Chapter 144 In the decades since the landmark articles by Caffey (1946) and Kempe and Silverman (1962), the medical community, law enforcement, and Child Protective Services (CPS) have developed a much greater awareness and sensitivity to the diagnosis of child abuse; these groups have not only advocated for protection of the child but have also promoted a more aggressive approach to the identification and prosecution of offending individuals.1,2 Child abuse remains a difficult, emotionally charged topic. The diagnosis of child abuse and the treatment of abused children are intertwined with legal issues of parental rights and family preservation. Because it typically occurs behind closed doors, the abuse is unobserved, and confessions are rare. Presentations are varied, and abuse and neglect may mimic other disease processes. Etiologies, Pathophysiology, and Clinical Presentation: According to the most recent survey from the U.S. Department of Health and Human Services, in the year 2009 an estimated total of 3,043,000 children were the subject of investigations undertaken by CPS agencies as alleged victims of maltreatment, and approximately 702,000 were found to be victims of maltreatment.3 Thus, in 2009, 40.2 of every 1000 children in the United States were evaluated by CPS for suspected abuse or neglect, and 9.3 of every 1000 children were confirmed by CPS as abused or neglected.3 Of confirmed cases, children were victims of neglect in 78.3%, physical abuse in 17.8%, sexual abuse in 9.5%, psychological maltreatment in 7.6%, and other forms of maltreatment in 9.6% (>100% as many children are victims of multiple forms).3 Young children are at greatest risk for fatality; 81% are younger than 4 years of age at the time of death, and 46% are younger than 1 year of age at death.3 An estimated 1770 children died from abuse or neglect in 2009.3 More than 90% of all confirmed perpetrators have a parental relationship to the victim (mother, father, step-parent, boyfriend or girlfriend of parent).3 Clinical presentations of child abuse are myriad. In some children, abuse is suspected from the start; however, in many, the presentation is cryptic until traumatic findings are made clinically or by imaging.4 Children commonly present with symptoms related to head, abdominal, or extremity trauma. Children may present with bruising, burns, or evidence of neglect. Not infrequently, manifestations of abuse may be found incidentally on imaging performed to evaluate a nontraumatic process. Therefore, the radiologist is occasionally the first to suggest the possibility of child abuse. Imaging: Initial imaging of the abused child is driven by the clinical presentation.5,6 Imaging is performed to evaluate for processes that need immediate management or may further threaten the child’s well-being if not diagnosed and treated. Once the child’s acute medical issues are addressed and their condition is stable, further imaging in the form of a radiographic skeletal survey can be performed to look for occult injuries and evaluate for child abuse as a diagnosis. The role of such imaging is threefold: 1. Recognition of physical abuse, supporting the diagnosis in suspected cases, and recognizing characteristic lesions when the possibility of child abuse has not been suspected. 2. Provision to the prosecution or defense of accused offenders of an understanding of the mechanism, patterns of healing (dating), and likelihood of such injuries with a reasonable degree of medical certainty. 3. Exclusion of the diagnosis of child abuse in cases of true accidental trauma or with variants of normal and disease processes that may mimic abuse. Computed tomography (CT) and magnetic resonance imaging (MRI) are used to evaluate suspected head trauma. There are no firm indications for CT of the chest in suspected physical abuse or infants with blunt traumatic injury. CT of the abdomen and pelvis is indicated only in children with physical examination, laboratory findings, or both suggesting traumatic intraabdominal injury.7–9 In all cases of suspected physical abuse in children younger than 2 years of age, a skeletal survey is mandatory (Box 144-1).5,6,10 A “babygram” consisting of single or few images of the entire infant is unsatisfactory. If radiographic film is used, high-detail film without a grid is recommended.10 Digital radiography has replaced film screen skeletal surveys in many centers; however, further evaluation of the technical elements necessary to produce high-detail images is still needed. Ideally, each skeletal survey is reviewed by a radiologist before the child leaves the radiography suite. Poorly positioned and otherwise suboptimal images should be repeated. Additional views may be obtained to further define positive or suspected abnormalities (e-Fig. 144-1). Commonly acquired additional views include lateral views of the extremities, coned views centered at the joints (wrist, ankle, knee), and Townes view of the skull. e-Figure 144-1 Images showing the value of additional views in a 2-month-old female infant. A follow-up skeletal survey performed 2 weeks after the initial examination may provide additional information (e-Fig. 144-2).11,12 As noted by Kleinman, the follow-up survey aids by (1) detecting additional fractures; (2) differentiating fractures from normal developmental variants; and, (3) assisting in dating injuries.11 Follow-up surveys may be limited or tailored to areas of interest.13 e-Figure 144-2 A 6-week-old male infant sent for an upper gastrointestinal series for evaluation of colicky pain was found to have healing rib fractures. In infants and children younger than 2 years, nuclear scintigraphy should be viewed as a complementary modality to radiographic evaluation.14–16 In general, nuclear medicine bone scans are used for problem solving and in children with a high suspicion for abuse but with negative or equivocal radiography. Whole-body MRI and positron emission tomography have both been studied for the detection of abuse injuries.17,18 Both modalities lack sensitivity for metaphyseal lesions but do detect many abuse-related lesions. Radiographic skeletal surveys should be performed in all cases of fatal suspected abuse and unexplained infant death.19–22 Postmortem surveys follow the same imaging protocol as used in living infants.20 At present, little experience with postmortem whole body CT exists; however, this technique does show promise for detecting subtle findings to guide the forensic pathologist.23 Imaging Findings: No one radiographic finding is pathognomonic of child abuse. Individual radiographic findings vary from high specificity to low specificity.24,25 High-specificity lesions are seen with abusive trauma but are rarely seen in other forms of trauma. Low-specificity lesions may be commonly seen with abuse-related trauma but are also common with trauma not associated with trauma. Paul Kleinman has written extensively on the radiography of child abuse and has classified the findings into categories of high, moderate, and low specificities (Box 144-2).24,25 This categorization is supported by many series in the literature, although a number of reports support slight modifications to the categorization of findings. Rib fractures are found in approximately 50% of fatally abused infants.26 The ribs may be the only site of skeletal trauma in some abused children.27 In a surviving infant, the astute clinician may palpate callus with healing or, rarely, crepitus, but otherwise, typically, no physical sign of injury is present. Most acute rib fractures are subtle buckle or greenstick type fractures not evident and frequently are not appreciated on radiography until evidence of healing is found (see e-Fig. 144-2).28 Fracture may occur at any point along the arc of the rib (costovertebral, posterior, lateral, anterior, or costochondral) but frequently involve the posterior rib.26,29 Posterior rib fractures at the costovertebral junction have a high specificity for abuse.30–32 Boal and associates reviewed 1463 rib fractures in 141 abused infants and noted that when individual sites along the rib arc were compared, costovertebral junction fractures outnumbered all other individual sites.30 However, fractures at the costovertebral junction represented only 33% of the total number of rib fractures. Fractures at other sites in the rib arc are very common in abused children, too.30 Fractures at the costochondral junction appear radiographically similar to classic metaphyseal lesions of the long bones and have a high association with visceral trauma.33 First rib fractures bear high specificity for child abuse.34 A squeezing injury, shaking injury, or a combination of both results in leveraging of the posteromedial rib over the spinal transverse process. Excessive compression and distraction forces are also placed on the lateral and anterior rib arc and at the metaphyseal equivalent region near the costovertebral junction of the rib (Fig. 144-3).28,35 Multiple fractures may involve a single rib. Oblique views of the ribs increase the sensitivity for rib fractures and aid in their characterization (Fig. 144-4).36 Nuclear scintigraphy aids in the detection of rib fracture and plays a complementary role to that of radiography (e-Fig. 144-5).14,15 Follow-up radiographs (see e-Fig. 144-2) and CT also provide increased sensitivity.37,38 CT may be more sensitive for rib fractures than radiography, but the greater radiation dose of CT limits its use as a screening modality.37 Nevertheless, focused CT may be helpful in problematic cases. If a CT is performed for evaluation of visceral trauma, reconstruction of images with narrow slice thickness, bone detail algorithm, and multiplanar reformats facilitate identification and delineation of rib fractures (Fig. 144-6). Figure 144-3 Mechanism of rib injury. Figure 144-4 A 2-month-old male infant with right pleural effusion. Figure 144-6 A 3-month-old male with multiple rib fractures, multiple metaphyseal fractures (classic metaphyseal lesions), a small subdural hematoma, and disruption of the posterior wall of the hypopharynx. e-Figure 144-5 A 5-week-old male with multiple rib fractures, subdural hematomas, and skull fracture. In contrast to adult ribs, fractures rarely occur in infant ribs because of cardiopulmonary resuscitation.39–42 Rare fractures caused by infant cardiopulmonary resuscitation are predominantly anterolateral and are usually radiographically occult.39,40,43 Rib fractures caused by birth trauma are rare.44 A case report noted posteromedial rib fractures from accidental blunt trauma in an infant.45 Rib fractures are commonly seen in infants with metabolic bone disease and have been reported after thoracotomy, chest tube placement, and chest physiotherapy.34,46 However, rib fractures in infants younger than age 12 months without a predisposing condition, for example, instrumentation, prematurity, chronic illness, metabolic bone disease, or all of these, are strongly suspicious for the diagnosis of abuse.34,47 The classic metaphyseal fracture, first described by Caffey and commonly referred to as a “corner” or “bucket-handle” fracture, was reexamined by Kleinman in 1986 with the use of detailed histopathologic and radiographic studies.1,48 He determined that the lesions represent a complete shearing or planar fracture that extends through the primary spongiosa of the metaphysis and that it is not an avulsion injury as described by Caffey.48,49 Depending on size and displacement of the metaphyseal fragment, the positioning of the child and the radiographic projection, this highly specific lesion caused by abuse may appear as a “corner” fracture or as a “bucket-handle” fracture (Fig. 144-7). Metaphyseal fractures of abuse may also be seen on ultrasonography.50 Figure 144-7 Corner and bucket-handle fracture patterns of the classic metaphyseal lesion. The “classic metaphyseal lesion,” a term coined by Kleinman, occurs from violent shaking as the infant is held by the trunk or extremities (Figs. 144-8 and 144-9; e-Fig. 144-10; and Fig. 144-11). Some lesions are probably also caused by torsional pulling on a limb. Typically, no bruising or outward sign of injury is evident with a classic metaphyseal lesion. Classic metaphyseal lesions are most commonly seen at the proximal humerus, distal radius, distal femur, proximal tibia, and distal tibia and fibula.51–54 Figure 144-8 A 2½-month-old male infant with acute and chronic subdural hematoma and 18 fractures. Figure 144-9 A 1-month-old female infant was brought to the emergency department for swelling of the leg without history of trauma. e-Figure 144-10 Anteroposterior right (A) and left (B) shoulders of a 5-month-old female infant, deceased, cause of death unknown. Occasionally, classic metaphyseal lesions become more conspicuous on short-term follow-up radiography.49 With healing, classic metaphyseal lesions typically become indistinct and sclerotic. Kleinman demonstrated subtle extension of physeal cartilage into the metaphysis as a sign of healing.55 Subperiosteal new bone is not seen unless there is an associated periosteal injury. Transverse, greenstick, and buckle fractures of the metaphysis may also be caused by child abuse but do not carry the same specificity as the classic metaphyseal lesions. Such fractures are considered to be of low specificity. Small stepoffs, beaks, and spurs at the metaphyseal margins may mimic abusive injury.56 Slight fragmentation of metaphyseal margins with physiologic bowing may also mimic abuse.57 Iatrogenic classic metaphyseal-like lesions have been reported with birth trauma and as a complication of treatment of clubfeet.50,58,59 Such reports are rare and it is likely that the reported fractures occurred with a similar torsional mechanism as occurs in child abuse.
Child Abuse
Overview

A, Frontal view of the right wrist shows subtle sclerosis and irregularity of the radial metaphysis. B, Lateral view confirms healing classic metaphyseal lesion.
A, Initial chest radiograph identified healing fractures at the right 9th, 10th, and 11th ribs. B, Follow-up chest radiograph 2 weeks later showed additional fractures, now healing, at the lateral aspect of the left third through ninth ribs. The father admitted to shaking the infant.
Rib Fractures
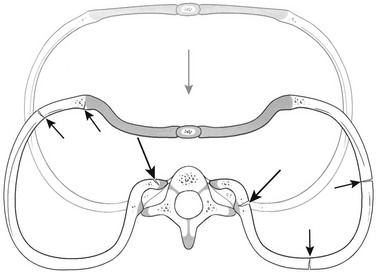
With anteroposterior compression (gray arrow) of the chest, excessive leverage of the posterior ribs occurs over the fulcrum of the transverse processes. This places tension along the inner aspects of the rib head and neck regions, resulting in fractures at these sites (long black arrows). This mechanism is consistent with morphologic patterns of injury occurring at other sites along the rib arcs and at the costochondral junctions (short black arrows). (From Kleinman PK. Diagnostic imaging of child abuse. 2nd ed, St Louis, MO: Mosby; 1998.)
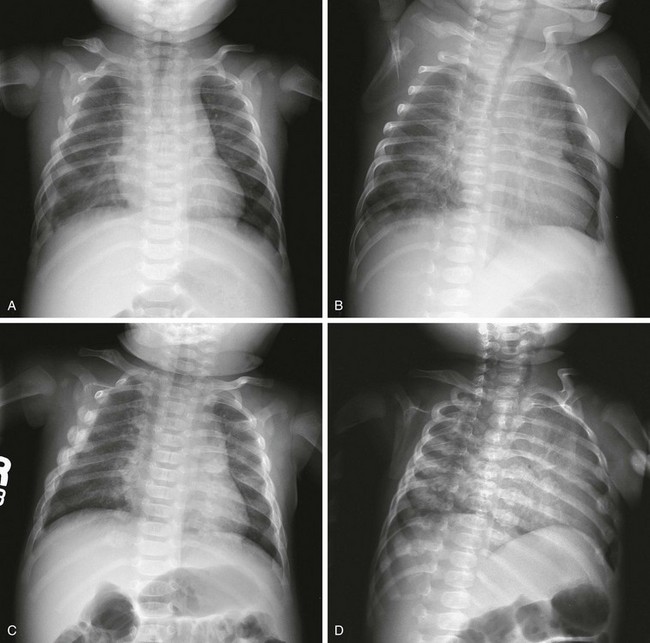
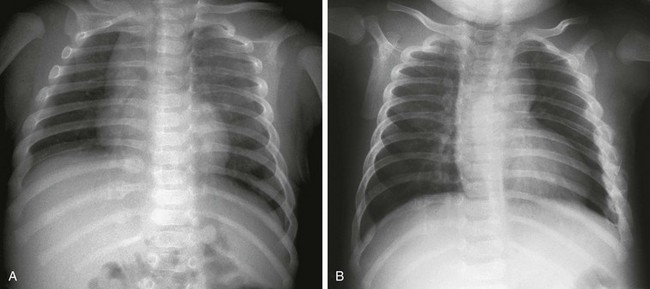
A, Anteroposterior radiograph shows healing right clavicular fracture and nine fractures of the right ribs and four fractures of the left ribs on initial survey. B, Some fractures are better depicted on the left posterior oblique view. C and D, Two weeks later, anteroposterior and left posterior oblique radiographs of the chest clearly show 18 right rib fractures and 11 left rib fractures, illustrating the value of a follow-up skeletal survey.

This computed tomography scanning was performed for concern of extension of infection into the chest. Images were also reconstructed with bone algorithm. Arrows indicate healing posterior and anterolateral rib fractures. The fracture lines are indistinct. Callus is present.

Posterior image from bone scintigraphy performed the same day shows multiple bilateral posterior and left lateral rib fractures. The posterior rib fractures are seen as abnormal foci of activity in a line on each side of the spine.
Long Bone Fractures
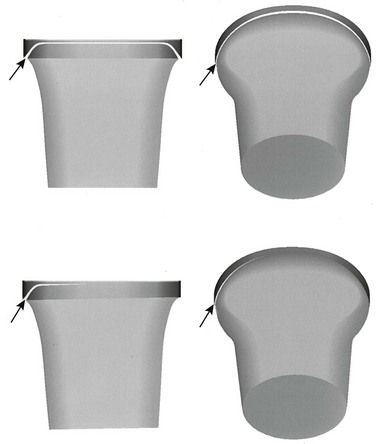
Fractures (arrows) extend adjacent to the chondro-osseous junction and then veer toward the diaphysis to undercut the larger peripheral segment that encompasses the subperiosteal bone collar. When the physis is viewed tangentially, the classic metaphyseal lesion appears as a corner fracture (left images). When a view is obtained through beam angulation, a bucket-handle pattern results (right images). Top images, Diffuse injury; bottom images, localized injury. (From Kleinman PK. Diagnostic imaging of child abuse. 2nd ed. St Louis: Mosby; 1998. Originally modified from Kleinman PK, Marks SC, Jr. Relationship of the subperiosteal bone collar to metaphyseal lesions in abused infants. J Bone Joint Surg Am. 1995;77:1471-1476.)

Anteroposterior radiograph of the right knee shows classic metaphyseal lesions at the distal femur and the proximal tibia.

A, Anteroposterior view of the left leg. B, Lateral view of the left leg shows classic metaphyseal lesions at the proximal and distal tibia, as well as a short oblique mid-diaphyseal fracture. Multiple rib fractures and classic metaphyseal lesions of the right tibia were also discovered.
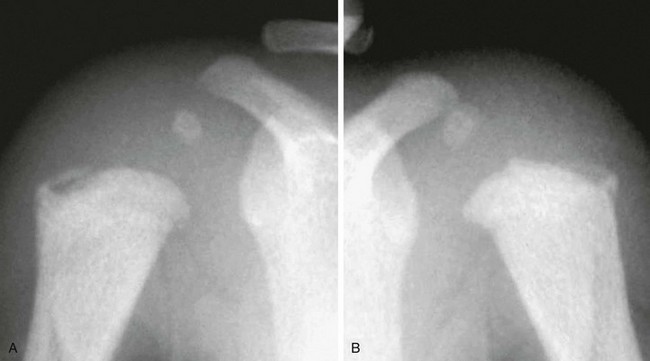
Eight fractures were identified at postmortem skeletal survey, including bilateral proximal humeral classic metaphyseal lesions.
Child Abuse









