11 Needle Imaging
Needle tip visibility is critical to the success and safety of regional block interventions. It is imperative to identify the needle tip before advancing the needle. The cut on the bevel is the best identifier of the needle tip for a beveled needle. Partial lineups (so that the needle tip is not within the plane of imaging but some of the needle shaft is) are a source of false reassurance with in-plane technique. A number of factors have been reported to influence needle tip visualization under clinical imaging conditions (Table 11-1).
Table 11-1 Factors Reported to Influence Needle Tip Visibility
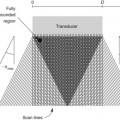
Insertion Angle (Angle of Insonation)
Needle tip imaging is optimal when the needle is parallel to the active face of the transducer. The cleanest needle echo is from a conventional needle at or near parallel. One study found a linear correlation between angle of incidence (measured from 0-75 degrees) and the mean needle tip brightness.1
Needle Gauge
There are multiple advantages to using a large needle for regional block. Needles as large as 17 gauge have been used to improve needle tip visibility for regional blocks.2 Alignment of a large needle is faster with in-plane technique. An additional advantage of a large needle is the ability to redirect the needle within the scan plane. A large needle tip can be used to displace structures (e.g., arteries or nerves) before advancing. The disadvantages of the large needle are patient discomfort and the consequences of unintended puncture (e.g., of vessels, nerves), which are typically worse. In addition, the soft tissue properties (tent and recoil) are more noticeable with large needles. With finer needle tips, the hand motion and needle tip motion are more closely matched, and it is easier to place a fine needle tip within a thin fascial plane.