Case presentation
A 10-year-old male presents with 2 days of initially intermittent, now constant, abdominal pain. He states that the pain started on the right side of his abdomen and was crampy in quality, although now has become more sharp. The pain has now localized to the right lower quadrant, although he complains of radiation to the umbilicus and the right upper quadrant. He has not had documented fever but his mother states he has “felt warm” and has reported nausea, but no vomiting, diarrhea, dysuria, or back pain. There is no history of trauma.
His examination reveals a somewhat uncomfortable-appearing child with a temperature of 100.1 degrees Fahrenheit, a heart rate of 105 beats per minute, respiratory rate of 18 breaths per minute, and blood pressure of 100/65 mm Hg. He has tenderness to the right lower quadrant and periumbilical areas, with mild voluntary guarding and rebound to the right lower quadrant. He has no hepatosplenomegaly. He has no scrotal or testicular tenderness or edema. You ask him to ambulate, which he does with some discomfort on the right side. Laboratory evaluation shows a white blood cell count (WBC) of 10 Thou/cc mm with 75% neutrophils and 20% lymphocytes. His urinalysis is normal, except for a specific gravity of >1.030.
Imaging considerations
While the diagnosis of appendicitis is ultimately made by a surgeon in the operative suite, imaging plays an important role in determining which patients may require operative intervention. However, equally important is which patients do not require imaging to make the diagnosis of appendicitis. This is based on clinical suspicion, including specific history and physical examination findings. The decision whether to ultimately obtain imaging may be institution dependent and may be influenced by such factors as availability of pediatric surgical consultation and imaging resources. Even in dedicated pediatric emergency departments, there is variation in initial imaging choice, which is influenced by variation in hospital resources.
There are well-validated appendicitis scoring systems that can be used to determine the probability of appendicitis in the pediatric patient, such as the Pediatric Appendicitis Score. There are also recently proposed scoring systems that have utilized new biomarkers in addition to traditional laboratory testing to assist the clinician in determining which patents are at low risk for appendicitis. Patients with a score suggestive of appendicitis may not need imaging; evaluation by a surgeon prior to imaging in these cases may be appropriate.
Limited abdominal ultrasonography (US)
US has become the initial imaging test of choice for the evaluation of pediatric appendicitis. The American College of Radiology Appropriateness Criteria for Right Lower Quadrant Pain-Suspected Appendicitis and the American College of Emergency Physicians both promulgate ultrasound as the initial imaging modality in pediatric patients. , This modality is noninvasive, utilizes no ionizing radiation exposure, is readily available at pediatric centers, and is increasing in use. The reliability of ultrasound in detecting appendicitis has been well documented, with reported sensitivities of around 90% and specificities of 95% when the appendix is clearly visualized. This modality is operator dependent, and skill in pediatric ultrasound is necessary for identification of the appendix and interpretation of the images. A child may not be cooperative for the study, potentially making it difficult to obtain meaningful images. The implementation of a training program at nonpediatric facilities focusing on language, the developmental level of a child, and interaction techniques can make for a productive experience.
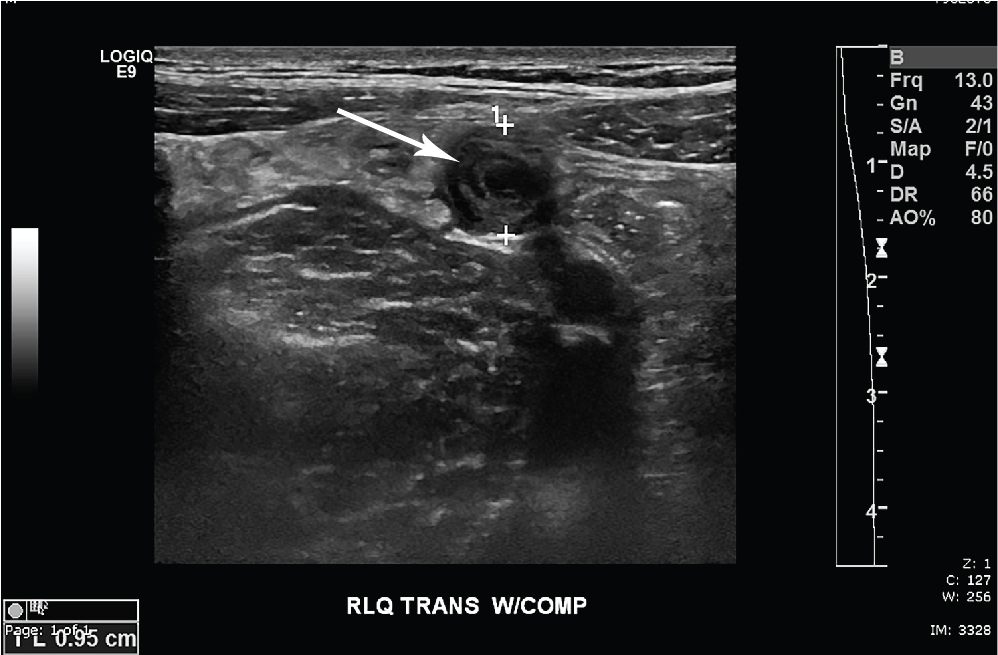
Diagnostic criteria exist for the identification of appendicitis by ultrasound. An appendiceal diameter of greater than 7 mm, a single wall thickness of greater than 2 mm, noncompressibility of the appendix, and the presence of a sonographic “target sign,” with a fluid-filled lumen are each direct indications of appendicitis. , An appendicolith, if present, may be identified. The diameter of the appendix as a sole criterion for detecting appendicitis is not recommended. A negative examination for appendicitis can be either an examination with complete visualization of a normal appearing appendix or an examination with a partially or nonvisualized appendix, with adequate visualization of other right lower quadrant structures and no secondary signs suggestive of appendicitis. Ultrasound may also demonstrate an alternative diagnosis as a cause of the presenting symptoms, such as genitourinary or gastrointestinal tract