- •
The diagnosis of an intracardiac mass requires definition of location, extent, hemodynamic effect, and tissue characteristics. Cardiovascular magnetic resonance (CMR) is ideally suited to provide this information.
- •
CMR may provide sufficient tissue diagnosis of masses such as lipoma and thrombus. Additional features in other cases may help refine the differential diagnosis but may not obviate the need for tissue procurement, particularly for treatment planning for malignant masses requiring histopathologic characterization.
- •
Benign tumors tend to obey tissue boundaries, whereas malignant processes are more likely to cross tissue planes.
- •
Malignant tumors of the heart are greater than 20 times more likely to represent metastatic disease versus primary cardiac tumors.
- •
Certain normal cardiac structures may be mistaken for abnormal cardiac masses; in such instances, delineating the anatomy helps define the diagnosis.
- •
Hemodynamic effects of masses are best assessed with cine imaging or velocity-encoded acquisitions, such as in cases of masses that may intermittently impair valve function due to obstruction.
- •
Contrast enhancement with first-pass T1-weighted imaging and delayed post-gadolinium imaging may provide information on the vascularity and fibrotic components of a mass.
- •
Delayed post-gadolinium imaging with a sufficiently long inversion time (greater than 600 ms) greatly facilitates the recognition of intracardiac thrombus.
This chapter illustrates the utility of cardiovascular magnetic resonance (CMR) in the diagnosis and characterization of cardiac masses. Although all possible cardiac masses are not described, we have grouped the cases into (1) normal cardiac structures that may be mistaken for a cardiac mass ( Case 1 ); (2) benign primary cardiac masses ( Cases 2-4 ); (3) malignant primary cardiac masses ( Cases 5 – 6 ); (4) cardiac masses due to systemic malignant processes ( Cases 7-9 ); and (5) nontumor cardiac masses ( Case 10 ). Some pericardial processes may also be considered masses, such as pericardial cysts (see Chapter 10 ).
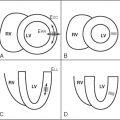
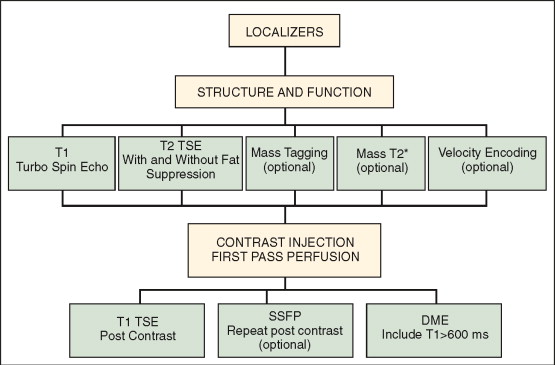
Multiple imaging modalities may be used to detect cardiac masses. CMR provides the most powerful non-invasive in vivo means of characterizing a mass based on its intrinsic tissue properties manifest as distinct signal intensities using different weightings. CMR’s multiplane acquisition affords evaluation of secondary hemodynamic effects of a mass, such as impaired mitral filling caused by a large left atrial mass. Figure 8-1 illustrates typical elements of a CMR cardiac mass protocol. The basic tasks in an imaging examination of cardiac masses are localization and characterization. Localization images help direct the examiner to relevant juxtacardiac abnormalities that may be related to the mass. Here one may find pleural and pericardial effusions, mediastinal extension of masses, or evidence of hepatic involvement. Morphologic questions include extent and infiltration of the mass, size, and involvement of cardiac structures. Utilizing T1- and T2-weighted turbo spin echo (TSE) sequences, with and without fat suppression, is central to tissue characterization. T2*-weighted sequences can be used in circumstances where hematoma or thrombus may be suspected. Evaluation of the hemodynamic effect of the mass requires dynamic imaging to define valvular involvement, compression or obstruction of vascular structures, and effect on cardiac function. Myocardial tagging can be employed to assist in defining motion of the mass versus normal myocardial deformation as well as to distinguish cardiac from juxtacardiac structures. After noncontrast acquisitions are completed, visualization of the transit of gadolinium-based contrast through the heart and mass with techniques such as perfusion imaging helps to define vascularity. Postcontrast imaging with various inversion times (TIs) allows for delineation of fibrotic components as well as ready delineation of thrombus when long (greater than 600 ms) TIs are used.
NORMAL CARDIAC STRUCTURES THAT MAY BE MISTAKEN FOR A CARDIAC MASS
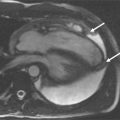
A 38-year-old woman with a history of hypertension, and tobacco and cocaine abuse presented to the emergency room with complaints of right foot pain. Clinical examination of the lower extremities demonstrated findings consistent with arterial embolization. Transesophageal echocardiography (TEE) was performed to evaluate for cardiac source of emboli. TEE suggested a mass in the right atrium. CMR was performed ( Figure 8-2 ).
Comments
CMR affords imaging of cardiac structures in limitless planes. Lack of true volumetric imaging capabilities and tissue characterization with other imaging modalities may cause certain cardiac structures to be described as abnormal cardiac masses. The term pseudomass denotes a normal cardiac structure that is mistaken for cardiac pathology. The Eustachian valve is present in the right atrium at the insertion of the inferior vena cava and is an embryologic remnant of the valve from the inferior vena cava that may be mistaken for a right atrial mass if prominent. Other cardiac structures that may be denoted pseudomasses include the crista terminalis, right ventricular trabeculation, and atrial septal aneurysm.
BENIGN PRIMARY CARDIAC MASSES
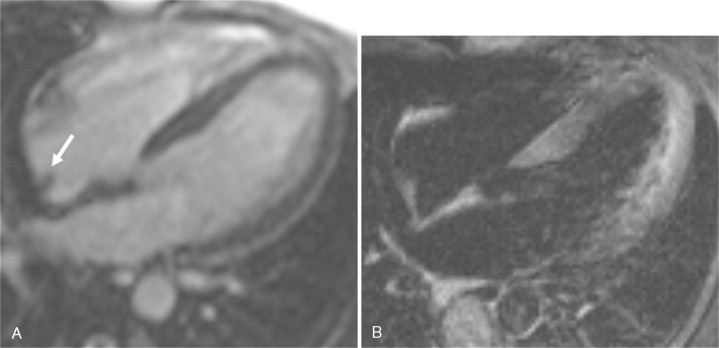
A 58-year-old man presented for cataract surgery and was found to have an abnormal electrocardiogram. Evaluation included a surface echocardiogram that was suggestive of a right atrial mass. CMR findings are shown in Figure 8-3 .
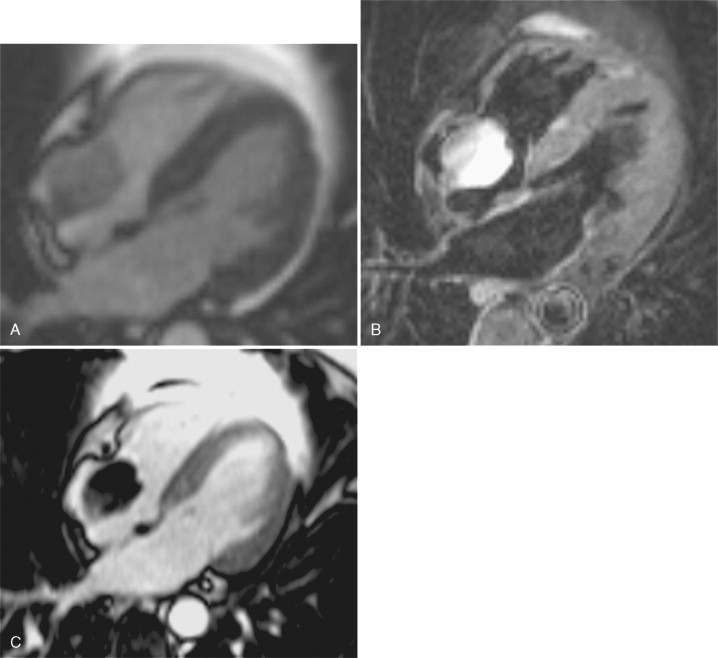
Comments
Cardiac myxomas comprise 30% to 50% of all benign cardiac tumors. They typically originate from the fossa ovalis; however, they may originate from the posterior atrial wall, anterior atrial wall, or atrial appendage. Seventy-five to eighty percent are seen on the left atrial side; rarely, a cardiac myxoma arises from ventricular myocardium. They are typically solitary tumors and often pedunculated with a smooth, rounded surface. Owing to their vascularity, myxomas typically perfuse with first-pass gadolinium contrast and enhance to variable extent on delayed enhancement imaging. Myxomas can be distinguished from benign tumors such as lipomas and fibromas using T2-weighted imaging; both lipoma and fibromas are typically dark on T2 weighted images compared with the T2 enhancement characteristic of myxoma.
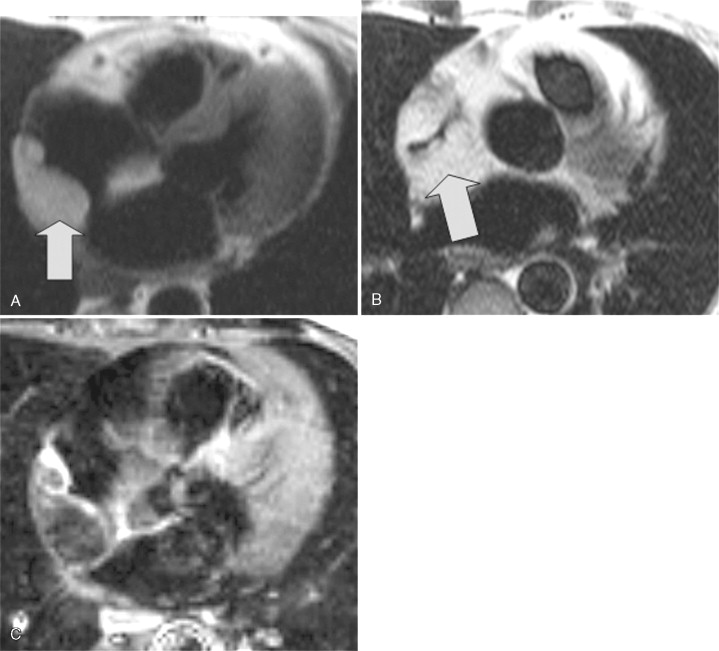
A 63-year-old woman had a history of breast cancer as well as poorly differentiated B cell malignancy. She presented with new-onset atrial flutter underwent transesophageal echocardiography prior to cardioversion. TEE demonstrated a right atrial mass obstructing the SVC. Given her medical history, the concern for malignant extension was significant prompting CMR examination to further characterize the mass ( Figure 8-4 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree