Musculoskeletal Traumatic Disorders
Mark E. Bittman
Jeannette M. Peréz-Rosselló
Donald A. Tracy
Abdusamea Shabani
Edward Y. Lee
INTRODUCTION
Trauma to the musculoskeletal system is common, and imaging plays a crucial role in the evaluation of the injured child. Knowledge of the normal appearance of the immature skeleton and familiarity with variants of normal anatomy are essential when evaluating the imaging of a pediatric patient with suspected traumatic injuries. The presence of growth plates in infants and children results in different fracture patterns and healing processes compared with those of adults. The physical properties of the skeletally immature bone are also different from those of adult bones. Skeletally immature bones are more porous and less mineralized than are mature bones, allowing for elasticity and plastic deformation prior to fracturing. Additionally, the periosteum of children’s bones is thicker and stronger than the periosteum of adult bones, which limits displacement of fracture fragments.1,2,3
In this chapter, the current imaging techniques and protocol guidelines for assessing the pediatric musculoskeletal trauma are reviewed. This chapter also discusses common injuries of pediatric patients on a bone-by-bone assessment including imaging findings, complications of healing, and treatment of injuries. In addition, an overview of accidental and nonaccidental musculoskeletal trauma is provided, with specific discussions on common mimickers of musculoskeletal injuries related to child abuse. Finally, common sports injuries in children are presented.
IMAGING TECHNIQUES
Radiography
Radiographs are typically the initial examination in the evaluation of a pediatric patient with trauma to the musculoskeletal system. Radiographs are readily available, cost effective, and highly sensitive to the detection of fractures and malalignment. However, one should minimize radiation exposure to children by using radiography judiciously and paying close attention to technical factors including collimation and exposure parameters.
The main utility of radiographs in the setting of trauma is to detect fractures. Radiographs define the anatomic relationship between a fracture line and the joint space or growth plate. This information determines fracture classification and has prognostic and treatment implications. Radiographs readily demonstrate displacement and angulation of fracture fragments. Joint subluxations and dislocations are often easily detected with radiographic evaluation. Follow-up radiographs are used to assess healing, to determine anatomic alignment after open or closed reduction of displaced fractures, and to evaluate for potential complications of orthopedic hardware.
A minimum of two orthogonal views is recommended to fully assess a suspected long bone fracture. The proximal and distal joints on either side of a long bone should be included in the field of view to ensure adequate anatomic coverage. Injuries to joints usually require a minimum of three views, namely, anteroposterior (AP), oblique, and lateral views. When specific types of injuries are clinically suspected, specialized views can be obtained, and it is helpful to tailor the examination based on the clinical query. For example, a 30-degree ulnar deviated view of the wrist is helpful in the detection of an early and subtle nondisplaced scaphoid fracture, which has important clinical implications if not diagnosed and managed in a timely fashion. In select cases where the radiographic diagnosis of a fracture is equivocal, obtaining a comparison view of the contralateral asymptomatic side may be helpful to ascertain whether a finding represents an injury or a normal variation of the anatomy.
Radiographic evaluation of soft tissues is limited and lacks the capability for discrimination of fluid from synovium in joints. However, the presence of soft tissue edema and/or joint effusion may guide additional imaging workup. Radiopaque foreign bodies can be detected on radiographs depending on their composition.
Ultrasound
At present, musculoskeletal ultrasound (US) is not commonly used in the evaluation of musculoskeletal injuries to the pediatric patient. However, in recent years, its use is gaining popularity because it can complement radiography in select cases and may add important information about soft tissue, bony, and cartilaginous injuries in children.4
A main advantage of US is the real-time dynamic assessment of the injured area without ionizing radiation. Also, because sedation is not usually required, US may be an alternative to magnetic resonance imaging (MRI) in very young pediatric patients who would otherwise have to undergo an MRI with sedation or anesthesia. Portability and rapid acquisition of images obtained at the bedside are other attractive features of US in the pediatric trauma patient.
High-frequency linear transducers (7.5 to 15 MHz) are typically used to assess superficial musculoskeletal structures. Lower frequency curved or vector transducers can be used to increase tissue penetration and improve visualization of deeper structures, especially in a child with a large body habitus. For demonstrating large continuous areas of anatomy, extended field-of-view software is useful. The split-screen function can provide side-by-side comparisons of the affected and normal contralateral sides. Such comparison is often valuable in situations where a finding is subtle in the symptomatic side. Color, power, and pulsed Doppler techniques are useful for assessing alterations of blood flow to injured tissue such as muscular hematomas and reactive synovitis.
US can be used for evaluation of fractures as well as injuries involving the soft tissues, tendons, and ligaments in the setting of trauma. Evaluation of fractures may be limited with US; however, an unsuspected fracture may be detected incidentally when US is used for assessment of adjacent soft tissue injury. US can detect disruption of ligaments and tendons that are superficially located. In addition, radial head dislocation, posterior shoulder subluxation, and upper extremity birth trauma are other potential clinical scenarios where US may be beneficial.4,5,6,7,8,9 Furthermore, when a radiopaque foreign body such as wood is suspected, a targeted US may identify the foreign body or the soft tissue reaction around it.9
Computed Tomography
Although a powerful imaging tool, multidetector computed tomography (MDCT) should be used judiciously because of the ionizing effects to the radiosensitive child.10 MDCT with multiplanar reformation (MPR) and three-dimensional (3D) imaging offers diagnostic advantages over radiographs in areas of complex orthopedic injury.11 MDCT can define or exclude a fracture that is occult or equivocal on radiographs. The administration of contrast media may be indicated when concomitant vascular injury is suspected.11,12
MDCT allows for faster scan speeds and thinner collimation, resulting in submillimeter slice thickness. Thin-slice volume acquisition of data enables isotropic voxels resulting in excellent spatial resolution and multiplanar reformation without degradation in imaging quality. Rapid acquisition decreases the need for sedation and minimizes motion artifact in the pediatric patient who may have difficulties for remaining motionless. Scan parameters depend on whether high detail is necessary for small areas of anatomy or if large areas of anatomy are to be scanned. Specific scan parameters for imaging the musculoskeletal system include 100 kVp, range of 25 to 200 mA, and scan time of 0.5 s/rotation.13 Radiation dose reduction techniques are rapidly evolving, and frequent revision of scan parameters and imaging protocols is recommended to ensure compliance with the principle of as low as reasonable achievable (ALARA).
The degree of displacement and relationship of fracture fragments influence the decision for surgical management. Multiplanar 2D and 3D CT reformations can define the relationship of fracture planes to the joint space and growth plate. On occasion, pathologic fractures through underlying bony lesions can be better characterized with MDCT. Fracture healing and complications of fractures, such as bony bars, are well depicted on MDCT.11 However, the evaluation of soft tissue structures, such as ligaments, muscles, and tendons, is limited with MDCT and is best achieved with US or MRI.
Magnetic Resonance Imaging
MRI is a powerful imaging tool for the evaluation of musculoskeletal trauma. It provides excellent contrast resolution, superior depiction of soft tissue structures, and visualization of hyaline cartilage without ionizing radiation. In the acute setting, MRI can identify radiographically occult injuries such as osseous contusions, chondral and osteochondral fractures, and tendon and ligamentous injuries.14,15 In the subacute and chronic setting, MRI can assess for complications such as growth plate arrest or superimposed infection.
For MRI techniques, the pediatric patient should be placed in a comfortable position with passive restraints applied to the region of interest to minimize motion artifacts. A body coil may be used when a large field of view is needed. However, when possible, a phased array coil or surface coil, which can be optimally fit into the area of interest and provide better quality MR images, should be used. The main MR pulse sequences currently used for evaluating musculoskeletal injuries include T1-weighted, inversion recovery (STIR), fast spin-echo T2-weighted, gradient-echo, and proton density sequences.
Inversion recovery (STIR) sequences are the most sensitive for detecting abnormal bone marrow signal due to trauma. Fast spin-echo T2-weighted sequences are also sensitive to detect abnormal marrow signal, but incomplete fat suppression may occur, potentially mimicking pathology. Gradientecho sequences can be employed to evaluate cartilage injuries. Proton density sequences are helpful to evaluate ligaments and
tendons. Intravenous contrast material is not routinely administered in the setting of acute trauma. However, it is useful for evaluating complications of trauma such as infections.
tendons. Intravenous contrast material is not routinely administered in the setting of acute trauma. However, it is useful for evaluating complications of trauma such as infections.
Nuclear Medicine
Bone scintigraphy, also known as “bone scan,” is performed after the injection of bone-seeking radiotracers such as Tc-99m disphosphonates or 18-labeled sodium fluoride (18F-NaF). Planar, pinhole, SPECT, SPECT-CR, or PET-CT images are typically obtained. The role of bone scintigraphy in the setting of musculoskeletal trauma is somewhat limited, particularly in the pediatric population. Typical indications include the detection of occult fractures, stress injury, fracture healing, and bone fragment viability.16,17,18,19,20 When orthopedic hardware limits fracture assessment on radiographs, bone scintigraphy may be performed as an alternative method of assessing healing. Hardware does not interfere with bone scintigraphy. The two types of nonunion—hypervascular and avascular—can be readily differentiated with a bone scan. Bone scintigraphy has been used in the postoperative setting following bone graft to assess bone graft viability.21 For the detection of stress reaction, it is important to recognize that bone scintigraphy, once the gold standard, is highly sensitive but lacks specificity.
Correlation with contemporaneous anatomic studies often adds clinically useful diagnostic information. The functional information provided by bone scintigraphy can be complementary to the anatomic information from radiography, CT, or MRI.
Fluoroscopy
Fluoroscopically guided studies, which use real-time moving images of the internal structures, are often provided to orthopedic surgery colleagues during operative reduction of misaligned fractures. Fluoroscopy offers real-time guidance for the surgeon during orthopedic hardware placement.22 Similarly, fluoroscopy can also help guide closed reduction of fractures prior to cast placement.
SPECTRUM OF PEDIATRIC FRACTURES
Physeal Fractures (Salter-Harris Fractures)
The presence of growth plates in children results in patterns of injuries different from those of adults. Growth plates or physes contribute to the longitudinal growth of long bones. Therefore, physeal injuries can result in growth disturbances. Trauma to the physis has important therapeutic and prognostic implications. Physeal injuries occur in 21% to 30% of pediatric long bone fractures.23
Although there are several classification systems to characterize a fracture involving the growth plate,24 the most widely accepted is the Salter-Harris classification system (Schematic P), which enables an effective method of communication among health care professionals.25 This classification system grades fractures as type I through V according to the risk increase for complications such as growth arrest. A type I fracture is a transverse fracture through the growth plate, with the fracture line traversing the zone of hypertrophic calcification. The epiphysis may separate from the intact metaphysis, or radiographs may be unremarkable (Fig. 24.1). The type II fracture is the most common growth plate injury accounting for ˜75% of physeal fractures26 (Fig. 24.2). The fracture plane involves a
portion of the metaphysis and then propagates though the physis. The type III fracture involves a portion of the physis with the fracture line exiting the epiphysis into the articular surface (Fig. 24.3). A type IV fracture has an intra-articular fracture line through the epiphysis, physis, and metaphysis. The type V fracture is a crush injury to the growth plate and is the least common type. Fractures in the lower extremity usually have a worse prognosis than do those in other locations.24,27
portion of the metaphysis and then propagates though the physis. The type III fracture involves a portion of the physis with the fracture line exiting the epiphysis into the articular surface (Fig. 24.3). A type IV fracture has an intra-articular fracture line through the epiphysis, physis, and metaphysis. The type V fracture is a crush injury to the growth plate and is the least common type. Fractures in the lower extremity usually have a worse prognosis than do those in other locations.24,27
Accidental Trauma
Musculoskeletal injuries of the appendicular skeleton by location is presented below (Schematics I and II).
 |
 |
 |
Appendicular Skeleton
Upper Extremities
Long Bones
Humerus
Proximal Humeral Fracture. Fractures of the proximal humerus are uncommon injuries and may occur at any age.26,28 In newborns, the proximal humerus is the second most common site of birth trauma following clavicle fractures. The underlying mechanism of injury is rotation and hyperextension of the upper extremity during birth.29,30 Fractures of the proximal humerus may also occur in both accidental and nonaccidental trauma. In children who ambulate, fractures of the proximal humerus are often sustained because of fall onto an outstretched arm or a direct blow to the lateral aspect of the shoulder girdle. A mechanism not consistent with the injury observed should alert the clinician of possible child abuse. The proximal humeral metaphysis is a common location for underlying bony lesions such as bone cysts, and therefore, pathologic fractures may coexist with minor trauma (Fig. 24.4).
Infants and toddlers more often sustain Salter-Harris type I fracture through the physis. In infants, the proximal humeral epiphysis may not be ossified or may be only partially ossified. As such, radiographic findings may mimic a shoulder dislocation because displacement of the metaphysis may be the only finding. Because the relationship of the humeral epiphysis and glenoid is not visible, one may falsely attribute inferior displacement of the humeral metaphysis to
a dislocation rather than to an epiphyseal separation. US and MRI are particularly useful in this setting in order to directly visualize the nonossified epiphysis and define its relationship with the metaphysis.4,31 Proximal humeral fractures in older children are more commonly Salter-Harris type II fractures with variable degrees of displacement. Other Salter-Harris fractures occur less frequently (Fig. 24.5). Buckle fractures (discussed in detail below) can also occur in the proximal humeral metaphysis, in a fashion similar to that of the distal radius. Acute avulsion fracture of the lesser tuberosity is rare in adolescents and may cause disability if not recognized in a timely manner.
a dislocation rather than to an epiphyseal separation. US and MRI are particularly useful in this setting in order to directly visualize the nonossified epiphysis and define its relationship with the metaphysis.4,31 Proximal humeral fractures in older children are more commonly Salter-Harris type II fractures with variable degrees of displacement. Other Salter-Harris fractures occur less frequently (Fig. 24.5). Buckle fractures (discussed in detail below) can also occur in the proximal humeral metaphysis, in a fashion similar to that of the distal radius. Acute avulsion fracture of the lesser tuberosity is rare in adolescents and may cause disability if not recognized in a timely manner.
The majority of the proximal humeral fractures with minimal displacement are treated nonoperatively given their high remodeling potential.32 However, humeral fractures with substantial displacement often require surgical reduction.
Midshaft Humeral Fracture. Fractures to the midshaft of the humerus are uncommon in the pediatric population. Transverse or oblique fractures typically occur because of direct impact, whereas spiral fractures usually require a torsional force. Comminuted fractures require high-energy forces and are often seen with motor vehicle accidents (MVAs) and are sometimes associated with other injuries. Displacement of fracture fragments depends on the fracture alignment with the adjacent musculotendinous attachment. In fractures located proximal to the attachment of the pectoralis major muscle, the proximal fracture fragment is abducted and rotated by the rotator cuff, and the distal fragment is adducted and pulled proximally by the deltoid and pectoralis major muscles. When the fracture line is located between the insertions of the pectoralis major and the deltoid muscles, the proximal fragment is adducted and the distal fragment is pulled up and outward by the deltoid muscle. Fractures distal to the deltoid muscle result in abduction of the proximal fragment.33 Because of the high remodeling capability of the humerus, most humeral shaft fractures are managed nonoperatively, and affected pediatric patients typically recuperate without associated complications.
Distal Humeral Fracture. The supracondylar fracture of the distal humerus is the most common pediatric elbow fracture and accounts for ˜60% of elbow fractures.33 The mechanism of injury is usually a fall onto an outstretched hand with the elbow in extension. The axial load of the child is transmitted to the olecranon process of the ulna, which impinges the posterior aspect of the distal humerus leading to a fracture. The olecranon fossa is the thinnest and weakest portion of the distal humerus, likely accounting for the frequency of this injury.34,35,36 A minority of distal humeral fractures result from a direct blow to a flexed elbow.37 There is a wide range of severity of supracondylar fractures ranging from radiographically occult fracture lines to markedly displaced and angulated fractures.
Radiographs are usually sufficient to diagnose a supracondylar fracture. A minimum of two views is obtained, which include an AP projection view and a true lateral view with the elbow in 90 degrees of flexion. The evaluation of the anterior humeral line is a helpful guideline to assess for a supracondylar fracture. On a well-positioned lateral radiograph of the elbow, a line drawn tangential to the anterior cortex of the humerus should bisect the middle third of the capitellum. In the setting of a fracture, there is usually posterior angulation of the distal fracture fragment, and the anterior humeral line course through the anterior aspect of the capitellum or anterior to the capitellum38 (Fig. 24.6). Lateral radiographs
degraded by suboptimal positioning may falsely reassure, therefore underscoring the importance to critically assess the technical quality of the examination. In some instances, a fracture line is not seen, but there is a joint effusion raising the concern for an underlying occult fracture. Short-interval follow-up radiographs (10 to 14 days) can confirm the presence of a nondisplaced fracture by identifying the fracture line or showing healing in the form of periosteal new bone formation. In these instances, there is usually a joint effusion but no fracture line is identifiable.
degraded by suboptimal positioning may falsely reassure, therefore underscoring the importance to critically assess the technical quality of the examination. In some instances, a fracture line is not seen, but there is a joint effusion raising the concern for an underlying occult fracture. Short-interval follow-up radiographs (10 to 14 days) can confirm the presence of a nondisplaced fracture by identifying the fracture line or showing healing in the form of periosteal new bone formation. In these instances, there is usually a joint effusion but no fracture line is identifiable.
The Gartland classification (Schematic B) describes supracondylar fractures based on the degree of separation of the fractured fragments.39 Type I is a nondisplaced or minimally displaced fracture, typically treated with casting. Type II involves the anterior cortex with dorsal angulation, but an intact posterior cortex, resulting in partial displacement. Type III is a fracture involving the anterior and posterior cortex (i.e., no cortical contiguity) resulting in full displacement40 (Fig. 24.7). The majority of type II and type III fractures are treated with percutaneous pin fixation and casting. Open reduction may be performed if closed reduction does not achieve satisfactory results.35,37,40 Complications of humeral supracondylar fractures are rare but include neurovascular injuries to the brachial artery or median nerve, compartment syndrome, Volkmann contracture, and cubitus varus.
Medial Epicondylar Fracture. Fractures of the medial epicondyle of the distal humerus represent ˜10% of all pediatric elbow fractures. They occur in a slightly older age group, typically 7 to 15 years old, than pediatric patients sustaining supracondylar or lateral condylar fractures.37,41,42,43 They are considered Salter-Harris type III or IV fractures and are extra-articular. The mechanism of injury is a valgus stress causing avulsion of the medial epicondyle from the attachment of the forearm flexors and supinators. This injury can occur in isolation or in association with an elbow dislocation.43,44 Isolated fractures occur in the setting of overuse in overhead-throwing athletes. Throwing athletes can sustain either an acute fracture or a chronic overuse injury from the valgus loading and distraction associated with the throwing motion. In the setting of elbow dislocation, the radius and ulna are usually displaced posteriorly, and there is a high incidence of associated medial epicondyle fractures.
Understanding the orderly progression of the appearance of the elbow ossification centers is important when assessing a pediatric patient with a medial epicondyle fracture. The ossification of the medial epicondyle typically occurs at 6 to 7 years of age and should be accounted for in this age group. Furthermore, when an ossification center is seen in the expected location of the trochlea, but a medial epicondyle ossification center is not present, then a displaced intraarticular avulsion fracture of the medial epicondyle should be suggested37 (Fig. 24.8).
Entrapped intra-articular fractures require reduction. Open reduction and screw fixation are indicated if closed reduction is unsuccessful.44 Nonincarcerated fractures that are displaced by >5 mm are usually treated surgically and those that are distracted by ≤5 mm are treated nonoperatively.45
Lateral Condylar Fracture. The lateral condylar fracture is the second most common pediatric elbow fracture. This injury accounts for 10% to 15% of the elbow fractures and usually occurs in children 6 to 10 years of age.42 The mechanism of injury includes varus force applied to a hyperextended elbow.46 Affected pediatric patients usually present with pain but lack the deformity typically seen with supracondylar fractures. Missed or delayed diagnosis of these fractures can often lead to a high incidence of nonunion or malunion.
Nondisplaced lateral condylar fractures of the distal humerus can be difficult to detect radiographically, with only a subtle fracture line abutting the margin of the metaphysis (Fig. 24.9). An internal oblique view most accurately shows a fracture line and displacement. Typically, there is an associated hemarthrosis with visualization of the posterior fat pad and elevation of the anterior fat pad. US and/or MRI examinations of the elbow can assess for fractures involving the cartilaginous epiphysis.
Lateral condylar fractures are usually Salter-Harris type II fractures involving the metaphysis of the lateral condyle extending to the physis. Less frequently, lateral condylar fractures can be Salter-Harris type IV intra-articular fractures with the fracture line coursing through the capitellum (Fig. 24.10). The Milch classification system (Schematic A) is used to characterize the location of the distal fracture line.47 The Milch type I fractures involve the capitellum, and the fracture line exists lateral to the capitellotrochlear groove. In contrast, the Milch type II fractures exit medial to the capitellotrochlear groove and involve the cartilaginous trochlea.34,37
Nondisplaced fractures are usually treated conservatively with a posterior splint. More than 2 mm displacement of the lateral epicondyle is an indication for operative management.48,49
Physeal Fracture. Distal humeral growth plate fractures are uncommon injuries seen in the setting of birth trauma, accidental trauma, and child abuse. A transphyseal fracture of the distal humerus generally occurs in patients 2 to 3 years old before the distal humeral ossification center appears.50,51 This fracture can be mistaken for an elbow dislocation because the displacement of the ossified distal humerus metaphysis is malaligned in relation to the radius and ulna. In the case of a dislocation, the radiocapitellar congruency is not maintained. US can be useful in evaluating elbow fractures by visualizing the fracture through the nonossified cartilaginous epiphysis.52 Displaced fractures are treated with closed reduction and pinning.37
Radius
Proximal Radial Fracture. Fractures of the radial head and neck account for ˜4% to 5% of the pediatric elbow fractures.34 Affected children usually present with point tenderness over the radial head and lateral elbow pain with pronation and supination. The mechanism is a fall onto an outstretched hand with an extended elbow and associated valgus force.42 The proximal radius impacts the capitellum and results in a fracture. Proximal radius fractures are usually Salter-Harris type II, with type I fracture being much less common. In contrast to adults, radial neck fractures are more common in pediatric patients than are radial head fractures.53 Up to half of patients with proximal radial fractures have associated
ligamentous injury and fractures of the medial epicondyle, olecranon, and proximal ulna.
ligamentous injury and fractures of the medial epicondyle, olecranon, and proximal ulna.
The findings of a proximal radial fracture on radiographs may be subtle presenting with only mild contour abnormality of the metaphysis (Fig. 24.11). A radiocapitellar view may be helpful to diagnose subtle proximal radial fractures. The O’Brien classification system (Schematic D) is used to quantify the degree of angulation.54 Type I is <30 degrees; type II is between 30 and 60 degrees; and type III is >60 degrees of angulation (Fig. 24.12).
Treatment of radial head or neck osseous injures depends on the degree of angulation. Less than 30 degrees of angulation is acceptable, and these injuries are usually treated conservatively with a cast or a long arm splint. Angulation between 30 and 60 degrees is controversial with regard to open or closed reduction management. With angulation of >60 degrees, operative reduction is required.55
Distal Radial Fracture. Fractures of the distal radius are common, accounting for 25% of the pediatric fractures.56,57,58,59 Children are at increased risk because of the rapidly growing skeletal structures and because of their increased level of activity. During rapid longitudinal growth, the mineralization is unable to keep up with the bone growth and makes the skeleton susceptible to fractures.60 Additionally, some authors suggest that bones prior to the adolescent growth spurt are relatively more porous, which may also contribute to the higher fracture risk.61 The incidence of distal radial fractures in the United States is increasing, which may be due to increased participation of sports when children fall onto an outstretched hand.62 Boys more commonly sustain distal radius fractures than do girls.62,63,64,65,66
On radiographs, a distal radial fracture with displacement, which is usually dorsal in direction, is relatively easy to diagnose. However, the “torus” fracture of the distal radius, which manifests as a subtle contour abnormality (“buckle”) along the compression side of the cortex most often involving the metaphysis, can be often overlooked and missed (Fig. 24.13). The lateral view or additional oblique views of the wrist may be helpful. Such views can distinguish a “torus” fracture from
a “greenstick” injury, which comprises a bend in the bone on one side and a visible break in the bone cortex on the other side. Details on these fractures are available at the end of the appendicular skeleton part of this chapter.
a “greenstick” injury, which comprises a bend in the bone on one side and a visible break in the bone cortex on the other side. Details on these fractures are available at the end of the appendicular skeleton part of this chapter.
 FIGURE 24.13 Torus fracture in a 2-year-old boy. Frontal radiograph of the wrist shows contour abnormality (arrows) of the distal radius consistent with a torus fracture. |
Operative treatment for distal radial fractures is rarely indicated because of the ability of the growing skeleton to remodel in the pediatric population. Most distal radial fractures heal with casting and immobilization. Orthopedists advocate closed reduction of distal radial fractures when there is complete displacement, >1 cm of shortening because of bayonet apposition or >15 degrees of angulation.67
Galeazzi Fracture. Galeazzi fracture (Schematic E) is a fracture of the distal radius, usually involving the diaphysis, with associated subluxation or dislocation of the distal radioulnar joint (DRUJ).68 The incidence of Galeazzi fractures in children is 0.3% to 2.7% of all forearm fractures.68,69 The radial fracture typically occurs 4 to 5 cm proximal to the DRUJ. If the radial fracture is <7.5 cm from the articular surface, there is a high incidence of instability of the DRUJ. Galeazzi fractures are seen during a high-energy impact such as MVA or fall from a height onto an outstretched hand with hyperpronation of the forearm.
On frontal radiographs, an angulated radial diaphyseal fracture with shortening of radius and widening of the space between the radius and ulna is seen. On the lateral view, there is dorsal displacement of the ulna with respect to the radius.
In order to restore the alignment and function, open reduction and internal fixation of the radius fracture and reduction and stabilization of the DRUJ is often performed although conservative management with good outcomes has been also reported in pediatric patients.70 Previous studies have shown that nonoperative management of Galeazzi fracture is associated with increased risk of complications such as malunion of the fracture and residual subluxation of the DRUJ.71
Ulna
Olecranon Fracture. Olecranon fractures constitute ˜4% to 7% of pediatric elbow fractures. These fractures are uncommon because of the relatively short size and higher strength of the olecranon compared to the distal humerus. The mechanism of injury is a fall onto an outstretched hand or direct impact to the posterior elbow.72 Stress injury to the olecranon due to overuse has been reported in overhead-throwing adolescent athletes. Avulsion-type fractures occur from strong pull of the triceps. Olecranon fractures are often associated with other elbow injuries such as fractures of the medial or lateral condyle, radial neck, and supracondylar region and may also occur in association with radial head dislocation.72
Radiographically, fractures involving the olecranon can be longitudinal, horizontal, or obliquely oriented. These fractures are best evaluated on a true lateral view of the elbow. The fracture may involve the growth plate of the apophysis or the articular surface.53 It is important to recognize that there is a variable appearance of the olecranon apophysis, which can sometimes simulate a true fracture. Similarly, the growth plate can mimic a nondisplaced fracture. In these situations, obtaining a comparison view of the contralateral asymptomatic side elbow may be beneficial for differentiation (Fig. 24.14).
Nondisplaced or minimally displaced fractures of the olecranon are treated with immobilization for 4 to 6 weeks, whereas displaced fractures require surgical fixation with pins, wires, screws, or plates.73
Monteggia Fracture. The Monteggia fracture represents a dislocation of the radial head with an associated proximal ulna fracture. Typically, the apex of the ulnar fracture and the direction of the radial dislocation are the same. This injury occurs in children who fall on an outstretched hand with the forearm in excessive pronation. The Bado classification (Schematic F) categorizes Monteggia fractures based on the displacement of the radial head.74 Type I (extension type) is the most common, with ulnar fracture and anterior dislocation of the radial head75,76 (Fig. 24.15). Type II (flexion type) is characterized by the ulnar fracture and posterior or posterolateral dislocation of the radial head. Type III (lateral type) describes the ulnar fracture and posterior or posterolateral dislocation of the radial head. The type IV (combined type) shows ulnar and radius fractures and anterior dislocation of the radius. Pediatric equivalent Monteggia fracture is a proximal ulnar fracture and a radial head or neck fracture without dislocation of the radial head (Fig. 24.16). In children, one can also see a bowing fracture of the ulna with radial head fracture.77,78
 FIGURE 24.16 Monteggia fracture in a 3-year-old girl. Frontal radiograph of the left elbow shows a proximal ulnar fracture (straight arrow) and an associated radial neck fracture (curved arrow). |
Closed reduction is the first line of management of Monteggia fractures. A recent study of 40 pediatric patients with Monteggia fracture showed that conservative management of Monteggia fractures, when indicated, may result in excellent outcome.79 Open reduction with internal fixation is reserved for complicated cases or when closed reduction fails.
Hands
Hand fractures (Schematic I) are relatively common in the pediatric population. In comparison to other bone fractures, the incidence of epiphyseal injury is 34% higher than reported elsewhere in the skeletal system in children.80 Although the majority of hand fractures heal without complication, potentially problematic hand fractures include displaced intra-articular fractures, Salter-Harris type I distal phalangeal fractures due to crushing injuries, and open fractures.
Mallet Finger. The mallet finger, also known as “baseball finger” or “dropped finger,” is the most common tendon injury of the hand that typically occurs during sport activities in children. The injury is characterized by avulsion of the bony or ligamentous attachment of the extensor mechanism to the distal phalanx. This injury occurs when the distal finger is “jammed” or struck against an object. Other mechanisms include a direct blow or a hyperextension injury.81,82 Affected pediatric patients usually present with pain and soft tissue swelling at the dorsum of the finger with inability to extend the distal interphalangeal joint (DIP).83
The small triangular avulsed bone fragment at the dorsal aspect of the distal phalanx near the DIP joint is best seen in lateral radiographs of the finger (Fig. 24.17). The distal phalanx may be fixed in flexion because of deficiency of the extensor tendon and unopposed action of the flexor tendon.
Cross-sectional imaging is usually not necessary. However, sagittal MR images can detect injuries to the extensor tendon when no bony injury is present.83
Cross-sectional imaging is usually not necessary. However, sagittal MR images can detect injuries to the extensor tendon when no bony injury is present.83
Fractures involving less than one-third of the joint surface may be treated nonoperatively with splint immobilization of the finger in extension.81,84 Greater than 50% of joint surface involvement is often treated surgically.85,86 Failure to treat a mallet finger in a timely manner may result in a “swan-neck” deformity or early secondary osteoarthritis (Fig. 24.18). A chronic mallet finger with permanent deformity requires surgical management.87
Boxer Fracture. The “boxer fracture” is a transverse fracture through the neck of the metacarpal, with apex dorsal angulation and external rotation of the distal fragment. The fifth metacarpal is most often affected. The mechanism of injury is typically a direct blow of the clenched fist against a hard object. Physical examination findings include point tenderness, swelling, and ecchymosis suggesting an underlying fracture. Loss of contour of the knuckle may be seen because of angulation of the fracture fragment.
Radiographs are usually diagnostic for detecting a boxer fracture. The AP radiograph usually shows a fracture line and foreshortening of the affected metacarpal. The lateral view demonstrates the typical volar angulation of the distal fracture fragment88 (Fig. 24.19).
The management depends on the degree of fracture angulation. The fourth and fifth metacarpals can tolerate a greater degree of angulation compared to the second and third metacarpals. Less than 40 degrees of angulation of the fourth and fifth metacarpal is generally acceptable. Nonoperative management includes splinting with or without closed reduction.89
First Metacarpal Fractures. Bennett and Rolando fractures are intra-articular metacarpal fractures/dislocations of the thumb. In the Bennett fracture, there is dorsal and radial dislocation of the distal fragment by the abductor pollicis longus muscle, whereas in the Rolando fracture, bone comminution is noted (Fig. 24.20). Note is made of the fact that both Bennett and Rolando fractures typically require open reduction and internal fixation.
Skier Thumb. The “skier thumb” is a fracture of the base of the proximal phalanx of the thumb with disruption of the ulnar collateral ligament (Fig. 24.21). This type of fracture is commonly seen in children whose thumbs are stressed by entrapment in a ski pole handle during alpine skiing.
 FIGURE 24.20 Rolando fracture in a 16-year-old boy. Oblique radiograph of the thumb demonstrates a comminuted intra-articular fracture (arrow) involving the base of the thumb. |
Scaphoid Fracture. The scaphoid is the most commonly fractured carpal bone, accounting for 3% of hand and carpal bone fractures in pediatric patients.90,91
Affected children often complain of radial-sided wrist pain after falling onto an outstretched hand. On physical examination, there is point tenderness elicited in the anatomic snuffbox and diminished range of motion with wrist flexion and extension. Scaphoid fractures can be classified by anatomic location, based on whether they involve the proximal pole, waist (midportion), or distal pole.91 The scaphoid waist is the most common location (Fig. 24.22).
A complete assessment of scaphoid fracture requires AP, lateral, and scaphoid views. A 30-degree ulnar deviated AP radiograph of the wrist, which is also known as “scaphoid view,” is particularly helpful for the detection of subtle and nondisplaced fractures. In addition to fracture line detection, displacement or obliteration of the navicular fat stripe often associated with scaphoid fracture may be seen on radiographs. Although radiographs usually are the initial imaging study for evaluation of clinically suspected scaphoid fractures, radiographs may be unremarkable in the acute setting in 13% to 30% of cases.90,92 MDCT or MRI can detect scaphoid fractures when clinical suspicion is high and radiographs are normal (Fig. 24.23).
The current management of scaphoid fractures is cast immobilization for a nondisplaced fracture and internal fixation for a displaced fracture with more than 1 mm step-off or angulation.86 Because of the tenuous blood supply of the proximal pole of the scaphoid, nonunion and avascular necrosis are two common complications in patients with delayed diagnosis.
Kienbock Disease. Although lunate fractures are rare, avascular necrosis of the lunate secondary to trauma can cause lunatomalacia or Kienbock disease.
Dislocations
Among various osseous dislocations that occur in the pediatric population, radial head, humeral head, and patella are the three most common bones prone to dislocation.
Nursemaid Elbow. Nursemaid elbow or pulled elbow (Schematic C) is anterior subluxation or dislocation of the radial head in relation to the capitellum. The annular ligament, which holds the radial head in place, may be disrupted or displaced in this injury. The mechanism of injury is longitudinal traction of an extended elbow while in supination. This may occur when caretakers are attempting to pull a child away from something or lifting a child by the hands during play.93 Children aged between 6 months and 3 years are most commonly affected. Affected children present with pain, a telltale history, and the arm is often held in flexion and pronation.
Imaging is not usually necessary because of the classic history but can be useful in excluding possible underling osseous fracture. Often, by the time the requested radiographs are obtained for evaluation, the radial head may be already relocated within the capitellum because the radiographer often reduces the subluxation or dislocation while supinating the patient’s elbow for the AP view acquisition.53 Sonographic findings may show widening of the radiocapitellar joint, increase joint echogenicity, interposition of the displaced annular ligament between the capitellum and the radial head, and the edge of a torn annular ligament.
Shoulder Dislocation. Shoulder dislocation is characterized by dissociation of the humeral head from the glenoid fossa. The shoulder is the most commonly dislocated joint in the body, and the four different types include anterior, posterior, inferior, and superior (Schematic G).
Anterior dislocations are the most common, accounting for over 95% of all cases.94 The mechanism of injury of an anterior dislocation includes a direct blow to the arm that is abducted, externally rotated, and extended at the time of impact. Direct trauma to the posterior humerus and a fall onto an outstretched arm may also result in anterior shoulder dislocation. Posterior dislocations are uncommon, accounting for 2% to 4% of shoulder dislocations.95 They may be caused by violent muscle contraction during seizure activity, electrocution, or electroconvulsive shock therapy.96 A direct anterior blow to the anterior aspect of the humerus or axial loading of an adducted and internally rotated arm can result in posterior shoulder dislocation. Inferior dislocation, also known as luxatio erecta, is the least common type and is caused by axial loading of an abducted arm. Conditions that predispose pediatric patients to shoulder dislocation include connective tissue disorders that result in ligamentous laxity, such as Ehlers-Danlos syndrome and Marfan syndrome, and glenoid dysplasia.
When shoulder dislocation is suspected, plain radiographs of the shoulder in the AP, transcapular, and axillary projections should be obtained. In anterior dislocation, the AP view demonstrates loss of congruency of the humeral head with the glenoid fossa, and the humerus lies in a subcoracoid position with the greater tuberosity abutting the anterior glenoid rim (Fig. 24.24). The transcapular view shows the humeral head displaced medial to the scapula. Posterior dislocations can be subtle on radiographs and are underdiagnosed in up to 50% of cases.97 The AP view shows widening of the glenohumeral distance of >6 mm, humeral head fixed in internal rotation (“lightbulb” sign), and compression fracture of the anteromedial humeral head (“trough line” sign). On the transcapular view, the humeral head can be seen displaced posteriorly with respect to the scapula. With inferior dislocation, the extremity is held over the head in a fixed position and the humeral head is seen beneath the coracoid process.
Postreduction radiographs are typically performed to assess for successful repositioning and to evaluate for concomitant fractures. Associated fractures following an anterior dislocation include Hill-Sachs deformity, bony Bankart lesions, and greater tuberosity fractures (Schematic G). A Hill-Sachs deformity is a cortical depression in the superolateral humeral head created by impaction with the inferior glenoid rim. Bony Bankart lesions are avulsions fractures of the anteroinferior glenoid rim. With posterior dislocation, a “reverse Hill-Sachs” deformity can occur in the medial humeral head.
MR imaging in shoulder instability is useful to demonstrate pathology in the osseous, cartilaginous, ligamentous, and labral structures (Schematic G). MR criteria for labral
tears include increased signal within the substance of the labrum that extends to the surface of the labrum (Fig. 24.25). Secondary findings include paralabral cysts, periosteal stripping, and bony injuries commonly seen with labral tears such as Hill-Sachs and bony Bankart lesions. In Hill-Sachs deformity, there is cortical depression of the superolateral humeral head. Associated bone marrow edema is seen in the acute setting. MRI is also useful to assess the integrity of the hyaline cartilage of the glenohumeral joint. The Bankart lesion describes a tear of the anteroinferior labrum with associated tear of the anterior periosteum. MR arthrogram may be helpful for detection and characterization of labrum and glenohumeral ligaments injuries. CT is useful to detect a shoulder dislocation that is subtle on radiographs and for preoperative planning.
tears include increased signal within the substance of the labrum that extends to the surface of the labrum (Fig. 24.25). Secondary findings include paralabral cysts, periosteal stripping, and bony injuries commonly seen with labral tears such as Hill-Sachs and bony Bankart lesions. In Hill-Sachs deformity, there is cortical depression of the superolateral humeral head. Associated bone marrow edema is seen in the acute setting. MRI is also useful to assess the integrity of the hyaline cartilage of the glenohumeral joint. The Bankart lesion describes a tear of the anteroinferior labrum with associated tear of the anterior periosteum. MR arthrogram may be helpful for detection and characterization of labrum and glenohumeral ligaments injuries. CT is useful to detect a shoulder dislocation that is subtle on radiographs and for preoperative planning.
Management includes reduction of the dislocation followed by immobilization and physical therapy. Operative treatment is reserved for irreducible dislocations, displaced fractures, and labral tears.
Lower Extremities
Long Bones
Femur. Pediatric femur fractures can be subdivided into fractures of the proximal femur (hip), femoral shaft, and distal femur. Classification schemes for each location exist and help guide treatment and prognosis. Many important differences exist between pediatric and adult femur fractures. For example, pediatric fractures heal rapidly and remodel quickly because of abundant vascularity and properties of the periosteum. In the pediatric population, high-energy trauma is typically required to cause proximal femur fractures, whereas elderly adults can sustain hip fractures with relatively minor trauma. The presence of growth plates results in injuries unique to the immature skeleton. Additionally, growth plate injuries may predispose children to growth disturbances and angular deformities. In contrast to adult patients with multiple trauma and femur fractures, the risk of pulmonary complications such as fat embolism in children is lower.
Proximal Femur Fracture. Hip or proximal femur fractures are much less common in children than in adults and account for <1% of all pediatric fractures.98,99,100,101 Early detection and treatment of proximal femur fractures are critical because of the risk of femoral head avascular necrosis.
The Delbet classification (Schematic T) divides pediatric hip fractures into four types.102 Type I is a transepiphyseal fracture with a transverse fracture through the proximal physis. Type IA is without dislocation and type IB is with dislocation. These fractures occur most frequently in infants, often resulting from difficult birth delivery. Type I fractures have the worst prognosis and highest association of avascular necrosis. Type II is called the transcervical type and is the most common, accounting for 40% to 50% of hip fractures.98,100,101,103,104,105,106,107 The fracture line traverses the midfemoral neck. Type III is termed cervicotrochanteric with the fracture line occurring through the base of the femoral neck. Type IV fractures are intertrochanteric and have the best outcome. As the name implies, the fracture line occurs in between the greater and lesser trochanters. If the fracture line involves the greater trochanter, premature closure of the apophysis may occur and subsequent coxa valga deformity.
Treatment of proximal femur fracture is emergent decompression of the intracapsular hematoma and reduction of displaced fracture fragments.
Femoral Shaft Fracture. The femur is the largest bone in the body and one of the most common long bones fractured in children. Femoral fractures are the most common cause for hospitalization in pediatric orthopedic injuries.108 Epidemiologic studies have shown a bimodal age distribution with regard to peak incidence of femoral shaft fractures. There is an early peak in the toddler age group with falls being the most common underlying mechanism of injury. The second peak occurs in adolescence when motor vehicle trauma is the most common cause. Because of the strength of the femur, usually a high-energy force is required to result in a fracture. Up to 30% of femur shaft fractures in pediatric patients <3 years may be the result of child abuse.109 Conditions that may predispose a pediatric patient to a femur fracture include osteogenesis imperfecta, as well as additional causes of osteopenia such as cerebral palsy, spina bifida, and other neuromuscular disorders.41,110,111,112,113
Femoral shaft fractures can be open, with breach of the soft tissues, or closed with intact soft tissues. The Gustilo classification system (Schematic Q) is the most commonly accepted classification of open fractures.114 Type I is an open
fracture with a clean wound and a wound size smaller than 1 cm in length. Type II is an open fracture with a wound >1 cm in length but without extensive soft tissue damage, flaps, or avulsions. Type III is a greater degree of soft tissue damage characterized by extensive laceration, damage, or soft tissue loss. Included in type III injuries are fractures requiring vascular repair and fractures that have been open for 8 hours prior to treatment.
fracture with a clean wound and a wound size smaller than 1 cm in length. Type II is an open fracture with a wound >1 cm in length but without extensive soft tissue damage, flaps, or avulsions. Type III is a greater degree of soft tissue damage characterized by extensive laceration, damage, or soft tissue loss. Included in type III injuries are fractures requiring vascular repair and fractures that have been open for 8 hours prior to treatment.
Typically, prophylactic antibiotics are administered to all open fractures to prevent osteomyelitis. Gustilo type I and II fractures are treated with immediate intramedullary nail fixation. Grade III fractures with arterial injuries are treated with external fixation. For unstable patients, amputation may be lifesaving.
Distal Femur Fracture. Fractures of the distal end of the femur (Schematic M) are less common than are shaft fractures and account for ˜12% to 18% of all pediatric femur fractures.41,108 Boys are more commonly affected than are girls. Common underlying mechanisms of injury include MVAs, pedestrians struck by a vehicle, sports injuries, and sometimes child abuse. Affected pediatric patients typically present with pain, swelling, and inability to bear weight. Concomitant vascular compromise may occur because of injury of the femoral artery. Therefore, a careful neurovascular physical examination is important in the setting of distal femur fractures.
Distal femur fractures are classified as supracondylar or physeal (condylar or intercondylar). Supracondylar fractures are more common in infants and young children, whereas physeal fractures occur more frequently in older children and adolescents. On radiographs, supracondylar fractures are located in the distal femoral metaphysis and do not extend into the growth plate. These fractures are typically transversely oriented and have varying degrees of displacement. Physeal fractures are classified according to the Salter-Harris classification system (previously described) (Schematic P).
Growth disturbance and leg length discrepancies are common complications of distal femur fractures in the pediatric population. A large meta-analysis study reported growth arrest in up to 50% of physeal fractures of the distal femur. Of these, 22% had leg length discrepancy of >1.5 cm.115 In another large series of physeal fractures, the incidence of distal femur fractures was low, accounting for 1.4% of all injuries; however, 25% of these developed physeal bone bridge formation.116 A large central bone bridge is the most common pattern of growth arrest in the distal femur.117 Distal femur fractures are typically treated with immobilization and closed reduction of the displaced or angulated fractures.
Patellar Sleeve Fracture. Patellar sleeve avulsion is the most common patellar fracture of the growing skeleton, accounting for 1% of all pediatric fractures.118 It is caused by cartilage avulsion from the lower pole of the patella from forceful contraction of the quadriceps muscle against a partially flexed knee. A “sleeve” of periosteum is pulled off the patella and continues to form bone if not treated, thus enlarging or even duplicating the patella (Fig. 24.26) (Schematic L).
This fracture usually prompts surgical reduction with internal fixation of the patellar tendon.118
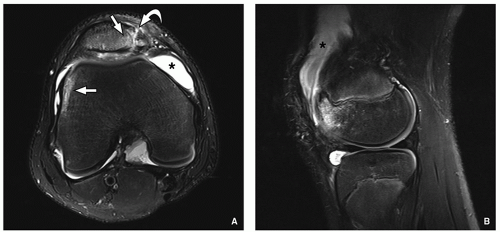
Patellar Dislocation. Lateral patellar dislocation is a relatively common injury that can occur in the setting of direct trauma. This injury occurs more commonly in active adolescent females.119 The mechanism of injury in transient lateral patellar dislocation is either a direct medial blow to the knee while the knee is in mild flexion, typically <30 degrees, or, alternatively, a valgus angulation and twisting with the knee in mild flexion, which can also result in lateral dislocation (Schematic L).
Lateral patellar dislocation can occur in pediatric patients with variant anatomy that predisposes to maltracking of the patella in the trochlear groove. Risk factors include patella alta, trochlear dysplasia, and excessive lateral position of the tibial tubercle.120 The Insall-Salvati index (Schematic J) is commonly used to assess patella alta, an important predisposing factor that leads to decreased contact of the patella and instability.121 The length of the patellar tendon divided by the length of the patella should normally be <1.3. If the Insall-Salvati index is >1.3, patella alta is suggested. Morphologic features of trochlear dysplasia that are associated with patellar dislocation include flattening or convexity of the joint surface, shallow femoral sulcus, lateral trochlear inclination,
and trochlear facet asymmetry.122 Excessive lateralization of the tibial tubercle in relation to the femoral sulcus can also predispose a patient to lateral dislocation.
and trochlear facet asymmetry.122 Excessive lateralization of the tibial tubercle in relation to the femoral sulcus can also predispose a patient to lateral dislocation.
In the setting of suspected patellar dislocation, plain radiographs of the knee should be acquired in the AP and lateral planes as well as with sunrise and tunnel views. The position of the patella is assessed in relation to the trochlea on all views and may be laterally positioned.123 The sunrise view may demonstrate an avulsion fracture fragment adjacent to the medial pole of the patella. On the lateral view, patella alta or superior location of the patella may be seen, a finding that suggests patellar maltracking. Soft tissue swelling and a joint effusion are nonspecific but may be present after patellar dislocation. Note that ˜50% to 75% of patellar dislocations are occult and therefore not correctly diagnosed at the time of the initial clinical and radiography evaluation.124
MRI is valuable in pediatric patients particularly with recurrent or complicated patellofemoral dislocation. Bone contusions in the medial pole of the patella and anterolateral aspect of the lateral femoral condyle are characteristic of a recent patellar dislocation on MRI (Fig. 24.27). Bone contusion on the lateral femoral condyle is due to the impact of the patella on the femur that occurs during spontaneous relocation. Other frequently encountered findings associated with patellar dislocation include (1) chondral fractures at either the inferomedial patella or the lateral weight-bearing surface of the femur, (2) medial retinaculum and medial patellofemoral ligament injury, and (3) partial- and full-thickness tearing at both the patellar and femoral attachment sites. In addition, in comparison to adults, medial patellar sleeve avulsion fractures are common in children in the setting of patellar dislocation due to the relative weakness of the osteochondral junction.
Conservative management consisting of appropriate rest as well as hip and thigh muscle strengthening exercise may be sufficient for pediatric patients with spontaneously relocated patellar dislocation without fracture or loose fragment. Surgical treatment such as lessening lateral tension and tightening medical restraint after removal of loose fragment may be necessary in recurrent or complicated patellar dislocation.