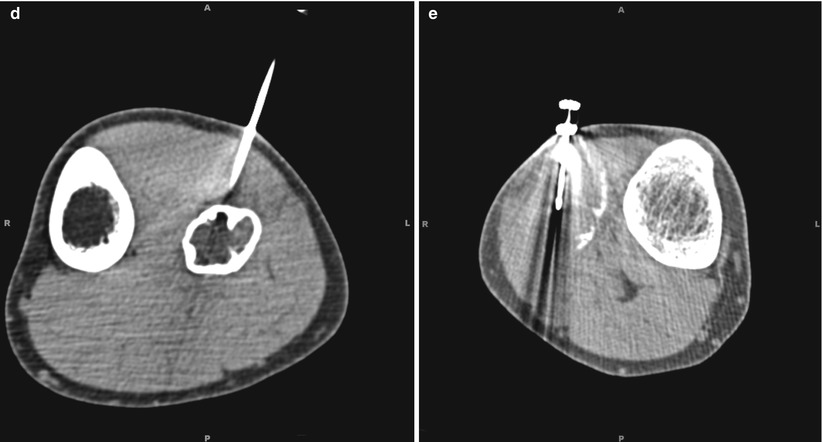
Fig. 24.1
A 23-year-old man presented with a 6-month history of increasing discomfort in his right proximal lateral calf. The patient brought outside images of both fibulas on plain film as well as an MRI scan of each side. Plain radiograph (a) showed a lesion of the left fibula with thin internal septations and without evidence of periosteal reaction or cortical break. An expansile destructive lesion was noted within the right fibular head, featuring thinning of the cortex and minimal periosteal reaction. Neoplasm was suspected and MRI was recommended. Sagittal MRI (b) demonstrated an expansile lesion within the proximal left fibular diaphysis. There was no evidence of bone marrow edema in the surrounding bone and no evidence of periosteal reaction. On the postcontrast images, there appeared to be central enhancement of this lesion. Coronal MRI (c) showed an expansile lesion in the head and proximal metaphysis of the right fibula. A soft-tissue component has extended into the proximal medullary canal. There was edema within the fascial planes surrounding the mass and within the extensor digitorum longus, fibularis longus, and lateral soleus muscles. The periphery of this lesion showed irregular enhancement. The tibial artery and vein ran along the medial border of the lesion and the fat plane was effaced, but there was no encasement of the artery or vein. The common peroneal nerve was obscured, but the lesion followed the expected course of the nerve. Axial CT image (d) showed an expansile lytic lesion of the proximal left fibular shaft with mild internal bony septation. A Bonopty access cannula (outer diameter 2.1 mm) was advanced into this lesion. Appropriate positioning within the targeted lesion was ensured by intermittent CT fluoroscopic observation. A total of four passes were made using 22-gauge needles for fine-needle aspiration. A Bonopty core biopsy device (inner diameter 1.3 mm) also was used for sampling. Two marrow aspirates were also collected. There was no evidence of malignancy on cytopathologic examination. Axial CT image of the right leg (e) showed a heterogeneous expansile lesion replacing the right fibular head with areas of cortical disruption. Using intermittent CT fluoroscopic observation to ensure appropriate needle positioning within this lesion, a total of four passes were made using 25-gauge needles for fine-needle aspiration. An additional nine passes were made with a 16-gauge Monopty core biopsy device. The cytopathologic findings were interpreted as a giant cell tumor with aneurysmal bone cyst features
A practical approach to PNB of the musculoskeletal system is to differentiate between biopsy of the appendicular skeleton and biopsy of the axial skeleton. Important differences in anatomy between the two lead to distinct complications and recommendations for imaging and interventional techniques. By virtue of anatomic location, PNB of the appendicular skeleton does not have the inherent risk of damage to vital organs that can occur in procedures for the axial skeleton. For example, complications such as pneumothorax or more serious iatrogenic pathologies such as nerve root injury are specific to the axial skeleton [9]. This chapter focuses on percutaneous image-guided biopsy of the appendicular skeleton, providing an in-depth assessment of the interventional techniques and tools that are utilized for lesions of the extremities. The chapter also discusses recommended practice pearls for avoiding the potential pitfalls and complications that can occur in percutaneous image-guided biopsy of lesions of the appendicular skeleton.
Indications and Patient Selection
The first step for ensuring an accurate and clinically useful PNB of the appendicular skeleton is to utilize appropriate indications and patient selection criteria. The decision whether to perform a biopsy should be made by the interventionalist together with the surgeon who will be treating the patient.
Indications for Appendicular Musculoskeletal Biopsy
1.
Evaluation of a solitary bone or soft-tissue lesion with nonspecific imaging findings in order to establish its benign or malignant nature.
2.
Confirm imaging and staging for cases of suspected metastasis.
3.
Confirm diagnosis of suspected infection and identify the organism.
4.
Re-biopsy for initially negative or inconclusive findings.
5.
Re-biopsy for evaluation of suspected residual/recurrent disease.
6.
Determine the nature and extent of systemic diseases.
The question in the case of a suspected primary neoplasm of the appendicular skeleton is whether the musculoskeletal lesion is benign or malignant. Previously, there was debate concerning the utility of PNB for primary musculoskeletal neoplasms such as bone sarcomas. However, because of its low complication rates and improvements in its diagnostic accuracy, PNB is now recommended generally for most lytic and blastic lesions in the appendicular skeleton [10]. Some cases of primary lesions still require special considerations, however, including (1) cartilaginous lesions, (2) liposarcomas, and (3) pathologic fractures. For some cartilaginous lesions, differentiation between benign and malignant may be difficult. Cases have been reported in which a chondrosarcoma was erroneously diagnosed as an enchondroma, possibly because of difficulty obtaining adequate tissue from noncalcified areas, which are more representative of the malignancy than calcified areas [11]. If the initial histopathologic analysis of the PNB is read as an enchondroma, the patient should be monitored to confirm this diagnosis. Conversely, some benign lesions such as synovial chondromatosis or chondromyxoid fibromas may show cytologic atypia leading to a misdiagnosis of chondrosarcoma. Ultimately, differentiating benign cartilage lesions from malignant tumors requires evaluation of clinical presentation, imaging, and histopathologic interpretation as well as assessment of changes in the lesion over time [12].
Other lesions that may be difficult to diagnose are soft-tissue tumors that are highly heterogenous [13, 14]. For example, PNB is not recommended for differentiating low-grade liposarcomas from lipomas [15]. Another special circumstance for biopsy is a pathologic fracture. In some of these cases, imaging may be inconclusive as to whether there is an underlying lesion that led to the fracture. If a malignancy cannot be ruled out on the basis of imaging alone, PNB is recommended.
Percutaneous needle biopsy is utilized to confirm that a suspected metastatic lesion is a metastasis rather than a new primary tumor and to confirm staging of the disease. Biopsy confirmation is especially important when there is uncertainty about diagnosis, as in cases where the lesion appears atypical for the type or stage of the primary tumor or if the lesion is suggestive of metastatic disease but there is no known primary tumor. For cases with no known primary lesion, a number of common sites of neoplastic origin should be considered, such as the lungs, prostate, breasts, kidneys, and thyroid. Successful biopsy of metastatic disease should be considered the final step in staging prior to the referring physician discussing appropriate management options with the patient. Because the biopsy induces subsequent real and artificial radiologic changes that may inhibit future imaging interpretation, the biopsy should be conducted only after completion of imaging studies for staging the disease by assessing any local and/or metastatic spread.
Percutaneous needle biopsy is also utilized in patients who have suspected infection. These patients typically have an initial assessment and laboratory values that are highly suggestive of infection, and the referring physician requests a biopsy to identify the organism and subsequently the appropriate treatment protocol. Suspicion of septic arthritis, either pyogenic or granulomatous, is an important indication for PNB. For patients who have suspected osteomyelitis, the bone biopsy specimens should undergo both microbiologic and histologic evaluation [16]. Percutaneous biopsy may also be requested to distinguish between infection and possible malignant disease.
The case of a negative result or an indeterminate tumor diagnosis presents a difficult decision. As previously noted, some of these may be “negative” in the sense that the lesion is identified as benign rather than the suspected malignant disease. Re-biopsy is typically not recommended unless there is change in the lesion to suggest malignancy. Initially inconclusive cases also are considered for re-biopsy. For example, a cystic or necrotic lesion such as a telangiectatic osteosarcoma may yield only fibrin, blood, or serous fluid that does not allow differentiation from a simple cyst, and re-biopsy is required if there is sufficient clinical suspicion or aggressive imaging appearance. Other reports of normal, inconclusive, or nonspecific biopsies may arise from poor technique, missed lesions, inappropriate handling of specimens, or sampling nonrepresentative portions of the lesion. Either open biopsy or repeat percutaneous biopsy can be utilized for these difficult cases.
Another situation that may warrant re-biopsy is when patients present with a lesion in the appendicular skeleton after they have already undergone therapy with curettage, resection, chemotherapy, and/or radiotherapy. Patients may present with a lesion at the primary site of treatment that is suggestive of local recurrence or a lesion at a new site (often several years later) that is suggestive of metastatic disease. The cases that are suggestive of metastatic disease are especially important for diagnostic biopsy to determine whether the patient has recurrence of primary disease or a new neoplasm that has not yet been identified.
The final reason for biopsy is to determine the nature and extent of systemic diseases. For example, the treatment for connective tissue diseases may be customized on the basis of the findings on biopsy of the synovial membrane [17, 18]. While synovial samples can be obtained via open or arthroscopic surgery, PNB is advantageous because it allows removal of specimens from several regions of the joint with minimal trauma. These biopsies are not always definitive, but rather contribute to the diagnosis when combined with several other criteria.
Contraindications
Although there are a number of relative contraindications for PNB of the appendicular skeleton, the only absolute contraindication is for lesions that can be diagnosed accurately on the basis of clinical and imaging studies alone. The presence of a bone or soft-tissue lesion does not necessarily merit a biopsy, and in cases in which the medical history, physical examination, laboratory results, and appropriate imaging studies allow accurate diagnosis of a musculoskeletal lesion, confirmatory biopsy should not be performed. For example, benign lesions such as intraosseous ganglia, subchondral sclerosis and cystic changes associated with advanced osteoarthritis, and enchondroma bone islands may appear as suspect lucent or sclerotic foci in patients with a known malignancy, but they can be differentiated by utilizing imaging findings and reviewing previous studies. Apophyseal avulsions in young patients are also sometimes mistaken as a malignancy. However, location of the lesion and clinical history are key differentiating points for these cases.
Relative Contraindications for Appendicular Musculoskeletal Biopsy
1.
Bleeding diathesis (severe coagulopathy or thrombocytopenia)
2.
Lack of safe biopsy tract.
3.
Compromised cardiopulmonary function or hemodynamic instability
4.
Uncooperative patient or inability to be positioned for the procedure
5.
Inadequate institutional infrastructure for the procedure
A simple medical history is typically sufficient to assess for coagulopathy in patients prior to biopsy of an extremity because there is a relatively low risk for vascular complications. For patients with a medical history suggestive of or a known existing bleeding diathesis, laboratory measurements of the patient’s prothrombin time, activated partial thromboplastin time, and international normalized ratio are recommended, and abnormalities should be corrected before the biopsy. For patients who require urgent biopsy, fresh frozen plasma can be administered shortly before the procedure to temporarily correct values. When the biopsy site is in close proximity to large vessels, the potential increased risk for bleeding may suggest consideration of alternative approaches. A hematology consultation may be required to deal with coagulopathies that the radiologist does not have experience in correcting. Special attention should be given to patients with a coagulopathy who are taking nonsteroidal anti-inflammatory drugs that can prolong the bleeding time [19]. There have been reports of significant bleeding weeks after discontinuing aspirin, despite normal platelet counts [20].
When determining the planned biopsy tract, the presence of infected soft tissue must be addressed. If the infection is along the planned tract and the target lesion is not considered likely to be infection on the basis of initial clinical and radiographic assessments, another tract should be selected or the patient should be treated for the infection before proceeding with the biopsy. Although there are no sites in the appendicular skeleton that are contraindicated solely because of inaccessible anatomic location, extensive soft-tissue infection may in effect make the targeted biopsy site inaccessible. In contrast, there are sites in the axial skeleton, such as the odontoid process and anterior arch of the first cervical vertebra, that are considered contraindications for PNB because of anatomic features that make the sites inaccessible [21].
