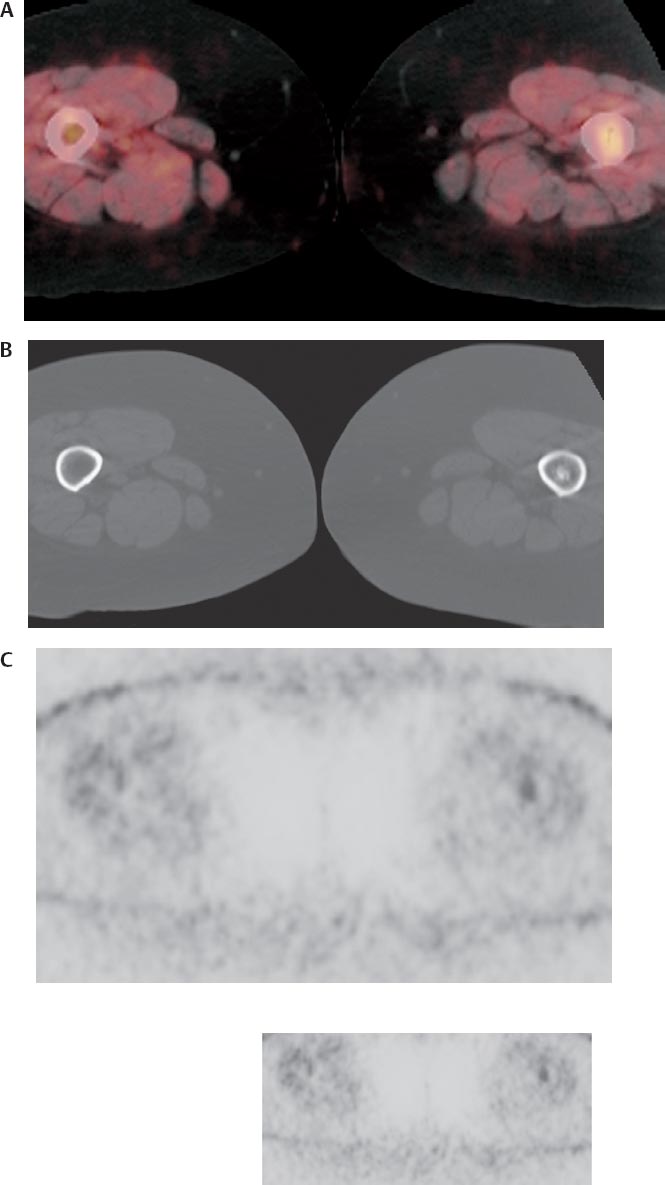
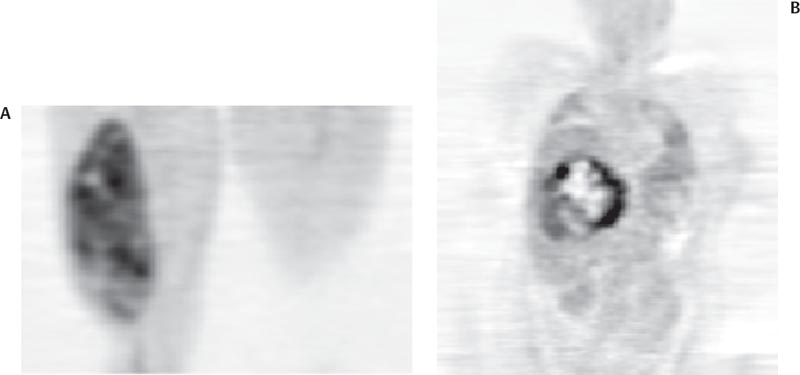
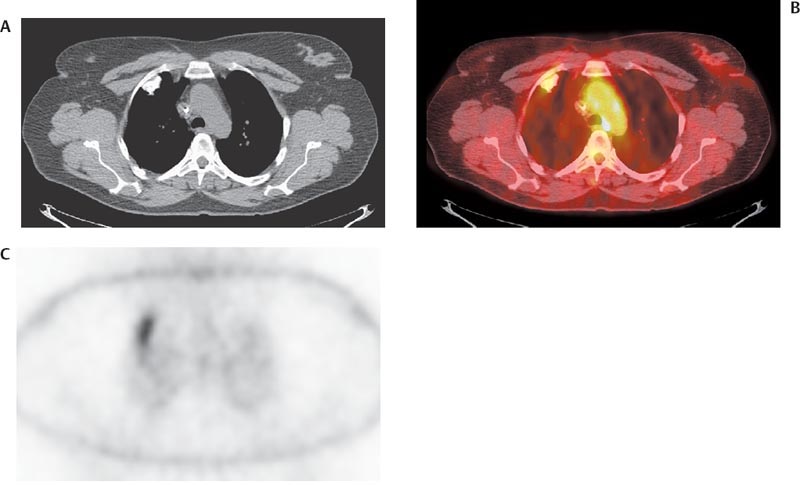
25 In a known bone or soft tissue lesion, positron emission tomography (PET) is of some value in determining whether the lesion is benign or malignant and in grading malignant lesions. In addition, bone or soft tissue lesions are detected incidentally on PET performed for other indications. The degree of fluorodeoxyglucose (FDG) uptake in the lesion can aid in differential diagnosis when correlated with conventional imaging modalities. Fig. 25.3 Liposarcomas. Coronal positron emission tomography (PET) scans demonstrate fluorodeoxyglucose uptake in liposarcomas in the (A) thigh and (B) abdomen. The abdominal liposarcoma is heterogeneous with a standardized uptake value (SUV) of 11.7, consistent with a poor prognosis tumor. Given the heterogeneity of uptake, the PET scan would be helpful in guiding biopsy. The thigh liposarcoma has a much lower SUV of 2.7, consistent with a better prognosis tumor. However, there is some degree of heterogeneity, suggesting myxoid degeneration and a poorer prognosis than might be predicted by the SUV alone. (Courtesy of Janet Eary, MD, Seattle, WA.) PET is valuable in both osseous and soft tissue malignancies. The primary uses are staging, guiding biopsy, detecting recurrence, therapy response, and tumor grading. The primary applications of PET are in guiding biopsy, therapy monitoring, and diagnosing local recurrence. Fig. 25.4 Osteosarcoma lung metastasis. (A) Computed tomography (CT) scan in a patient with osteosarcoma demonstrates a calcified right upper lobe lesion. (B) Axial positron emission tomography (PET)/CT scan demonstrates uptake in this lesion consistent with metastasis. (C) In this case, it is important to review the nonattenuation-corrected image to determine that the uptake is not artifactual secondary to the increased density of the lesion. Although PET can detect lung metastases from osteosarcoma, CT is more sensitive for this purpose.
Musculoskeletal Tumors
Eugene C. Lin and Abass Alavi
 Distinguishing Benign from Malignant Musculoskeletal Tumors
Distinguishing Benign from Malignant Musculoskeletal Tumors
Benign versus Malignant Bone Tumors
Clinical Indication: C
Accuracy
Pearls
Pitfalls
Benign versus Malignant Soft Tissue Tumors
Clinical Indication: C
Accuracy
Pearls and Pitfalls
 Evaluation of Known Musculoskeletal Tumors
Evaluation of Known Musculoskeletal Tumors
Osteosarcoma and Soft Tissue Sarcomas14,15
Clinical Indication: B
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine