Musculoskeletal Infections: PET-CT and SPECT-CT Imaging
Katrin D. M. Stumpe
Klaus Strobel
Juerg Hodler
Infections of bones and joints are severe diseases that can result in debilitating joint destruction, joint fusion, or bone and soft tissue defects. Early diagnosis is the key to successful therapy and prevention of complications. Commonly, infection is not limited to one compartment. Osteomyelitis and septic arthritis may be associated with soft tissue infections including cellulites, abscess formation, or fasciitis. Conversely, soft tissue infections may involve bones and joints. A good example is diabetic foot, which typically starts as soft tissue infection and then proceeds to bone and joint infection. The ideal imaging method should not only be sensitive and specific in the diagnosis of infection but also be topographically precise. For assessment of soft tissue abnormalities, ultrasound and magnetic resonance imaging (MRI) are commonly used; for joints standard radiographs, ultrasound, and MR imaging; and for bones, standard radiographs and MR imaging. Both ultrasound and MRI are excellent in identifying effusion and soft tissue abscess formation. The cited imaging methods have many advantages, including topographic information, early detection of disease (MR imaging), or extent of bone destruction (standard radiographs). However, these methods tend to be nonspecific, and it may be difficult to differentiate infection from nonspecific edema, trauma, or neoplasm.
In this situation, radionuclide imaging can play an important role. Bone scans are sensitive in diagnosing bone and joint infections. Many institutions use labeled leucocytes as the standard of reference to identify infectious foci in the musculoskeletal system. Major weaknesses of this method are in imaging chronic infections and the axial skeleton (see Chapter 58). Similarly, antigranulocyte antibody imaging has a definitive role in imaging osteomyelitis of the peripheral skeleton. Integrated single-photon computed tomography (SPECT) and computed tomography (CT) may assist in the differentiation of increased uptake by using image coregistration. This is particularly promising in skeletal imaging.
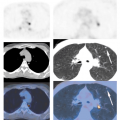
Fluorodeoxyglucose (FDG) positron emission tomography (PET) has shown encouraging results for diagnosing both acute and chronic infection of the trunk and the extremities and seems to be more accurate in detecting chronic osteomyelitis than conventional functional imaging, including bone scan, antigranulocyte antibody imaging, and labeled leucocyte imaging (see Fig. 60.1). Whether PET has the potential to replace conventional scintigraphy completely depends on several factors, including cost and availability. FDG-PET makes use of the fact that there is no physiologic FDG accumulation in white blood cells not actively fighting inflammation. Therefore, granulocytes residing in the hematopoietic marrow do not demonstrate activity, which permits imaging of the axial skeleton. FDG-PET may be superior to MRI in distinguishing disc space infection from erosive osteochondrosis. Data with FDG-PET/CT concerning osteomyelitis in diabetic foot are controversial.
Experience with FDG-PET-CT and SPECT-CT in the musculoskeletal system is still limited, and more data have to be gathered before a definitive role in the imaging algorithms for infection can be assigned to them. Combined PET-CT improves the limited anatomic information of FDG-PET.
General Remarks
Musculoskeletal infections can be divided into infections occurring in the axial and the peripheral skeleton. Infections of the axial skeleton include sternal osteomyelitis, disc-space infection, and vertebral osteomyelitis. Osteomyelitis of the long bones and of the foot, for example, in patients with diabetic pedal ulcers belong to the group of peripheral musculoskeletal infections. Some patients with musculoskeletal infections have undergone osteosynthesis or have metallic prostheses. As presentation on positron emission tomography (PET) scans of these patients is somewhat special, there is a separate discussion of this topic in Chapter 61.
In children, involvement of the bones and joints of the peripheral skeleton is frequent (see Chapter 66). In adults, peripheral musculoskeletal infections occur frequently in patients with trauma and diabetes, but infections of the vertebral column become more common. Bone infections are typically hematogenous, but may also be caused by surgery, penetrating trauma, or by continuity, for instance, in ulcers found in diabetic feet.
Triple-phase bone scintigraphy is sensitive in the early diagnosis of infection. In addition, 67Ga, leucocytes and monoclonal antibodies are used to increase the specificity in cases of positive bone scintigrams (1). However, the need to use multiple tracers and to perform imaging at multiple times adds complexity to the procedure and is an inconvenience to patients.
A single imaging method, equally sensitive and specific, would be preferable. Magnetic resonance imaging (MRI) is accurate in the detection of musculoskeletal infections and is currently the most widely used imaging method in the workup of musculoskeletal diseases. MRI provides at the same time anatomic details and abnormalities of bone marrow, joints, and surrounding soft tissues with high sensitivity (2). It provides adequate spatial resolution and tomographic capabilities, which are required to distinguish between bone and soft tissue infection. Computed tomography (CT) has proven to be a useful adjunct to MRI in the detection of bone sequestration and identifies even small devitalized bony fragments. In this regard, CT is superior to MRI (2).
Recent publications on the use of fluorodeoxyglucose (FDG) positron emission tomography (PET) in chronic musculoskeletal infections suggest that this method is promising (3,4,5). In contrast to conventional nuclear infection scanning, PET results are obtained with a single scan obtained 40 to 60 minutes after injection of the radiopharmaceutical. Recently introduced combined PET-CT imaging may even be superior in musculoskeletal infection. PET is sensitive in demonstrating disease activity. CT demonstrates the precise anatomic location of the finding and alterations of bone structure. Similar aspects may be true for SPECT-CT cameras. However, the spatial resolution might be a limiting factor for the detection of small infectious lesions such as ulceration in diabetic feet.
Musculoskeletal Infection: Peripheral Skeleton
Acute and Chronic Osteomyelitis of the Long Bones
Osteomyelitis is a serious health problem that can result in severe morbidity and loss of function. Conventional radiographs may not be diagnostic because bone destruction and periosteal new bone formation in acute hematogenous osteomyelitis is typically noted only after approximately 2 weeks after disease onset, although acute infection may present earlier with subtle signs of abnormality such as periosteal reaction or obliteration of fat planes between compartments.
Conventional scintigraphy is sensitive in detecting osteomyelitis. Three-phase bone scan is the procedure of choice if the suspected osteomyelitis is not superimposed on another disease causing bone remodeling. This means that standard radiographs should be normal. If the suspected osteomyelitis is superimposed on another disease associated with bone remodeling, leukocyte or granulocyte-antibody imaging is the procedure of choice in the nonhematopoietic marrow-containing skeleton, and leukocyte imaging and bone marrow scintigraphy are the procedures of choice in the hematopoietic marrow–containing skeleton (6).
Osteomyelitis may be classified as acute, subacute, and chronic. Acute osteomyelitis becomes chronic in 15% to 30% of cases. In contrast to acute osteomyelitis, subacute or chronic osteomyelitis is more difficult to diagnose with imaging. Subacute and chronic osteomyelitis with extensive tissue destruction is one of the most severe complications, which can occur after trauma with open fractures and orthopedic surgical interventions. Patients may present with relatively subtle symptoms for a long time. In contrast to acute osteomyelitis, inflammatory parameters such as C-reactive protein, erythrocyte sedimentation rate, and white cell count rate lack sensitivity, especially in the assessment of low-grade infections. MRI assists in the management of these patients, but it is of limited value for discriminating between active residual infection and simple postoperative changes. In addition, the image quality of MRI is severely affected by the presence of metallic implants in these patients (7) (See Chapter 61).
Because edematous and infected tissues are not readily distinguished on MRI, determination of the true extent of the infection is not easy. Edema surrounding active infection easily leads to overestimation of the extent of disease, potentially leading to medical overtreatment or to more extensive surgical intervention than absolutely necessary. Ledermann et al. (7) reported about 100% sensitivity but five false-positive findings with MR in 17 investigated regions in patients with proven chronic posttraumatic osteomyelitis. In patients with chronic osteomyelitis, CT may play an important role because it may demonstrate sequestration, fistulation extending into bone, and bone
defects potentially important for surgical planning and stability of bone.
defects potentially important for surgical planning and stability of bone.
FDG-PET imaging is increasingly used in the diagnosis of acute osteomyelitis of the peripheral skeleton and may also be suitable in suspected chronic infection. In this diagnosis, PET may be useful because FDG is avidly taken up by activated macrophages, which are the predominant inflammatory cells in the chronic phases of infection.
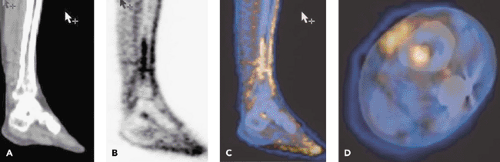
In acute and subacute bone and soft tissue infections, FDG-PET is sensitive and specific. We found a sensitivity of 100% and specificities between 83% and 99% in bone infection (n = 18) (8). In the diagnosis of chronic osteomyelitis, FDG-PET seems to be comparably sensitive and specific. In a study by de Winter et al. (9), sensitivity, specificity, and accuracy in suspected chronic musculoskeletal infection of the peripheral skeleton (27 patients) were 100%, 86%, and 93%, respectively. Similar results were found in a study by Guhlmann et al. (10,11) and by Kälicke et al. (12) in patients with chronic osteomyelitis in the axial and peripheral skeleton. Zhuang et al. (13) demonstrated a sensitivity of 100% and a specificity of 87.5% with two false-positive findings in 22 patients. One of the false-positive patients had a tibial nonunion and the other had an osteotomy. It is well known that postoperative reparative tissue may present with increased FDG uptake. However, when wound healing proceeds properly, fibroblasts predominate and FDG accumulation quickly subsides (14). FDG-PET has a relatively high spatial resolution compared with other nuclear imaging techniques, but the anatomic information available in PET is still limited. PET/CT solves this problem and adds valuable anatomic information (Figs. 60.1 and 60.2).
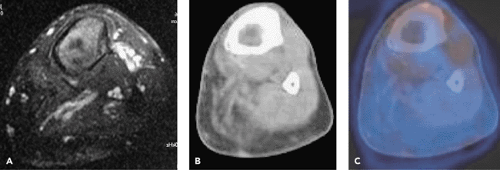 Figure 60.2 Patient with left lower limb amputation and suspected chronic osteomyelitis in the distal part of the stump. Contrast-enhanced T1-weighted fat-suppressed MRI of the left distal bone stump shows moderate contrast media enhancement in the bone marrow (A). CT shows marked left leg atrophy (B). Coregistered PET-CT shows no FDG accumulation in the patient’s femoral stump (C). The clinical follow-up confirmed absence of osteomyelitis.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|