- •
Cardiovascular magnetic resonance (CMR) can be used to assess myocardial inflammation.
- •
A single CMR study provides comprehensive information on ventricular size, morphology, function, pericardial involvement, and inflammatory activity.
- •
Inflammatory activity of the myocardium can be assessed by:
- •
T2-weighted CMR (identifies global or regional edema)
- •
T1-weighted, gadolinium (Gd)-enhanced CMR shortly after contrast injection (hyperemia and capillary leakage caused by inflammatory activity)
- •
T1-weighted, Gd-enhanced CMR late after contrast injection (“late Gd enhancement” identifies inflammation-induced irreversible injury)
- •
- •
A combination of these sequences and derived criteria increases the diagnostic accuracy of CMR.
- •
CMR is useful for the follow-up of patients with complicated or ongoing myocarditis.
- •
CMR is useful for identifying patients suitable for endomyocardial biopsy.
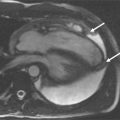
A 42-year-old man, previously healthy and active, presented with new-onset severe chest pain at rest, shortness of breath, and generalized weakness after a GI infection with severe diarrhea 2 weeks before. CMR was performed ( Figures 13-1 to 13-5 ).





Comments
Myocardial inflammation may be caused by a variety of diseases such as viral infection, toxic agents, or autoimmune processes. The incidence has been underrated because of a lack of specific clinical findings and more importantly sensitive tools to detect myocarditis in clinical settings. Although usually of benign prognosis, more severe cases of myocarditis come with a substantial mortality. Endomyocardial biopsy with immunohistology is considered by many the gold standard. Its utility as a first line diagnostic tool, however, is significantly hampered by its limited sensitivity and invasiveness.
Cardiovascular MR (CMR) is being increasingly used in various clinical scenarios of myocarditis. The contribution of CMR in suspected myocarditis includes:
- •
Regional and/or global ventricular dysfunction
- •
Inflammatory activity in the myocardium
- •
Inflammation-induced irreversible tissue damage
- •
Pericardial involvement
For quantitatively assessing function, steady-state free precession techniques provide a very robust image quality and also allow for looking at pericardial effusion. It should be emphasized that the accurate quantification of ventricular size and ejection fraction/stroke volume are of specific use in the follow-up of patients with myocarditis, who may have only minor functional abnormalities.
The versatile MR technology is (as in other organ systems) especially helpful to identify inflammatory tissue characteristics. Three different criteria are being used:
- •
Globally or regionally increased water content in T2-weighted images (inflammatory edema)
- •
Globally increased blood volume (inflammatory hyperemia) and increased early distribution of interstitial Gd compounds (capillary leakage) in T1-weighted images pre- and early post-contrast administration (early enhancement). This is calculated using the following formula:
<SPAN role=presentation tabIndex=0 id=MathJax-Element-1-Frame class=MathJax style="POSITION: relative" data-mathml='SImyo(postcontrast)-SImyo(precontrast)/SImyo(precontrast)SIskeletal(postcontrast)-SIskeletal(precontrast)/SIskeletal(precontrast)’>SImyo(postcontrast)−SImyo(precontrast)/SImyo(precontrast)SIskeletal(postcontrast)−SIskeletal(precontrast)/SIskeletal(precontrast)SImyo(postcontrast)-SImyo(precontrast)/SImyo(precontrast)SIskeletal(postcontrast)-SIskeletal(precontrast)/SIskeletal(precontrast)
SI myo ( postcontrast ) – SI myo ( precontrast ) / SI myo ( precontrast ) SI skeletal ( postcontrast ) – SI skeletal ( precontrast ) / SI skeletal ( precontrast )

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree