CHAPTER SEVEN Musculoskeletal
PEDIATRIC OBESITY
It has been well reported in the lay press that pediatric obesity has reached epidemic proportions. It is estimated that somewhere between one fifth and one third of children in the United States are obese; pediatric obesity is also becoming a worldwide trend. If you consider which pediatric diseases are common and which cause significant morbidity and mortality in adulthood, pediatric obesity may well be the number one pediatric health concern. Obesity is a multiorgan system problem, but because it is a disease of the soft tissues, it is included here in the musculoskeletal chapter.
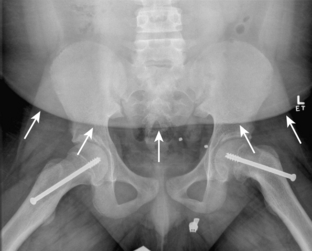
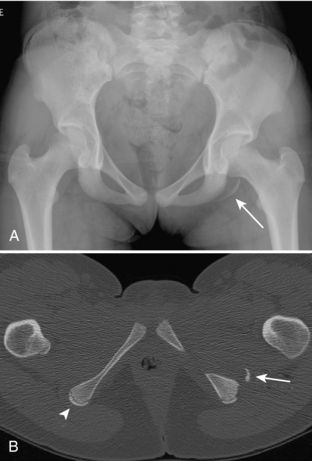
Pediatric obesity has a well-documented association with several diseases of childhood such as slipped capital femoral epiphysis (Fig. 7-1) but is also associated with a host of other potential problems, including: psychosocial problems (poor self-esteem, depression); glucose intolerance/type 2 diabetes (the frequency of pediatric type 2 diabetes has increased 100 times in the past 20 years in Cincinnati); hyperlipidemia; steatohepatitis; cholelithiasis; obstructive sleep apnea; hypertension; and pulmonary embolism. Many of these traditionally adult disorders are now being encountered in obese children. Perhaps most concerning, approximately 80% of obese children will go on to be obese adults and have all of the associated morbidity.
NORMAL VARIANTS AND COMMON BENIGN ENTITIES
Probably more than in any other organ system, the normal imaging appearance of the skeletal system is strikingly different in children from its appearance in adults (Fig. 7-2A-D). This is related to the changing appearance of growing and maturing bone. The most striking changes occur in the vicinity of physes and apophyses. Many of the more common mistakes made in pediatric skeletal radiology are related to the misinterpretation of normal structures as being abnormal. Textbooks are dedicated to the normal radiographic appearances and variations of bones in children. The details of the normal changes in the radiographic appearance throughout the maturing skeleton cannot be covered here. The following section describes several normal variants and commonly encountered benign entities.
Apophyseal Irregularity
In the growing child, apophyses in various parts of the body can have variable and often somewhat irregular appearances. Separate ossicles of an apophysis can mimic fragments, irregularity can mimic periosteal reaction, and mixed sclerosis and lucency can be confused with findings of an inflammatory or neoplastic process. Common apophyses that may have this appearance include tibial tuberosity, ischeal tuberosity, ischeal pubic synchondrosis, and posterior calcaneal apophysis (Fig. 7-3A-C). Irregularity and fragmentation are commonly seen in the normal tibial tuberosity. The calcaneal apophysis can often demonstrate a strikingly sclerotic appearance. The ischeal pubic synchondrosis can appear very prominent and asymmetric.
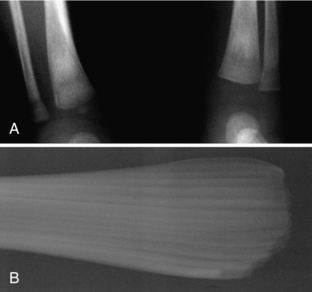
Distal Femoral Metaphyseal Irregularity
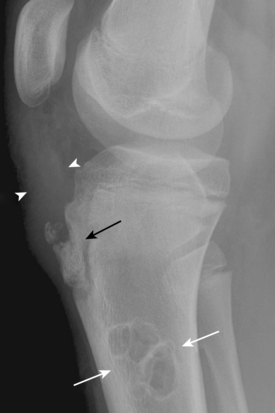
Distal femoral metaphyseal irregularity, also referred to as cortical desmoid and cortical irregularity syndrome, refers to the presence of irregular cortical margination and associated lucency involving the posteromedial aspect of the distal femoral metaphysis. It occurs in as many as 11% of boys aged 10 to 15 years. Although debated, its presence is thought to be related to chronic avulsion at the insertion of the adductor magnus muscle. Although this lesion can be associated with pain, it is often discovered incidentally, and its significance lies in its alarming radiographic appearance. On radiography, there is cortical irregularity present along the posteromedial cortex of the distal femoral metaphysis, best seen on the lateral view (Fig. 7-4A-C). On frontal radiographs, there may be an associated lucency (see Fig. 7-4). Familiarity with the typical location, appearance, and patient age is important so that these lesions are not confused with aggressive malignancies. Because the lesions are often bilateral, confirmation of their benign nature can be made by demonstrating a similar lesion on radiographs of the opposite knee. In problematic cases, computed tomography (CT) or magnetic resonance imaging (MRI) can be used to demonstrate the characteristic findings: a characteristic scooplike defect with an irregular but intact cortex; no associated soft tissue mass; and sometimes a subtle contralateral lesion (see Fig. 7-4).
Benign Cortical Defects
Benign cortical defects, or nonossifying fibromas, are commonly encountered lesions of no clinical significance. They are seen in as many as 40% of children at some time during development and are most common between 5 and 6 years of age. The term nonossifying fibroma is typically reserved for larger lesions. They occur most commonly within the bones around the knee, particularly the distal femur. They appear as lucent, eccentric, well-defined lesions with thin cortical rims (Fig. 7-5) and are typically round or oval. Over time they become more sclerotic and eventually resolve. When the characteristic pattern is identified, no further imaging or follow-up is necessary.
TRAUMA
Fractures in children differ from those in adults for multiple reasons. Children’s bones are more pliable and have a greater propensity to deform prior to breaking. Therefore, incomplete fractures are more common in children than adults. The incomplete fracture may be purely a bowing type of fracture (Fig. 7-6), may be associated with a buckling of the cortex on the concave margin of the bowing (torus fracture), or may demonstrate an incomplete fracture along the cortex of the convex margin of the bowing (greenstick fracture; see Fig. 7-6). Buckle fractures may be subtle and may appear only as an increase in acute angulation of a normally gentler curve (Fig. 7-7).
Involvement of the Physis
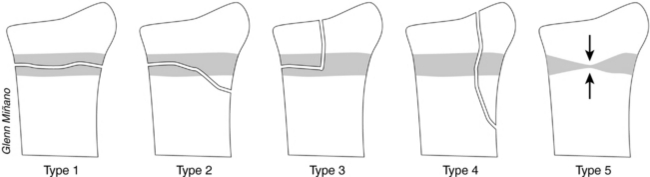
One of the potential problematic issues with fractures in children is involvement of the physis. The physis is involved in as many as 18% of pediatric long bone fractures. Physeal involvement may result in growth arrest of that limb and in a higher rate of necessary internal fixation. The standard classification for physeal fractures is that by Salter and Harris. It divides fractures into five types according to whether there is involvement of the physis, epiphysis, or metaphysis, as determined by radiography (Fig. 7-8). Fractures with higher numbers have a greater incidence of complications. Type 1 fractures involve only the physis. They tend to occur in children younger than 5 years of age. On radiography, the epiphysis may appear to be displaced in comparison to the metaphysis. However, type 1 fractures often reduce prior to the radiograph’s being obtained, and the only imaging finding will be soft tissue swelling adjacent to the physis. Type 2 fractures involve the metaphysis and the physis but do not involve the epiphysis (Fig. 7-9A, B). They are the most common type of physeal injury (up to 75%). On radiography, there is typically a triangular fragment of bony metaphysis attached to the physis and epiphysis. Type 3 fractures involve the physis and epiphysis but not the metaphysis (see Fig. 7-9). Type 3 injuries have a greater predisposition for growth arrest. Type 4 injuries involve the epiphysis, physis, and metaphysis and, like type 3 injuries, are associated with a high rate of growth arrest. Type 5 fractures consist of a crush injury to part of or all of the physis. Posttraumatic growth arrest may be detected radiographically by demonstration of a bony bridge across the physis.
Commonly Encountered Fractures by Anatomic Location
WRIST
The wrist is the most common fracture site in children. Most fractures of the distal forearm are buckle or transverse fractures of the distal metaphysis of the radius, with or without fracture of the distal metaphysis of the ulna (see Figs. 7-7, 7-9). However, the distal radius is also the most common area of physeal fracture (28% of physeal injuries occur in the distal radius). Displacement or obliteration of the pronator fat pad indicates a fracture or deep soft tissue injury. The normal pronator fat pad is visualized on a lateral view of the forearm as a thin line of fat with a mildly convex border. In most distal forearm fractures, the convexity of the pronator fat pad is increased or the fat pad becomes obliterated by soft tissue attenuation.
ELBOW
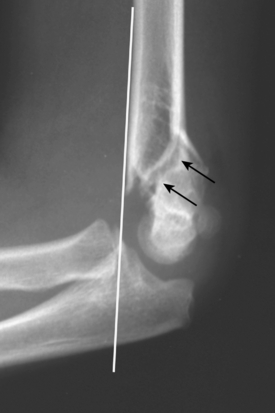
There are several unusual features that make elbow injuries in children different from those in adults. In contrast to adults, in whom fracture of the radial neck is the most common injury, children most commonly experience supracondylar fractures. They usually occur secondary to hyperextension that occurs when falling on an out-stretched arm. As many as 25% of such fractures are incomplete and may be subtle on radiography. On radiographs, there can be posterior displacement of the distal fragment such that a line drawn down the anterior cortex of the humerus (anterior humeral line) no longer bisects the middle third of the capitellum (Fig. 7-10). The fracture line is usually best seen through the anterior cortex of the distal humerus on the lateral view (see Fig. 7-10). A joint effusion is typically evident. Elbow effusions are identified when there is displacement of the posterior fat pad, resulting in its visualization on a lateral view (Fig. 7-11A, B). Normally, the posterior fat pad rests within the olecranon fossa and is not visible on a true lateral view of the elbow. The anterior fat pad, which is often visible normally, may become prominent and have a prominent apex anterior convexity.
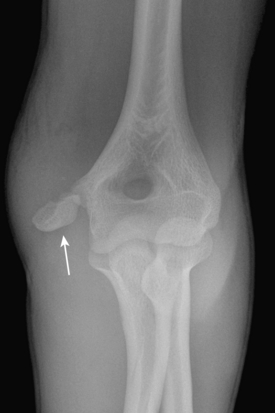
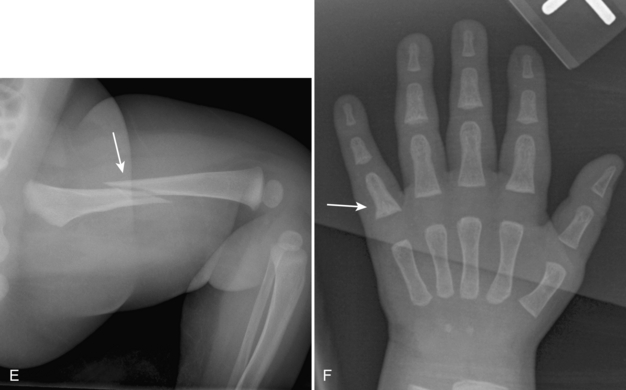
Other elbow injuries include fractures of the lateral condyle (Fig. 7-12) and avulsion of the medial epicondyle (Little League elbow; Fig. 7-13). With avulsion of the medial epicondyle (10% of elbow injuries), the medial epicondyle may become displaced. To avoid mistaking the displaced apophysis for one of the other ossicles of the elbow, it is important to know the predictable order of ossification of the elbow ossification centers. The order can be remembered by the mnemonic CRITOEcal (capitellum, radial head, internal epicondyle, trochlea, olecranon, external epicondyle). Whenever there is a fracture of the forearm, it is important to evaluate the radial-capitellar joint for potential dislocation of the radial head. The radial head should align with the capitellum. If it does not, radial head dislocation should be suspected (Fig. 7-14).

FIGURE 7-12. Fracture of the lateral condyle. Radiograph shows avulsed sliver of bone (arrows) arising from lateral condyle.
Toddler’s Fracture
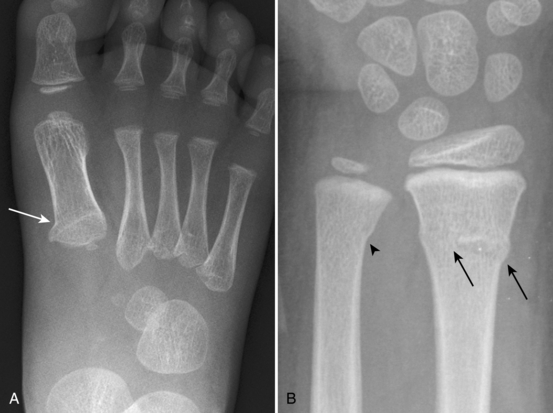
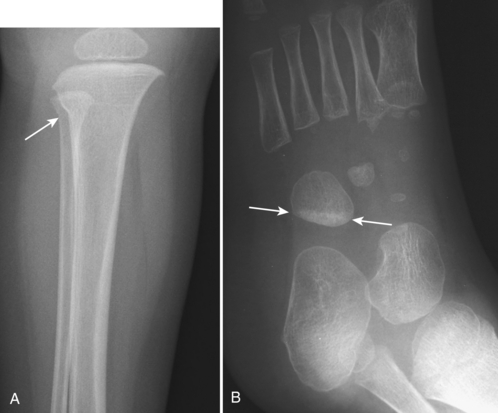
When a child first begins to walk, a nondisplaced oblique or spiral fracture of the midshaft of the tibia can occur (Fig. 7-15). Such an injury is common and is referred to as a toddler’s fracture. Most children present with failure to continue to walk or refusal to bear weight on that extremity. Oblique views often demonstrate the fracture better than do frontal or lateral views. Toddlers can also suffer from similar types of fractures involving the proximal anterior tibia, calcaneus, or cuboid (Fig. 7-16A, B).

FIGURE 7-15. Toddler’s fracture. Radiographs show subtle oblique, nondisplaced fracture (arrows) through proximal tibial shaft.
Avulsion Fractures in Adolescents
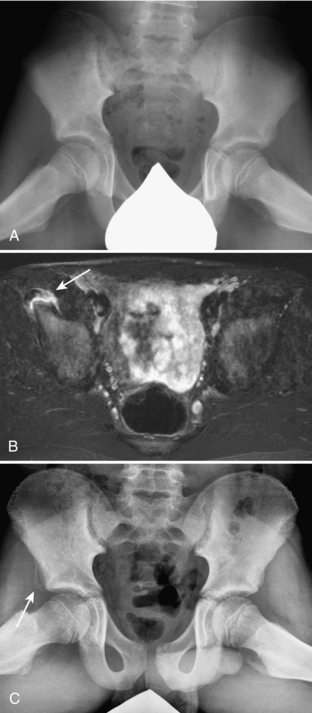
Radiologists may encounter findings of chronic avulsion when patients are imaged for pain or incidentally when imaging is performed for other reasons. The irregularity and periostitis that can be associated with chronic avulsions should not be misinterpreted as suspicious for malignancy. In addition, if unwarranted biopsies of these areas are performed, the histologic changes associated with the healing callus of the avulsion injury may be misinterpreted as malignancy. The most common sites of avulsion occur within the pelvis, where muscles capable of great force attach. Sites at which apophyseal avulsions most commonly occur, along with the associated muscular attachments, are the iliac crest (transversalis, internal oblique abdominalis, external oblique abdominalis); the anterior superior iliac spine (sartorius); the anteroinferior iliac spine (rectus femoris; Fig. 7-17A-C); the ischial apophysis (hamstring muscles: biceps femoris, gracilis, semimembranosus, semitendinosus; Fig. 7-18A, B); and the lesser trochanter (iliopsoas). The radiographic findings of avulsion injuries include displacement of the ossified apophysis from normal position and variable, and often exuberant, amounts of associated periosteal new bone formation.
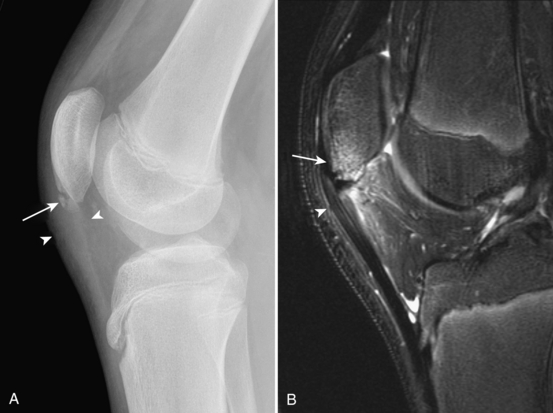
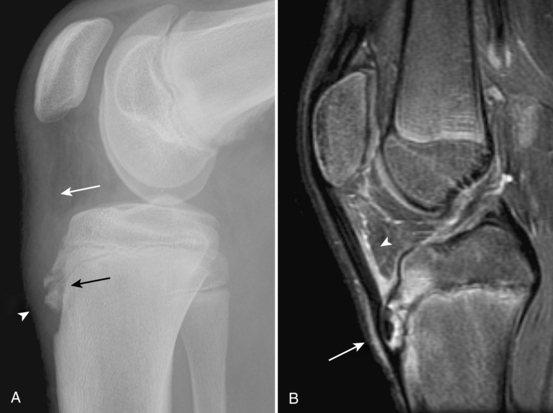
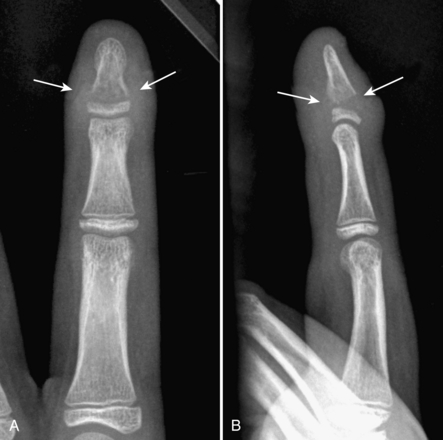
The extensor mechanism of the knee consists of the quadriceps femoris muscles, the quadriceps tendon, the patella, the patellar tendon, and the patellar tendon insertion on the tibial tuberosity; this mechanism can also be involved by avulsion injuries. Chronic avulsion of the patellar tendon at its attachment to the patella is called Sinding-Larsen-Johansson syndrome. It occurs most commonly in children between the ages of 10 and 14 years of age. Symptoms include localized pain and swelling over the inferior aspect of the patella associated with restricted knee motion. Radiography demonstrates irregular bony fragments at the inferior margin of the patella associated with adjacent soft tissue swelling and thickening and indistinctness of the patellar tendon (Fig. 7-19A, B). Chronic avulsive injury of the patellar tendon at its inferior attachment is referred to as Osgood-Schlatter lesion (tibial tuberosity avulsion). It is a common disorder that most often affects active adolescent boys. Symptoms include pain and swelling over the tibial tuberosity. Radiography demonstrates bony fragmentation of the tibial tuberosity, associated adjacent soft tissue swelling, and thickening and indistinctness of the patellar tendon (Fig. 7-20A, B; and see Fig. 7-5).
Child Abuse
Child abuse, also referred to as the more politically correct and less graphic nonaccidental trauma, is unfortunately common. It is estimated that more than 1 million children are seriously injured and 5000 killed secondary to abuse each year in the United States alone. Most of the children are less than 1 year of age and almost all are less than 6 years of age. When clinical or imaging findings are suspicious for potential abuse, a radiographic skeletal survey is typically obtained. The purpose of the skeletal survey is to document the presence of findings of abuse for legal reasons so that the child can be removed from exposure to the abuser. Other tests sometimes used include a repeat skeletal survey after approximately 2 weeks to look for healing injuries not seen on the initial skeletal survey, skeletal scintigraphy, abdominal CT, and MRI of the brain. The identification and reporting of findings of child abuse by the radiologist is an important task. False-positive cases can cause a nonabused child to be removed from his or her family, whereas false-negative cases can result in a child’s returning to a potentially life-threatening environment.
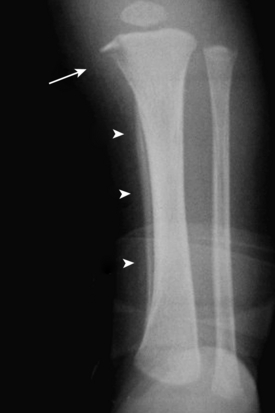
The radiographic findings of abuse vary in their specificity. One of the highly specific findings is the presence of posterior rib fractures occurring near the costovertebral joints (Fig. 7-21A-F). These are thought to occur when an adult squeezes an infant’s thorax. Such rib fractures may be subtle prior to development of callus formation. The evaluation for rib fractures should be a routine part of the evaluation of the chest radiograph of any infant. Another finding that is highly specific for abuse is the metaphyseal corner fracture (see Fig. 7-21). This fracture extends through the primary spongiosa of the metaphysis, the weakest portion, and usually occurs secondary to forceful pulling of an extremity. The broken metaphyseal rim appears as a corner fracture (a triangular piece of bone) when seen tangentially or as a crescentic rim of bone (referred to as a bucket-handle fracture) when seen obliquely. Other fractures associated with abuse include those of the scapula, spinous process, and sternum. Spiral long bone fractures in nonambulatory children are also highly suspicious. Multiple fractures in children of various ages (some with callus and some acute) as well as multiple fractures of various body parts are highly suspicious for abuse (see Fig. 7-21). In fact, any fracture in an infant should be viewed with suspicion, because as many as 30% of fractures in infants are secondary to abuse. Extraskeletal findings seen in abuse include acute or chronic subdural hematoma, cerebral edema (asphyxia), intraparenchymal brain hematoma, lung contusion, duodenal hematoma, solid abdominal organ laceration, and pancreatitis.
