note pulmonary arterial invasion (arrowheads)
Diseases Causing the Pattern
Pulmonary metastases (Fig. 19.2) are the most common cause of multiple nodules or masses. Lymphoproliferative diseases (Fig. 19.3), particularly in the secondary involvement of the lungs in Hodgkin lymphoma or non-Hodgkin lymphoma, may also manifest multiple nodules or masses [1]. Pulmonary epithelioid hemangioendothelioma (Fig. 19.4), which is a low- to intermediate-grade vascular neoplasm, can manifest multiple nodules. Rheumatoid nodules, amyloidomas (Fig. 19.5), sarcoidosis, pulmonary vasculitis including ANCA–associated granulomatous vasculitis (former Wegner’s granulomatosis) (Fig. 19.6), fungal infection (Fig. 19.7) or nocardiosis, and septic emboli are the benign inflammatory or infectious causes of multiple pulmonary nodules. Pulmonary Langerhans cell histiocytosis (eosinophilic granuloma) also manifests multiple variable-sized cavitating or noncavitating nodules with cystic lung lesions.
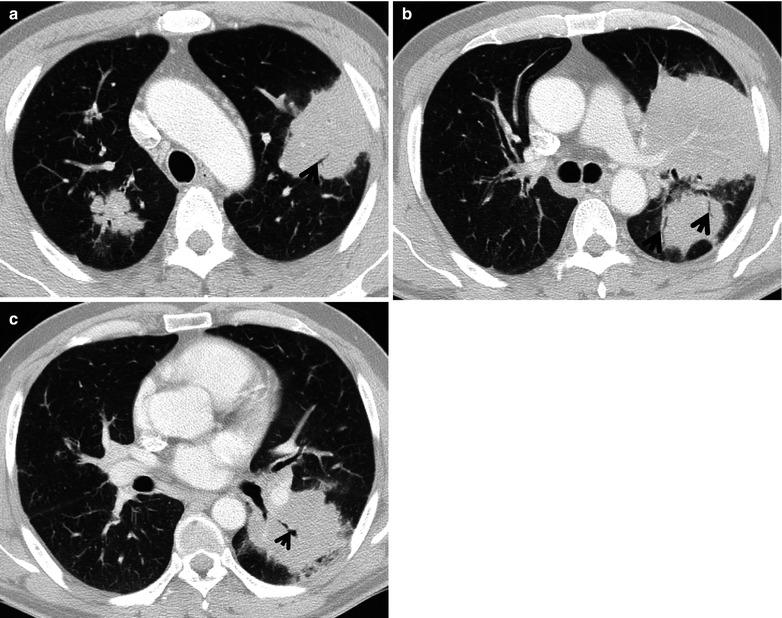
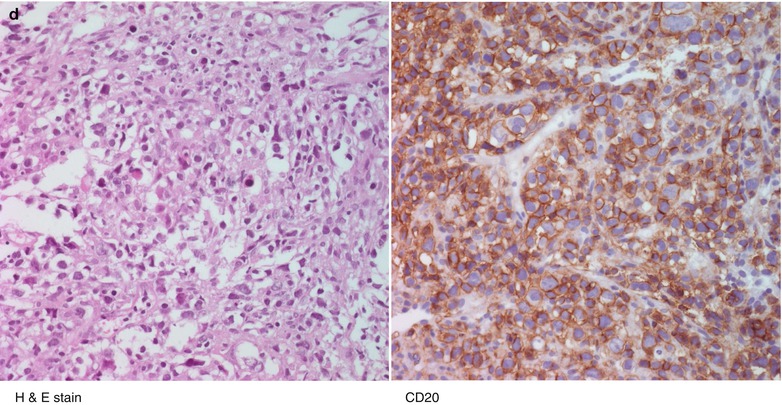
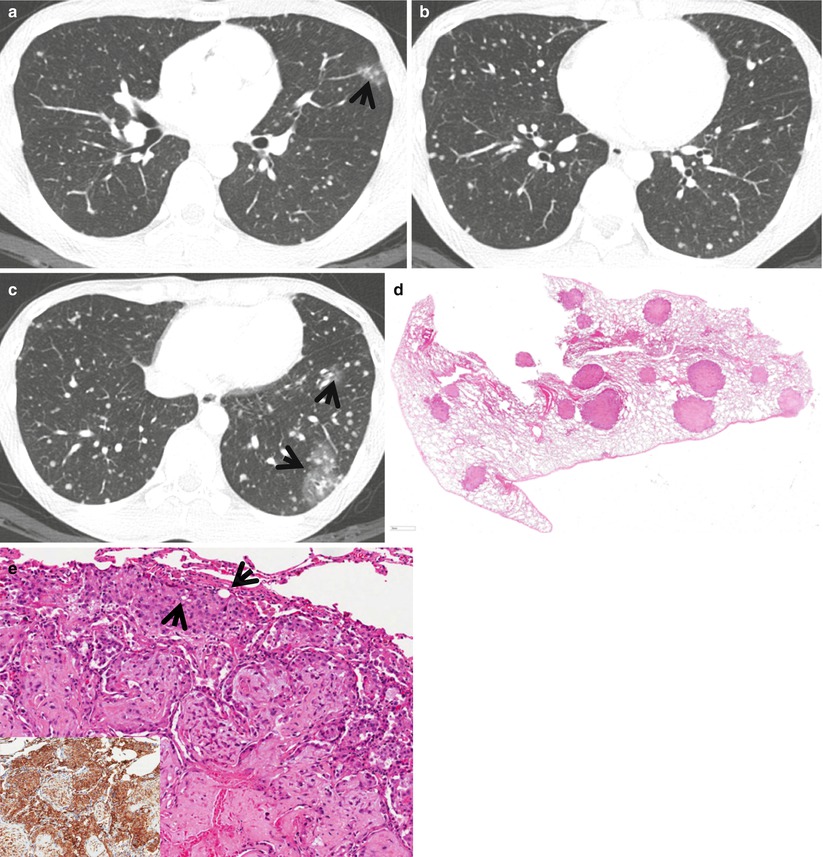
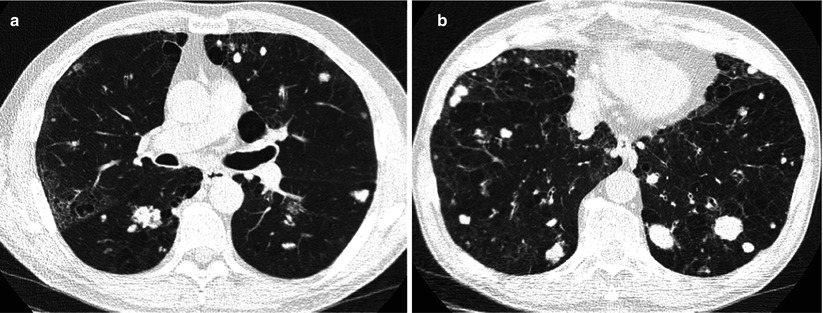
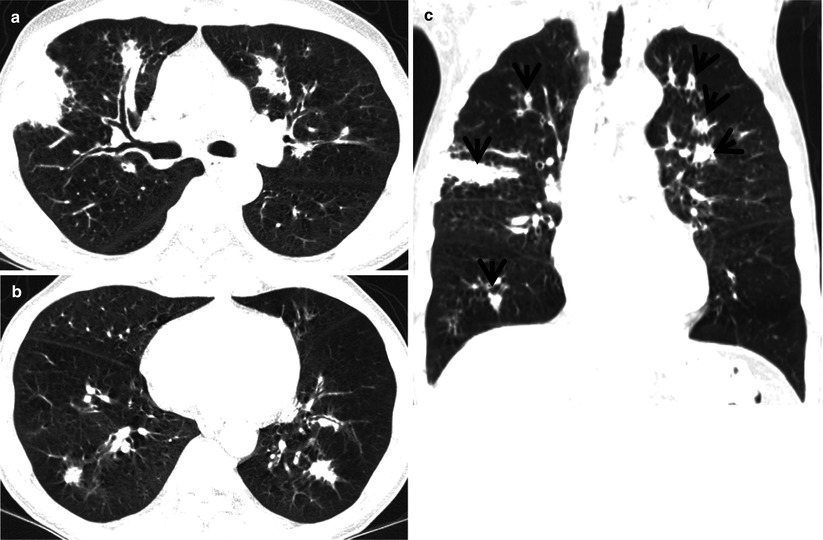
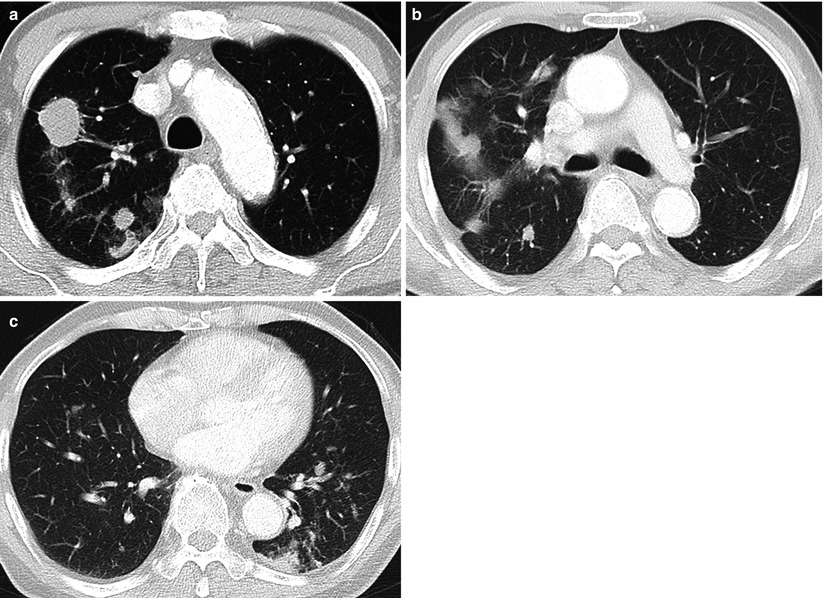
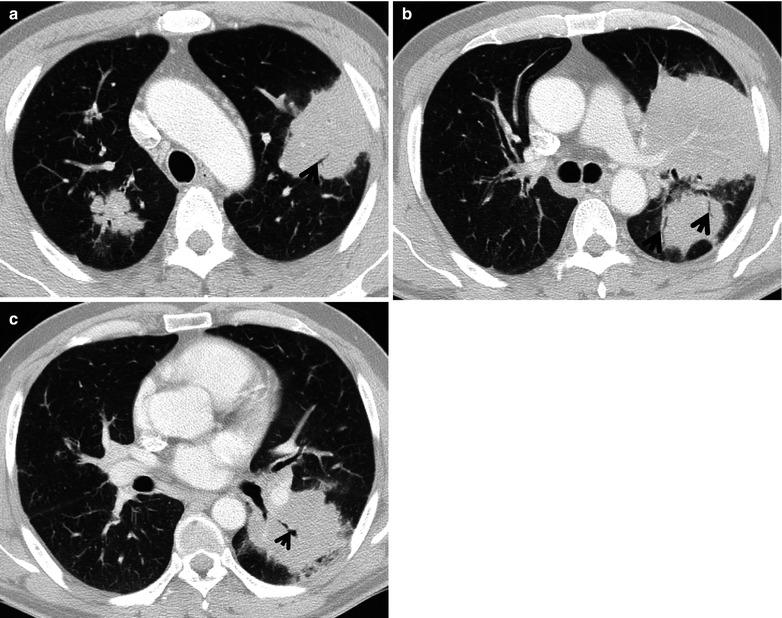
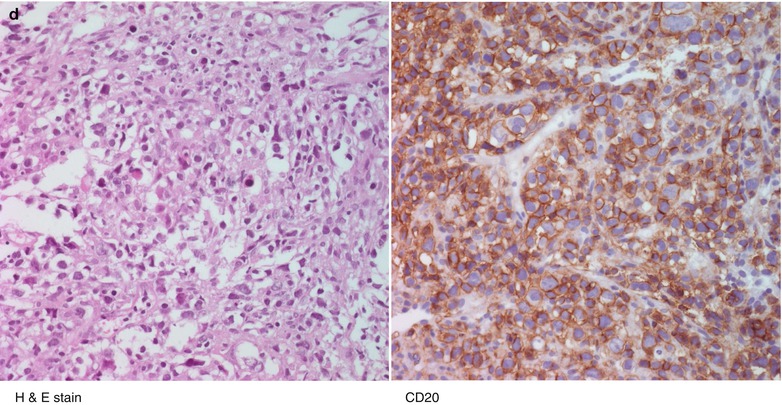
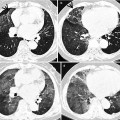
Fig. 19.3
Diffuse large B-cell lymphoma involving lung parenchyma in a 48-year-old man who is complaining of febrile sense, cough, and dyspnea. (a–c) Lung window images of CT scans (2.5-mm section thickness) obtained at levels of aortic arch (a), main bronchi (b), and bronchus intermedius (c), respectively, show multiple variable-sized nodules and masses in both lungs. Lesions typically have bronchovascular distribution. Also note CT air-bronchogram signs (arrows) within mass lesions. (d) Photomicrographs of H & E staining (left) and immunohistochemical staining of CD20 (right), respectively, disclose atypical, pleomorphic, and large lymphoid cells and reactive to CD20. These findings are compatible with large B-cell lineage lymphoma
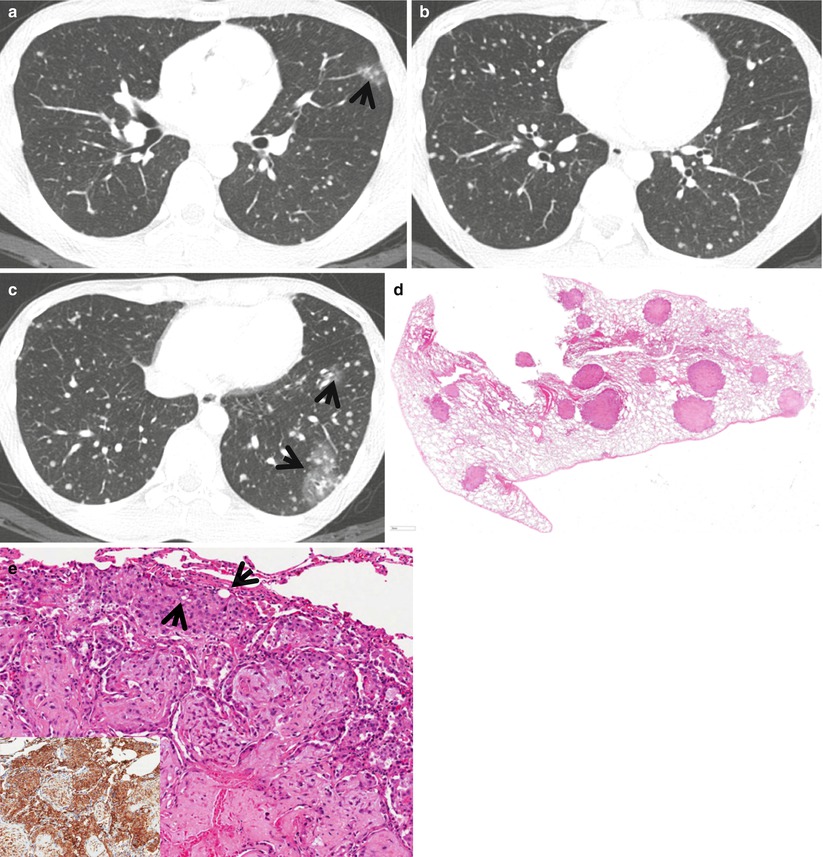
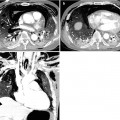
Fig. 19.4
Epithelioid hemangioendothelioma appearing as multiple innumerable pulmonary nodules in both lungs in a 22-year-old man. (a–c) Lung window images of CT scans (2.5-mm section thickness) obtained at levels of right middle lobar bronchus (a), cardiac ventricle (b), and suprahepatic inferior vena cava (c), respectively, show multiple variable-sized small nodules in both lungs. Nodules show random distribution. Also note surrounding ground-glass opacity (arrows) in some nodules, suggestive of associated hemorrhage. (d) Low-magnification (×40) photomicrograph exhibits multiple nodules having central sclerotic and peripheral mild cellular (epithelioid endothelial proliferation) components. Nodules are distributed randomly. (e) High-magnification (×200) photomicrograph discloses abundant eosinophilic stroma and tumor cells containing prominent cytoplasmic vacuoles or intracytoplasmic lumina (arrows). Inset: positive staining for CD31 indicating endothelial origin of tumor cells
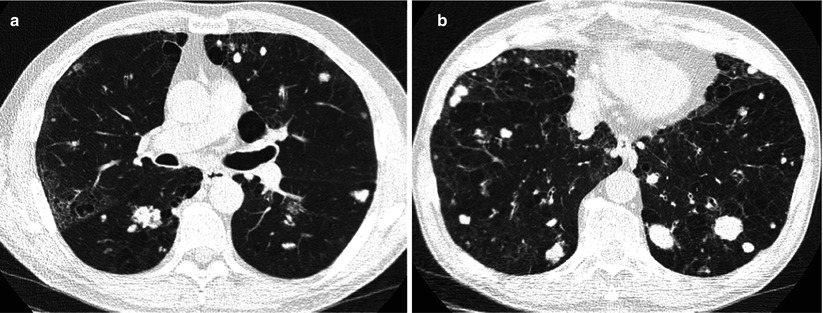
Fig. 19.5
Biopsy-proven (surgical lung biopsy using video-assisted thoracoscopic surgery) amyloidomas presenting as multiple variable-sized nodules in a 62-year-old man. (a, b) Lung window images of thin-section (1.5-mm section thickness) CT scans obtained at levels of bronchus intermedius (a) and suprahepatic inferior vena cava (b), respectively, show multiple lung nodules of different size. Also note accompanying emphysema and bullae in both lungs
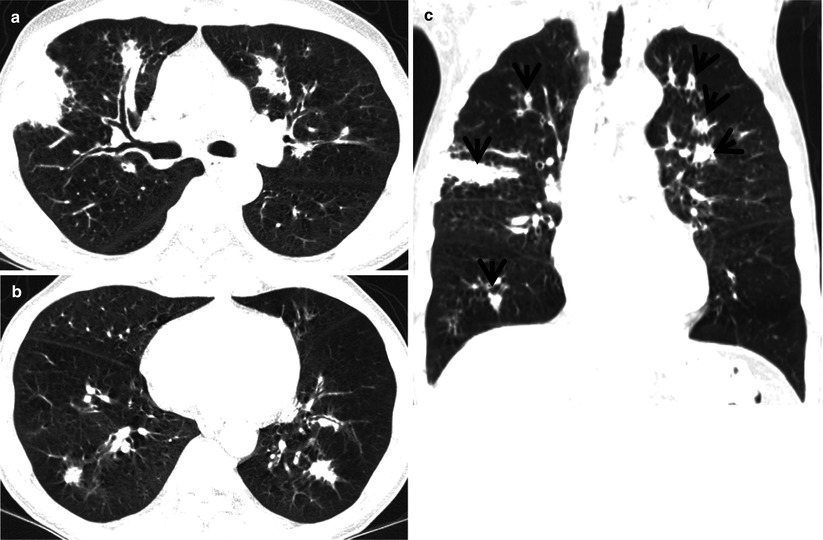
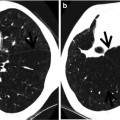
Fig. 19.6
Antineutrophil cytoplasmic antibody (ANCA)-associated granulomatous vasculitis displaying multiple masses in a 64-year-old man. (a, b) Lung window images of thin-section (1.5-mm section thickness) CT scans obtained at levels of right upper lobar bronchus (a) and cardiac ventricle (b), respectively, show multiple variable-sized nodules and masses in both lungs. Lesions are typically located along bronchovascular bundles or subpleural lungs. Also note relatively extensive pulmonary emphysema. (c) Coronal reformatted CT image (5.0-mm section thickness) demonstrates nodules or mass (arrows) of diverse size in both lungs, which are distributed along bronchovascular bundles. Also note extensive emphysema in both lungs
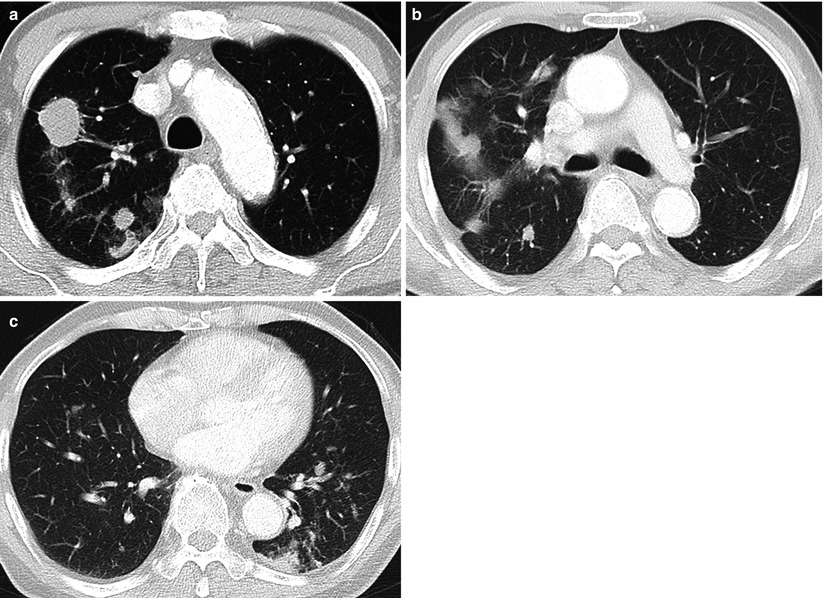
Fig. 19.7
Pulmonary cryptococcosis manifesting as multiple variable-sized nodules in both lungs in a 72-year-old man. (a–c) Lung window images of CT scans (2.5-mm section thickness) obtained at levels of aortic arch (a), main bronchi (b), and cardiac ventricle (c), respectively, show multiple variable-sized nodules and masses in both lungs. Lesions are located along bronchovascular bundles or subpleural lung. Core biopsy from right upper lobe nodule discloses cryptococcal organisms
Distribution
Lesions in abovementioned diseases show random distribution.
Clinical Considerations
The presence of multiple nodules or masses in both lungs in a patient with extrathoracic malignancy or primary lung cancer suggests the diagnosis of pulmonary metastases or lung-to-lung metastases. Pulmonary nodules in a patient with rheumatoid arthritis may favor the diagnosis of necrobiotic nodules (rheumatoid nodules). Approximately 15–20 % of patients with pulmonary epithelioid hemangioendothelioma (EH) have a hepatic involvement. Pulmonary EH manifesting as multiple nodules have a relatively good prognosis, whereas the disease manifesting as reticulonodular lesions or diffuse infiltrative pleural thickening have aggressive clinical courses. Lung nodules in a patient with chronic inflammatory disease (e.g., Sjögren’s syndrome) or systemic lymphoproliferative disorders and plasma cell dyscrasias (e.g., multiple myeloma) may suggest the presence of amyloidomas [2]. Nocardiosis is a disease in patients with underlying diabetes or chronic kidney disease [3]. Common predisposing factors for septic embolism include tricuspid valve endocarditis with or without IV drug addiction, alcoholism, skin infection, and peripheral septic thrombophlebitis [4]. Airway invasive pulmonary aspergillosis is a disease in immunocompromised patients (those who have hematologic malignancy and who underwent hematopoietic stem cell transplantation) particularly whose peripheral blood absolute neutrophil count is <500 cells/μL (neutropenia). Cryptococcosis is an indolent lung infection in mildly immunocompromised patients [5]. Generalized symptoms and signs, such as diffuse alveolar hemorrhage, acute glomerulonephritis, chronic refractory sinusitis or rhinorrhea, imaging findings of nodules or cavities, and multisystemic disease, precede typical imaging findings in pulmonary vasculitis [6].
Key Points for Differential Diagnosis
Diseases | Distribution | Clinical presentations | Others | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Zones | |||||||||||||
U | M | L | SP | C | R | BV | R | Acute | Subacute | Chronic | |||
Pulmonary metastasis | + | + | + | + | + | + | Variable-sized nodules | ||||||
Lymphoproliferative disease | + | + | + | + | + | ||||||||
Pulmonary epithelioid hemangioendothelioma | + | + | + | + | + | ||||||||