pathology. Ultrasound results can be equivocal or nondiagnostic. Adequate visualization can be impaired by inadequate compression due to pain or obesity, overlying gas, and retrocecal location of the appendix. If ultrasound is inconclusive and there are indirect findings suggestive of appendicitis, such as surrounding free fluid, and increased echogenicity of mesenteric fat, or a clinical appendicitis score suggestive of appendicitis, then secondary imaging options (such as computed tomography [CT] or magnetic resonance imaging [MRI]) or, in some instances, surgical consultation should be considered. Conversely, lack of these findings with an equivocal ultrasound may warrant observation of the patient with strict return precautions and reevaluation within 24 hours.
Computed tomography
CT has proven to be an excellent imaging modality for diagnosing appendicitis, with reported sensitivities of 93% or greater and specificities of 92% or greater. , CT also can depict other etiologies of abdominal pain, such as colitis, bowel obstruction, ovarian pathology, and urinary calculi, as well as bladder and kidney infection. Anatomical variation of appendix location, as seen with a retrocecal appendix, can also be visualized. Intravenous (IV) contrast is recommended for this study. Although most normal appendices measure 7 mm or less in diameter on CT, a normal appendix can measure greater in diameter. Therefore, diameter should be used cautiously as a diagnostic criterion for appendicitis on CT. As with ultrasound, one should consider other signs of an inflammatory process, such as appendiceal wall thickening, hyperenhancement, periappendiceal inflammation, phlegmon, or abscess.
The current trend and suggested best practice favor CT as a secondary study in suspected uncomplicated appendicitis, with CT considered in patients where the diagnosis of appendicitis is clinically suspected but ultrasound imaging is equivocal or nondiagnostic. However, in facilities where ultrasound is not routinely used to diagnose appendicitis, CT is an acceptable alternative imaging strategy, especially if pediatric surgical consultation is not available. CT is also appropriate in cases where there are suspected intraabdominal complications, such as perforation and abscess. Of course, this modality exposes the patient to ionizing radiation and IV placement is required. Sedation is rarely needed since CT is rapid. If CT imaging is employed, the lowest dose of ionizing radiation needed to achieve visualization and a meaningful study should be used.
Magnetic resonance imaging
MRI has recently been considered as an imaging modality to investigate pediatric appendicitis. Protocols vary and there is no accepted standard protocol for evaluating pediatric appendicitis, but most utilize a rapid-sequence technique and contrast is not always employed, as gadolinium has not been shown to increase diagnostic accuracy in detecting appendicitis. , Reported sensitivity and specificity rates in the pediatric population are approximately 96%. , Findings reported to be consistent with appendicitis include an appendiceal diameter greater than 7 mm, periappendiceal fat infiltration, and restricted diffusion of the appendiceal wall.
MRI has the added advantage of not exposing the patient to ionizing radiation. This, and the apparent accuracy of MRI, makes this an attractive alternative to US and CT imaging. However, this modality is not always readily available, potentially requires sedation for optimal imaging in younger patients, may not be cost-effective at this time, and requires expertise at interpreting a pediatric study. Studies have demonstrated that, in children older than 5 years of age, this modality can be utilized without the need for sedation. , , At this time, most MRIs of appendicitis have been performed in dedicated pediatric facilities; however, a recent study showed magnetic resonance (MR) to be clinically effective when used in a stepwise ultrasound to MR algorithm for imaging for appendicitis in a nonpediatric hospital, with interpretation by nonpediatric radiologists. This study also reported the capability to decrease the MRI examination time for children to 11 minutes.
Imaging findings
This child had graded compression limited abdominal ultrasound imaging of his right lower quadrant. There is a noncompressible, blind-ending tubular structure that measures 10 mm in diameter. Hyperemia is present with some free fluid surrounding the structure. There is no appendicolith ( Fig. 17.1 ). The tip of the appendix is seen with surrounding edema and hyperemia ( Fig. 17.2 ). For comparison, the findings of acute appendicitis on IV-contrast CT from another patient are provided ( Fig. 17.3 ).