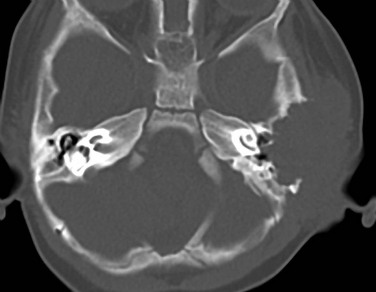
Chapter 12 Rhabdomyosarcoma (RMS) is the most common soft tissue sarcoma of childhood, accounting for approximately 60% of all soft tissue sarcomas and 5% to 8% of all childhood cancers.1 Approximately 40% of all RMSs occur in the head and neck region. Temporal bone RMS is relatively rare. In a study of 39 pediatric head and neck RMS cases, 6 patients (15%) had temporal bone involvement.2 Most patients present before age 12 years, and 40% are younger than 5 years at presentation. An equal gender incidence is observed. The embryonal form is the most common type to involve the middle ear.3 The onset may be insidious, with presentations of serosanguineous otorrhea or nonsuppurative granulation tissue simulating otitis externa or otitis media. The most common presentation of temporal bone RMS is chronic otitis media that is not responsive to therapy.2 Many patients present with swelling or facial nerve palsy.3 The role of computed tomography (CT) is to demonstrate bone erosion and a soft tissue mass. Magnetic resonance imaging (MRI) is indicated for evaluation of intracranial extension and involvement of vascular structures (internal carotid artery, jugular vein, and dural venous sinuses). MRI appearance is usually a nonspecific, enhancing, destructive mass (Fig. 12-1, A and 1B). Partial or total sparing of the otic capsule leaves the bony cochlea, vestibule, and semicircular canals isolated, creating an appearance referred to as skeletonization. Figure 12-1 Rhabdomyosarcoma in a 12-year-old girl with hearing loss. Treatment regimens combining chemotherapy and radiotherapy, with or without surgery, have improved the once-dismal outcomes of patients with temporal bone RMS. In a study of 14 patients, 82% of 5-year disease-free survival rate was reported.3 Langerhans cell histiocytosis (LCH) is a histiocytic proliferation of unknown etiology occurring primarily in infants and children. The diagnosis of LCH is made histologically by demonstration of the characteristic electron microscopic features of CD1a positivity in the involved tissue.4 In children younger than 15 years, the annual incidence of LCH is estimated to be 0.5 in 100,000.5 The mean age at presentation is 12 years, and no sex predilection is observed. The most common form of LCH is a solitary osteolytic lesion of the skull and spine.6 The temporal bone may be involved in isolation or as part of polyostotic or systemic disease.7 Temporal bone involvement may be unilateral or bilateral (30% of cases). Although ear and temporal bone involvement is relatively rare, otologic signs and symptoms may be the only manifestations of LCH, including ear infection, otorrhea, postauricular swelling, or aural polyp. The ossicles may be eroded. Conductive hearing loss is occasionally seen in temporal bone LCH.8 Sensorineural hearing loss and vertigo may result from destruction of the bony labyrinth. The lesion is characterized on CT as a nonspecific, lytic soft tissue mass. As in calvarial LCH, no periosteal reaction of the residual bone, which has sharp, well-defined margins, is seen (Fig. 12-2). The role of MRI is to demonstrate the soft tissue mass and the associated intracranial involvement and evaluate the hypothalamic-pituitary axis, which may be concomitantly involved in systemic LCH. Chemotherapy is generally the treatment of choice for temporal bone LCH.
Neoplasia
Rhabdomyosarcoma
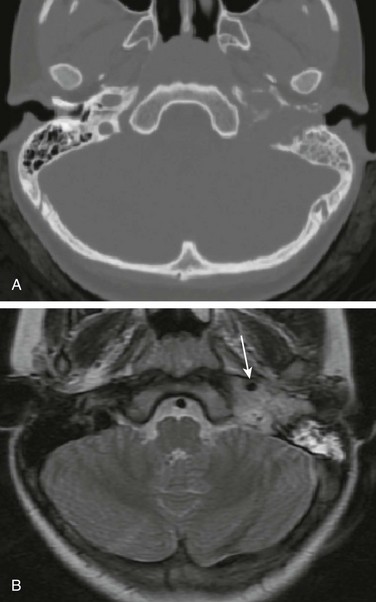
A, Axial noncontrast computed tomography image shows a destructive soft tissue mass involving the petrous and tympanic segments of the left temporal bone. The mastoid air cells are opacified. B, Axial T2-weighted magnetic resonance image displays that the mass is less hyperintense than the fluid in the mastoid air cells. The signal void of the petrous segment of the left internal carotid artery (arrow) is displaced anteriorly. (Courtesy Arzu Kovanlikaya, MD, New York.)
Langerhans Cell Histiocytosis
Neoplasia