Case presentation
An 8-month-old male presents with 2 months of cough and intermittent rhinorrhea. He has been seen multiple times by his primary care provider and has been diagnosed at various times with viral upper respiratory tract infection and acute otitis media, for which he has been prescribed oral antibiotics. He has had some intermittent fevers as well, all of which have resolved after several days. There has been no travel or sick contacts, nor has there been any history of choking or concern for foreign body ingestion.
Physical examination reveals a thin but well-appearing and active child. He is afebrile and his vital signs are unremarkable, except for mild tachypnea (65 breaths per minute). There is no rhinorrhea and the oropharynx is clear. His chest demonstrates decreased breath sounds to the upper left chest, but there are no crackles, retractions, grunting, or stridor. He has a normal abdominal examination.
Imaging considerations
Plain radiography
This imaging modality is the most commonly utilized imaging modality for the neonatal or infant chest. Two views are preferred (anterior-posterior [AP] and lateral) when possible. Plain radiography may suggest the presence of a chest mass, prompting the use of advanced imaging. Ninety percent of chest masses can be visualized by plain radiography.
Plain radiography is the first-line imaging modality when chest masses are suspected. However, this modality may miss small masses, and further imaging is indicated when a mediastinal mass is suspected, since a diagnosis is not usually made by plain radiography alone.
Ultrasound (US)
This imaging modality is increasingly used for the evaluation of specific chest conditions. Examples include pneumothorax, pleural effusion, hemothorax, and chest masses. US of the mediastinum is limited, however, in patients above 5 years of age due to poor acoustic windows. The lack of exposure to ionizing radiation, rapidity, availability, and no need for sedation are all advantages of sonography.
Computed tomography (CT)
This imaging modality is typically utilized when plain radiography is abnormal and further delineation of a suspected chest mass is indicated. CT is also used for surgical planning when indicated. CT is readily available and rapid and usually does not require sedation. CT does include exposure to ionizing radiation, and appropriate pediatric imaging protocols should be utilized to reduce this exposure as much as possible.
CT is often utilized in patients with mediastinal masses. It has been shown to be very accurate for the characterization of masses (such as size and location) and to determine whether there is involvement of adjacent structures. CT can differentiate between cystic and solid structures and can evaluate for the presence of calcification, fat, or vascular components. CT findings have been shown to impact management in 65% of cases and have added additional diagnostic information in 82%. ,
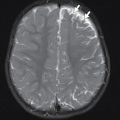
Magnetic resonance imaging (MRI)
As with CT, MRI is used for further anatomic definition and tissue characterization of suspected chest masses. MRI is particularly good at differentiating cystic from solid structures, especially compared to CT. , MRI may also be used when planning surgical procedures. Availability and the need for sedation are potential disadvantages of MRI.
Positron emission tomography (PET)
PET is not a first-line imaging modality for diagnosing mediastinal masses in pediatric patients. However, PET imaging, including PET-CT or PET-MRI, can be used in staging tumors and monitoring response to therapy. , Such imaging for children, though, is usually found at tertiary pediatric centers and generally is not widely available.
Imaging findings
The patient had two-view plain radiography of the chest performed. There is a large rounded opacity in the left mid to upper chest that has a well-defined border laterally and inferiorly. There is mass effect on the lower trachea (displacement to the right) and left mainstem bronchus (displaced inferiorly and medially) ( Fig. 4.1 ).


Case conclusion
The patient was admitted with consultation by Pediatric Oncology and Pediatric Surgery. A contrast-enhanced CT scan of the chest was obtained, demonstrating the mass, which appears centered in the posterior left mediastinum but extends to involve the middle and anterior mediastinum ( Fig. 4.2 ). CT-guided biopsy revealed that the mass was a neuroblastoma. The tumor was determined to be intermediate risk. A metaiodobenzyl guanidine (MIBG) scan, whereby MIBG is absorbed by neuroendocrine cells, making this scan useful in the evaluation of metastasis of neuroendocrine tumors, was negative for metastases. The patient was treated with chemotherapy and subsequent surgical resection of the residual mass.


The most common cause of the appearance of a large mediastinum in neonates and young children is the normal prominence of the thymus. The thymus is important for the development of the immune system during childhood, primarily T cells, which are responsible for regulating cellular immunity, and B cells, which are responsible for regulating humeral immunity. Visualization of the neonatal/childhood (age <5 years) thymus by plain radiography is a normal finding. A normal thymus appears on plain chest radiography as a prominent soft tissue opacity in the anterior mediastinum, sometimes filling the anterior upper chest in young infants. It may be difficult to distinguish from the cardiac silhouette. A feature of the normal thymus often present on plain radiography is the “thymic wave sign,” which is undulation of the lateral thymic contour caused by the ribs, since the thymus is soft in texture and abuts the anterior ribs and costal cartilage ( Fig. 4.3 ). , Another normal appearance of the thymus on an AP view is that it can extend asymmetrically to the right, over the lung, with a straight inferior margin, and a convex lateral border, producing the so-called “sail sign” ( Fig. 4.4 A–C). However, one should not confuse this finding with the “spinnaker-sail sign,” in which the thymic lobes are laterally and superiorly displaced due to pneumomediastinum ( Fig. 4.4 D). , Infants and children (under 5 years of age) have a thymus with convex margins. With increasing age, the thymus becomes smaller, with more concave and straight borders. The thymus becomes inapparent on plain radiography by the teenage years. While the thymus is normally visible on plain radiography in neonates, infants, and young children, this is not the case with adolescents, and a normal thymus should not cause mass effect. A prominent, normal thymus may be mistaken for a mediastinal mass, occasionally prompting further imaging, typically US, CT, or MRI. A normal thymus will appear on advanced imaging as a homogenous structure without calcification or compression of surrounding structures. , The presence of calcification or mass effect should prompt further investigation for pathology.