PERIOSTEAL REACTION IN THE NEWBORN
When periosteal reaction is encountered in a newborn, there are a number of entities that must be considered (Table 7-1). They include physiologic new bone formation; TORCH infections (osteomyelitis), prostaglandin therapy; Caffey disease; metastatic neuroblastoma; and abuse. Physiologic periosteal new bone formation is commonly seen in infants during the first few months of life. It typically involves rapidly growing long bones, such as the femur, tibia, and humerus. Differential features that support physiologic growth as the cause of periosteal reaction include symmetric distribution, benign appearance of the periosteal reaction, and appropriate age of the child. When periosteal reaction involves the femur, tibia, or humerus, the other three bones are usually involved too. Radiographs may show one or several dense lines of periosteal reaction paralleling the cortex of the diaphysis of the long bones. Neonates with congenital heart disease are commonly treated with prostaglandins to maintain patency of the ductus venosus; these children commonly demonstrate prominent periosteal reaction.
Table 7-1. Differential Diagnosis for Periosteal Reaction in a Newborn
| Physiologic growth |
| TORCH infections |
| Syphilis, rubella |
| Prostaglandin therapy |
| Caffey disease (infantile cortical hyperostosis) |
| Neuroblastoma metastasis |
| Abuse |
TORCH Infections
CONGENITAL RUBELLA SYNDROME
Rubella is the most common of the transplacental viral infections. Its features include eye abnormalities, deafness, hepatosplenomegaly, aortic and pulmonic stenosis, and intrauterine growth retardation. Bony changes are present in as many as 50% of cases. They include irregular fraying of the metaphyses of long bones and generalized lucency of the metaphyses. The findings have been likened to a celery-stalk appearance (Fig. 7-22). These radiographic findings are most apparent during the first few weeks of life. The bony manifestations of rubella are currently extremely rare.
SYPHILIS
Congenital syphilis occurs secondary to transplacental infection, usually occurring during the second or third trimester. Clinical findings include hepatosplenomegaly, rash, rhinorrhea, anemia, and ascites. Bony changes are present in as many as 95% of patients but often do not appear until 6 to 8 weeks after the time of infection. The radiographic findings may be present before the blood serology turns positive. Findings include nonspecific metaphyseal lucent bands and periosteal reaction involving multiple long bones (Fig. 7-23). The Wimberger corner sign is the most specific finding of syphilis and consists of destruction of the medial portion of the proximal metaphysis of the tibia, resulting in an area of irregular lucency (see Fig. 7-23). Bony manifestations of syphilis are much more commonly encountered than those of rubella or other TORCH infections.
Caffey Disease (Infantile Cortical Hyperostosis)
Caffey disease is an idiopathic syndrome that consists of periosteal reaction shown on radiographs, irritability, fever, and soft tissue swelling over the areas of periosteal reaction. It occurs during the first few months of life. The bones most commonly involved include the mandible, clavicle, ribs, humerus, ulna, femur, scapula, and radius. Imaging shows periosteal new bone formation, sclerosis, and adjacent soft tissue swelling (Fig. 7-24). The disease is self-limited and currently occurs much less commonly than in the past.
LUCENT PERMEATIVE LESIONS IN CHILDREN
A bone lesion is considered permeative when it has ill-defined borders, has a wide zone of transition, and has multiple small, irregular holes centrally. As in an adult, a permeative bone lesion in a child is consistent with an aggressive inflammatory or neoplastic lesion. The finding is nonspecific. The more common causes of a permeative lesion in a child include osteomyelitis, Langerhans cell histiocytosis, neuroblastoma metastasis, Ewing sarcoma, and lymphoma/leukemia. The differential diagnosis can be further limited by considering the patient’s age (Table 7-2). If the patient is younger than 5 years of age, the most likely diagnoses include osteomyelitis, Langerhans cell histiocytosis, and metastatic neuroblastoma. Ewing sarcoma and lymphoma are exceedingly rare in children younger than 5. In older children, Ewing sarcoma and lymphoma/leukemia become candidates, and metastatic neuroblastoma becomes much less likely.
Table 7-2. Differential Diagnosis of a Permeative Bone Lesion in a Child on the Basis of Age
| Less Than 5 years | Greater Than 5 years |
|---|---|
Osteomyelitis
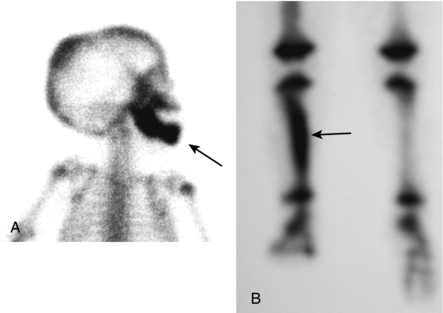
The earliest radiographic finding of osteomyelitis is deep soft tissue swelling evidenced by displacement or obliteration of the fat planes adjacent to a metaphysis. Bony changes may not be present until 10 days after the onset of symptoms. Initial bony changes consist of poorly defined lucency involving a metaphyseal area. Commonly, progressive bony destruction is present (Figs. 7-25A, B; 7-26A-C). Periosteal new bone formation begins at approximately 10 days. Oseteomyelitis can appear as sclerotic, rather than lucent, when it is a chronic process (see Fig. 7-26). Other imaging modalities that are used in the evaluation of suspected osteomyelitis include skeletal scintigraphy, MRI, and occasionally CT. On skeletal scintigraphy, osteomyelitis appears as a focal area of increased activity on the angiographic, soft tissue, and skeletal phase images. Skeletal scintigraphy becomes positive early after the onset of osteomyelitis and is often positive prior to development of changes seen on radiography. Another advantage of scintigraphy is the ability to evaluate for multiple sites of involvement. MRI also demonstrates abnormal findings early after the onset of osteomyelitis. Osteomyelitis appears as an area of increased T2-weighted signal within a metaphysis. There are usually large areas of surrounding edema that are seen as an increased T2-weighted signal within the adjacent bone marrow and soft tissues. Gadolinium administration may show areas of nonenhancement suspicious for necrosis or abscess formation (see Fig. 7-26). Identification of drainable fluid for surgical planning is one of the advantages of MRI over scintigraphy.
Langerhans Cell Histiocytosis
Letterer-Siwe disease is an acute disseminated form of LCH that occurs in children less than 1 year of age. There is acute onset of hepatosplenomegaly, rash, lymphadenopathy, marrow failure, and pulmonary involvement. Skeletal involvement may not be present. The prognosis is poor; most children die within 1 to 2 years.
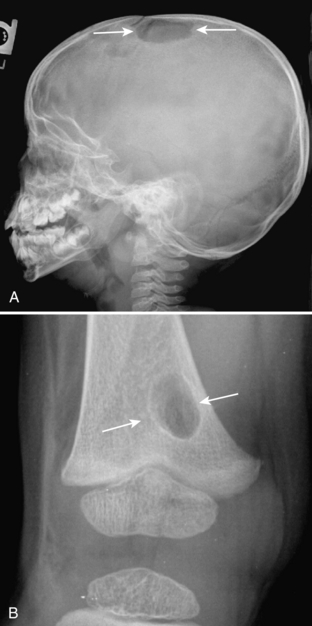
The radiographic appearance of skeletal manifestations of LCH is extremely variable. Lesions may be lucent or sclerotic, may be permeative or geographic, and may have a sclerotic or poorly defined border. The most common sites of LCH, in decreasing order of frequency, are the skull (Fig. 7-27A, B), ribs, femur, pelvis, spine, and mandible. Skull lesions may have a “beveled edge,” which is related to uneven destruction of the inner and outer tables of the skull. Rib lesions may be multiple and commonly have an expanded appearance. When the spine is involved, a classic finding is vertebral plana (vertebral destruction with severe collapse; Fig. 7-28A, B).