Radiography
Radiography is generally the first imaging modality to be considered when infectious or inflammatory musculoskeletal processes are clinically suspected. It can be often useful for excluding other musculoskeletal causes of patients’ symptoms such as fractures and tumors. For evaluation of soft tissue infection, radiography is not necessarily required but may provide valuable information such as demonstrating the presence of soft tissue gas or foreign body. For assessment of bone infection, the sensitivity of radiography ranges from 43% to 75% and its specificity ranges from 75% to 83%.
1 As a result, initial radiographic results are often negative particularly in the early stages of infectious and inflammatory musculoskeletal disorders. For example, radiographic evidence of loss of bone mineralization is not evident on radiographs until the loss reaches 30% to 50%.
2,
3,
4,
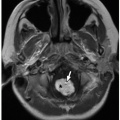
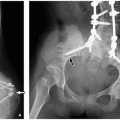
5 However, radiographs may provide subtle information on early findings of infectious and inflammatory musculoskeletal disorders, which include soft tissue swelling, focal osteopenia, subperiosteal resorption, focal radiolucencies (
Fig. 22.1), and periosteal reaction.
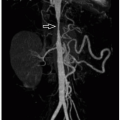
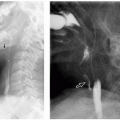
2 Therefore, radiographs may provide clues on underlying pathologic conditions and guide subsequent imaging studies for further investigation. In addition, in cases of chronic infectious and inflammatory disorders, radiographs can be helpful in determining the presence, progression, healing, and complications of the process (
Figs. 22.2,
22.3 and
22.4). In more advanced cases, new periosteal bone formation and cortical destruction can also be detected on radiographs.
Ultrasound
Because of its unique ability to clearly visualize soft tissues without potentially harmful radiation, ultrasound (US) is an attractive imaging modality for use in the pediatric population. US examinations are usually easily tolerated even by infants and young children with parents often holding them for maximal comfort. High-resolution musculoskeletal US requires the use of high-frequency linear transducers (10 to 15 MHz), which can provide optimal visualization of superficial and small structures in the pediatric population. If color Doppler is added to the technique, it can help evaluate hyperemia around the periosteum, synovium, and surrounding soft tissue abscesses often associated with infectious and inflammatory disorders.
US can show soft tissue abnormalities as early as 2 days after the onset of symptoms.
6 Although US is not typically used for evaluation of cortical bone abnormalities, periosteal elevation or subperiosteal collections presenting as a hypoechoic layer of purulent material can sometimes be evaluated with US (
Fig. 22.5). US is useful for diagnosing and following up on soft tissue abscesses, for identifying precipitating factors such as foreign bodies or fistulae, for detecting effusion when transient or septic arthritis is clinically suspected (
Fig. 22.6), and for guiding percutaneous drainage of fluid collections associated with infection for therapeutic purposes.
4 In addition, US can be useful for evaluating regions that are complicated by orthopedic instrumentation and therefore might not be well seen with computed tomography (CT) or magnetic resonance imaging (MRI). Furthermore, US can be a valuable imaging modality in pediatric patients for whom MRI is contraindicated.
Computed Tomography
Computed tomography (CT) is an excellent imaging modality for assessing cortical bone and for detecting gas in soft tissues. However, because it is radiation bearing, the use of CT is currently limited in infants and children with underlying musculoskeletal infectious or inflammatory disorders. Overall, MRI is a preferred imaging modality over CT for evaluation of bone or soft tissue infection or inflammation. However, CT may be the only option for infants and young children when sedation is contraindicated and thus, MRI cannot be performed.
4The currently available postprocessing techniques including multiplanar and 3D reconstructed CT images allow delineation of even the most subtle osseous changes such as early erosions due to infection or inflammation. CT can also clearly show abnormal thickening of the affected cortical bone, sclerotic changes, encroachment of the medullary cavity, and small draining sinuses in chronic osseous infections. In addition, CT can assist in guiding bone biopsies for diagnosis and draining deep abscesses for treatment. For evaluation of bones alone, intravenous (IV) contrast is not usually needed. However, the use of IV contrast can help better assess the presence and extent of associated soft tissue abnormalities such as abscess formation.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) is currently the only imaging modality with the ability to simultaneously assess all relevant anatomic structures in the setting of musculoskeletal infectious or inflammatory disorders. It is the study of choice when a focal or multifocal area of osteomyelitis is suspected. For detecting soft tissue abnormalities, its specificity is up to 97%
7 and its sensitivity, up to 100%.
8 MRI evaluation can reliably differentiate acute from chronic infection.
9 However, MRI may not be helpful in distinguishing infectious from noninfectious inflammatory processes. Recently, screening for multifocal noninfectious conditions with whole-body MRI has shown promising results.
10 Whole-body MRI has a great potential to become evolved into an established and sensitive imaging modality for the diagnostic workup of pediatric patients with underlying multifocal infectious or inflammatory disorders. With the unique advantage of providing a comprehensive single evaluation of the entire body in a reasonable time without IV contrast or radiation, it is particularly beneficial in the pediatric population. Disadvantages of MRI include its occasional inability to differentiate infectious
from reactive inflammation as well as its difficulty with evaluating regions with metallic implants.
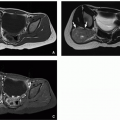
The basic MR imaging protocol for investigation of musculoskeletal infectious and inflammatory disorders includes T1 and T2/short tau inversion recovery (STIR) performed in orthogonal planes. T1-weighted MR imaging is useful for assessment of anatomy and bone marrow. A 3D image acquisition using T1 gradient sequence is useful in the detection of bone erosions, because it allows the generation of multiplanar reconstruction, which adds diagnostic confidence. Fluid-sensitive imaging sequences (T2/STIR) can delineate contrast between normal and abnormal tissue. A gradient echo sequence can be useful to identify hemosiderin, seen as blooming artifacts. The use of gadolinium helps delineate the extent of bone marrow abnormality, differentiate devitalized from vascularized bone, and demonstrate the extent of soft tissue abscesses (
Fig. 22.7) and sinus tracts.
11
Nuclear Medicine
Currently, because of the availability of MRI, nuclear medicine studies are rarely performed for evaluation of infectious or inflammatory disorders particularly in pediatric patients. Nevertheless, they may provide valuable information for children for whom CT or MRI is contraindicated.
Nuclear medicine studies can be of value for evaluating multifocal infections or as a screening imaging modality although they are limited mainly by low spatial resolution. Several nuclear medicine studies are currently available for evaluating pediatric musculoskeletal infectious and inflammatory disorders including technetium-99m methylene diphosphonate (99mTc) bone scan, gallium-67 citrate scan, and indium-111-labeled white blood cell (WBC) scan.
A 99mTc bone scan is usually performed when the area of infection is not well established clinically and the presence of a bone infection is uncertain. It shows elevated blood flow and abnormal increased deposition of tracer at the site of infection (
Fig. 22.8). The tracer accumulates in areas of increased vascularity as well as in areas of increased physiologic activity in direct proportion to the destruction of the bone and osteoblastic healing activity. Triple phase (angiographic, bloodpool, delayed-phase) bone scan can be used when the site of acute osteomyelitis is not known or when multifocal points of infection are suspected.
2 A diagnosis of acute osteomyelitis requires tracer activity in all three phases of bone scan.
2 Bone scan is highly sensitive (sensitivity of 85% to 100%) but not particularly specific (specificity of 54% to 96%) for detecting osteomyelitis.
1,
12 Both sensitivity and specificity of bone scans can be increased with the use of pinhole collimators and single photon emission computed tomography (SPECT).
13 Because of its variable specificity, bone scan may not be able to distinguish among infection, tumor, and trauma. Furthermore, there can be initial false-negative results secondary to ischemia from vascular compression and thrombosis as well as obscuration of subtle abnormal uptake at the metaphysis by normal high physeal uptake.
11,
14Indium-111-labeled WBC scan is used in the diagnostic evaluation of occult infections when other imaging modalities are either contraindicated or noninformative. Labeled leukocytes migrate to and accumulate at sites of inflammation, which are then visualized on nuclear medicine imaging.
15 111In-labeled WBC scans detect localized inflammation but do not clearly distinguish between infectious and noninfectious inflammatory processes.
15 They have been used in the diagnostic evaluation of fever of unknown origin, prosthetic joint infections, and vascular graft infections.
Gallium-67 citrate scan is more specific than 99mTc bone scan for assessment of chronic osteomyelitis, but false positives occur in conditions such as healing fractures, noninfected prosthesis, and tumors.
16 Gallium scan uses radiogallium, which attaches to transferrin and leaks from the bloodstream to the regions of inflammation showing increased isotope uptake in sterile inflammatory conditions, infection, and malignancy.
16 It is often performed in conjunction with bone scan. One limitation of the use of gallium scan is that it does not show bone detail particularly well and may not distinguish well between bone and nearby soft tissue inflammation. In addition, gallium scan involves a higher dose of radiation and requires a longer scanning time than does 99mTc bone scan, making it less appropriate for use in the pediatric population. Gallium scan can take up to 48 hours to be completed, whereas bone scan typically takes up to 3 hours with a delayed view at 24 hours, if necessary.
16