Caution should be used in patients who have compromised cardiopulmonary function or hemodynamic instability. Patients who have a history of myocardial infarction, chronic heart failure, or other high-risk chronic medical condition should have a thorough pre-biopsy medical evaluation and clearance by their primary care physician. Because of the low risk for complications of appendicular biopsies, these patients should be considered appropriate candidates for biopsy once their medical condition is optimized.
Uncooperative patients, especially children, may require general anesthesia. As with any surgical case requiring general anesthesia, the risks and benefits of the procedure must be assessed. Patients who are overly concerned about the procedure but are considered high risk for general anesthesia may tolerate a benzodiazepine or other sedating medication that will allow them to undergo the procedure with only local anesthesia.
The last relative contraindication is a function of the treatment center rather than the patient. If the institution is not equipped to perform PNB on a regular basis, the accuracy of the diagnostic studies may be questionable. Definitive diagnosis with appropriate treatment is best performed at an institution that has a team consisting of an orthopedic surgeon, radiologist, and pathologist who coordinate their efforts in selecting appropriate patients, performing the biopsy, providing histopathologic analysis, and subsequently managing the continued care of the patient [4, 22, 23].
Technique
The importance of technique in performing a biopsy has been magnified by the change in treatment options. Historically, most malignant tumors of the extremities were treated with amputation. The biopsies that were conducted prior to the amputation were generally performed by an open surgical approach where contamination of the surrounding tissue was inconsequential. However, there has been a significant shift over the last several decades away from amputation and toward limb-sparing surgery. Today, as many as 95 % of patients are able to undergo limb-sparing procedures without compromising the oncologic outcome [27–29]. Therefore, biopsy must be preceded by careful clinical evaluation and analysis of the imaging studies. The diagnostic accuracy may be greatly influenced by the biopsy method and equipment utilized as well as the location of sampling. Furthermore, a poorly planned or performed biopsy may result in the patient requiring a more radical dissection or amputation with a significant negative impact on long-term survival [4, 30, 31]. The three most critical factors that need be considered for an optimal outcome are (1) preprocedure and intraprocedure imaging, (2) the interventional devices utilized, and (3) the approach and relevant anatomy.
Imaging
Imaging plays an important role in pre-biopsy planning as well as in facilitating localization of the lesion at the time of biopsy. Prior to biopsy, radiographs in two projections as well as CT or MRI scan of the lesion should be obtained for all patients. If more than one site of metastasis is suspected on the basis of initial imaging studies, the most accessible site that will provide adequate tissue should be selected for biopsy. Bone scintigraphy may be useful in patients with metastatic disease to identify additional lesions that are more accessible than initially detected disease sites [32]. In cases where there are multiple lesions with different imaging characteristics, more than one biopsy is needed [33].
The biopsy can be guided by fluoroscopy [10, 11, 34], ultrasound [23, 35], CT [14, 31, 36, 37], or MRI [38, 39]. Each of these imaging modalities has pros and cons in terms of costs, radiation exposure, time required to complete the biopsy, and efficacy in locating the lesion and determining its relevant characteristics. In rare cases, imaging choice is dependent on available imaging modalities and patient positioning.
Fluoroscopy is recommended for lesions of the extremity that do not require careful negotiation of neurovascular structures. Low soft-tissue contrast makes fluoroscopy less ideal for lesions with large cystic or necrotic areas. Biplane fluoroscopy is recommended over conventional fluoroscopy for deeper lesions because of its ability to accurately determine the needle depth. The advantages of fluoroscopy compared to CT and MRI are that it is easy to use; allows fast, multidirectional, near real-time visualization; and costs substantially less.
Ultrasound can be utilized for biopsy of superficial soft-tissue lesions, lesions that have some degree of subperiosteal or extraosseous extension, or bone lesions that demonstrate cortical disruption with an adequate acoustic window for passage of the biopsy needle [40–42]. Lesions that were traditionally targeted with palpation alone are now often visualized with ultrasound to avoid complications such as disruption of vascular structures and to ensure intralesional sampling (Fig. 24.2). Ultrasound is inadequate for visualizing deep medullary bone lesions and deep soft-tissue lesions because of poor sound penetration. The advantages of ultrasound are that it provides real-time visualization, color Doppler imaging for regions of variable tissue and adjacent vascular structures, and no radiation to the patient or the interventionalist. Ultrasound is also relatively inexpensive and requires minimal patient and preprocedure preparation, and the procedure can be performed more quickly than a CT-guided biopsy [23].
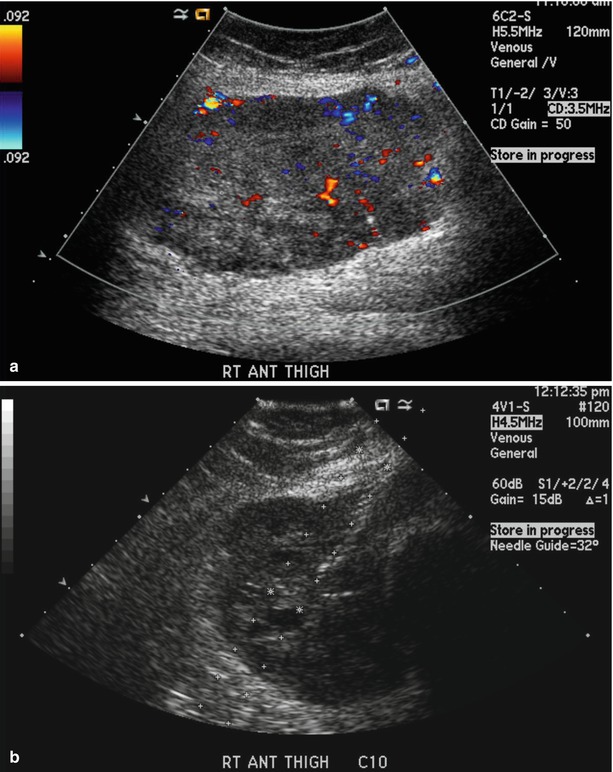
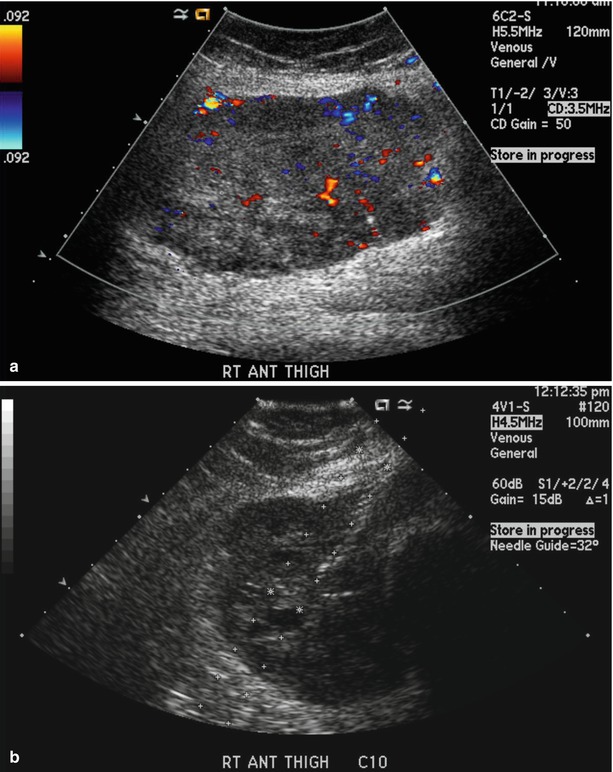
Fig. 24.2
An 83-year-old woman was referred for evaluation of a right anterior thigh mass. The patient described a 6-week history of right anterior thigh fullness near the knee. Ultrasound evaluation of the right anterior distal thigh showed a heterogeneously echogenic solid mass (a). With ultrasound guidance (b), 22-gauge needles were advanced into the mass at four different sites, and eight samples were obtained by the capillary technique. Three core biopsy samples of the lesion were obtained with an 18-gauge Monopty biopsy device. The biopsy revealed a pleomorphic high-grade sarcoma of the right thigh
While CT is frequently required for lesions of the upper thoracic and cervical spine, skull base, and facial bones [21], there are fewer concrete indications for the use of CT in the appendicular skeleton, and some cases are based on operator preference. Deep lesions or lesions adjacent to neurovascular bundles may require a high-resolution “road map” of the compartmental anatomy that is best provided by CT. In comparison to fluoroscopy, CT has an additional element of safety because it can provide better soft-tissue visualization, which allows more precise needle placement within three dimensions [20, 43, 44]. One of the arguments against the use of conventional CT is that it can be time consuming during positioning. However, CT fluoroscopy can address this limitation by providing real-time visualization that allows instantaneous cross-sectional anatomic imaging.
Magnetic resonance imaging is often used for lesions that are not identified on other imaging modalities (Fig. 24.3) and for targeting a focal marrow abnormality or specific portion of a heterogenous lesion that is targeted for biopsy. Intra-articular locations represent a unique group for which lesion conspicuity and real-time guidance are both important issues that are best addressed by MRI. Like CT, MRI is ideal for creating high-resolution reconstructions of the associated compartmental anatomy for deep lesions. Finally, there are some indications for MRI that are more case specific. For example, if a patient has orthopedic hardware near a lesion, use of CT may be limited by streak artifacts. The advantages of MRI are that there is no radiation, it is a cross-sectional technique with an easily adjustable imaging plane, and it provides superior tissue contrast. Some of the disadvantages are the cost of deploying and maintaining a specialized magnet or modifying an existing magnet and suite for interventional use and the currently higher cost of MR-compatible biopsy equipment. There are also specific contraindications to the use of MR, such as the presence of a pacemaker, certain cerebral aneurysm clips, cochlear implants, or other strongly ferromagnetic material near critical locations.
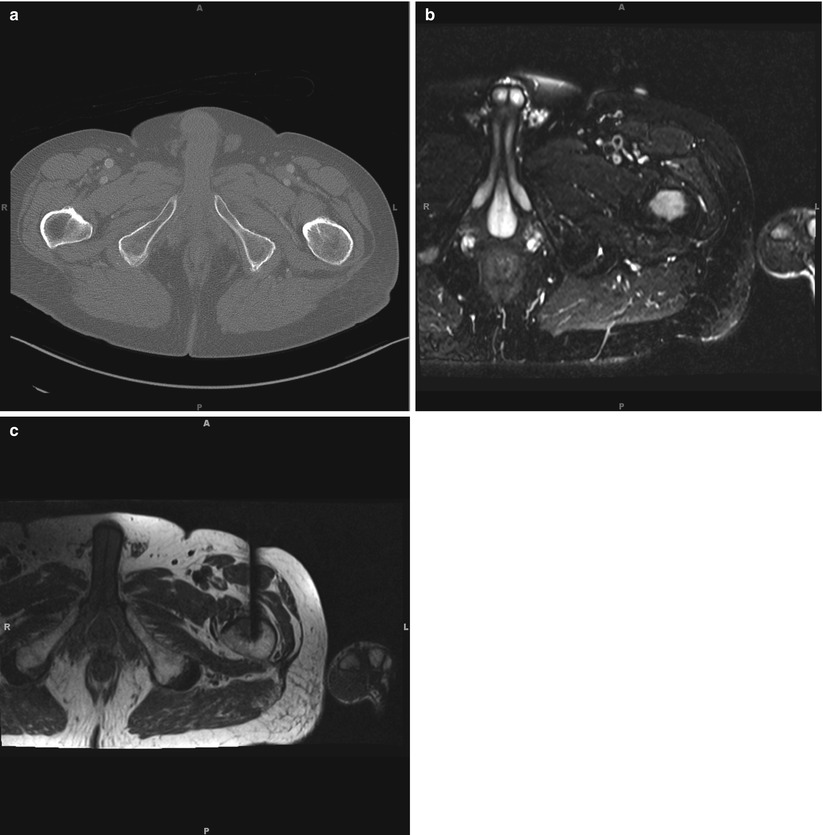
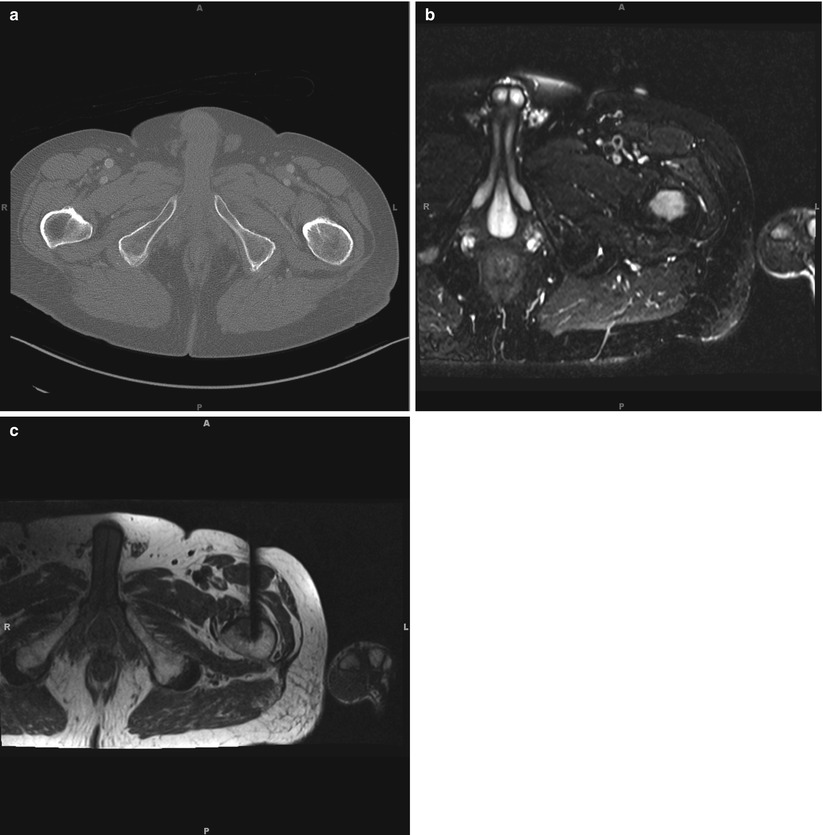
Fig. 24.3
A 78-year-old man with 3 to 4 months of left hip and thigh pain had an MRI at an outside institution which reported a suspicious lesion in the left proximal thigh. With a broad differential inlcuding metastasis of an unknown primary, lyphoma, and myeloma, the patient underwent a screening chest and abdomen CT and presented to our institution for possible biopsy of the lesion. The CT (a) showed diffusely osteopenic bones but no definite evidence of discrete lesion that could be target for biopsy. The patient subsequently agreed to undergo MRI-guided biopsy. Pre-biopsy T2, turbo spin echo, fat saturated imaging (b) redemonstrated the T2-hyperintense lesion in the proximal femur which was noted on the prior outside MRI study. Under real-time MRI guidance (c), a 4 mm MRI compatible coaxial bone biopsy needle system was utilized. A total of 3 core needle biopsies were obtained from the lateral, central and medial portions of the lesion. Pathology reported findings consistent with diffuse large B-cell lymphoma which included bone and marrow space diffusely and extensively involved by an atypical lymphocytic infiltrate composed of large cells that were CD20, CD10, and Bcl-6 positive and had abundant cytoplasm, vesicular chromatin, and conspicuous nucleoli
Devices
Proper needle selection is equally as important as appropriate imaging modality in providing accurate biopsy diagnosis. Core-needle biopsy (CNB) is generally considered more accurate than fine-needle aspiration (FNA) because of the larger yield of specimen available for diagnosis [10, 33]. However, FNA can provide rapid, onsite cytopathologic assessment of the adequacy and character of the tissue specimens to guide additional sampling, whereas CNB results are usually not available for several days. These advantages and disadvantages of CNB and FNA are largely complementary, and multiple studies have reported that CNB and FNA have greater clinical utility when used together than when used alone [45–47].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree