Fig. 7.1
Seminoma. Transverse gray-scale sonogram of the testis (arrows) shows an enlarged heterogeneous hypoechoic testis consistent with a large tumor, replacing the entire testis, pathologically confirmed as seminoma
The vast majority (85 %) of pure seminomas are hypoechoic and 70 % of cases have a homogeneous texture without dense echogenic foci. Ten percent of seminomas present with varying degrees of cystic change, which some investigators attribute to infiltration and obstruction of the tubuli recti by tumor.
Most seminomas are confined within the tunica albuginea. Tumor extension through the tunica albuginea, involvement of paratesticular structures, and/or gross invasion of the spermatic cord should prompt consideration of another tumor type, particularly lymphoma. Retroperitoneal lymphatic spread and hematogenous spread to the lung, brain, or both are present in approximately 25 % of cases at the time of presentation.
Color flow or power Doppler ultrasound can be used for demonstration of vascularity of tumors. A color flow Doppler study showed increased vascularity in 95 % of primary testicular tumors larger than 1.6 cm in diameter and hypovascularity in 86 % of those smaller than 1.6 cm in diameter.
3-D power Doppler ultrasound is an alternative excellent technique for display vascularity of the lesions (Fig. 7.2).
Fig. 7.2
Seminoma. (a) Longitudinal color flow Doppler ultrasound shows a heterogeneous hypoechoic solid mass with prominent vascularization, pathologically confirmed as seminoma. (b) 3-D power Doppler ultrasound reveals vascularization of the tumor (arrows) (c) Another reformat image of 3-D power Doppler clearly shows prominent vascularity of the tumor
There is no correlation between vascularity and type or histologic stage of tumors.
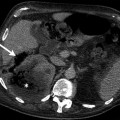
Computed Tomography
CT is a preferred imaging technique for staging of testicular cancer (Fig. 7.3).
Fig. 7.3
(a) Contrast-enhanced axial CT image of the abdomen of patients with embryonal carcinoma shows left para-aortic hypodense lymphadenopathy (arrow). (b) Axial CT of abdomen from a different patient reveals small-sized lymph nodes in left para-aortic region and anterior of the psoas muscle (arrow). (c) Contrast-enhanced coronal CT image of the abdomen shows same left para-aortic lymphadenopathy (arrow) with excellent anatomic display
Magnetic Resonance Imaging
Fibrous septa within tumor and enhancement of these septa higher than tumoral tissue are suggestive of seminoma.
Seminomas usually appear as homogeneous, low-signal-intensity nodular lesions on T2-weighed images (Fig. 7.4).
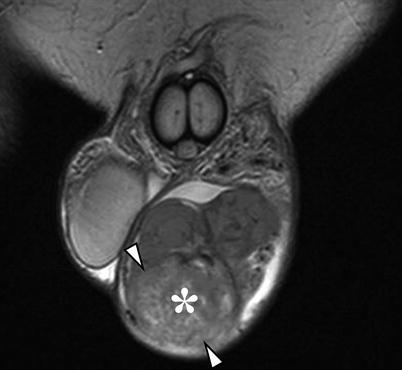
Fig. 7.4
Seminoma. Coronal T2-weighted image of a surgically confirmed seminoma of the left testis (*) in a 50-year-old patient. Seminoma has heterogenous signal intensity. There is interruption of the tunica albuginea by tumor suggestive of invasion and involvement of the epididymis (arrowheads) which confirmed on histopathology
Pathology
Seminoma averages 5 cm in diameter and is usually well circumscribed, multinodular and bulging, cream, pink, or tan, with focal hemorrhage (Fig. 7.5).
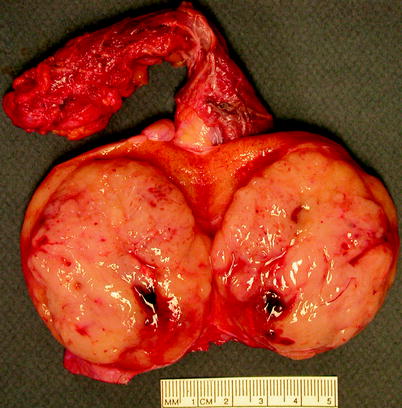
Fig. 7.5
Seminoma. A well-circumscribed bulging light tan tumor is shown, sharply demarcated from adjacent normal testicular tissue and with minimal hemorrhage and necrosis (Image courtesy of Christine Lemyre)
Necrosis, fibrous septa, extensive fibrosis, or invasion of adjacent soft tissues are seen in some. Histologically, it usually consists of sheets and nests of cells separated by thin fibrovascular septa but sometimes arrayed in linear cords or ribbons. The fibrovascular septa are characteristically infiltrated by variable numbers of lymphocytes, and granulomatous inflammation is often present in seminomas.
About half of cases show areas of necrosis, and vascular invasion is sometimes evident. Tumor cells are round to polygonal, with distinct cell membranes, clear or light pink cytoplasm, and large central nuclei with finely granular chromatin and one or more conspicuous nucleoli (Fig. 7.6). Mitotic figures are readily observed, and syncytiotrophoblasts may be present, singly or in small clusters (Fig. 7.7).
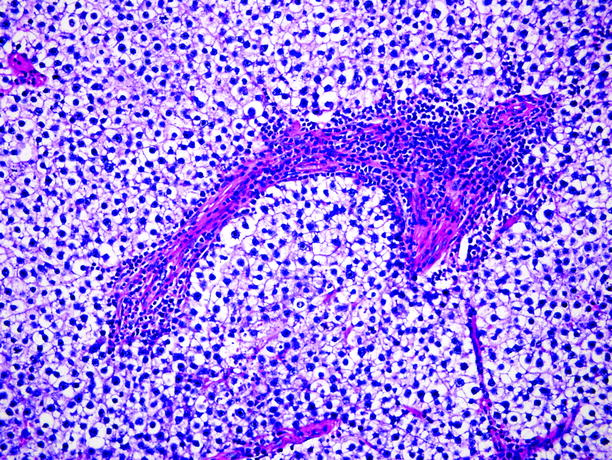
Fig. 7.6
Seminoma. Tumor cells with abundant clear to lightly eosinophilic cytoplasm, growing in sheets intersected by fibrous septa infiltrated by lymphoid cells
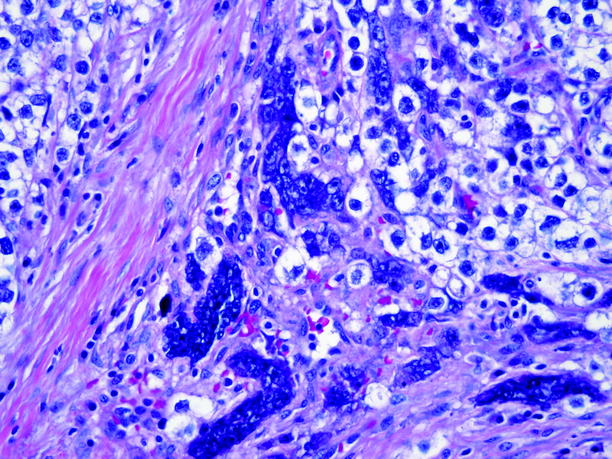
Fig. 7.7
Seminoma. Randomly scattered syncytiotrophoblasts are found in 4–7 % of seminomas. Although they may be accompanied by a small amount of blood, the extensive bleeding and necrosis typically seen in choriocarcinoma are absent, and the tumor cells mingled with the syncytiotrophoblasts are seminoma cells, not cytotrophoblasts, as would be the case in choriocarcinoma
Spermatocytic seminoma is typically well circumscribed, multinodular, gray to tan, soft, and friable, sometimes with a mucinous cut surface (Fig. 7.8). Cysts are sometimes present, but necrosis and hemorrhage are absent or minimal.
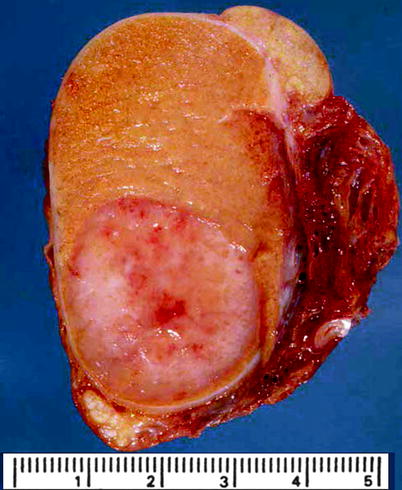
Fig. 7.8
Spermatocytic seminoma. Tumor is well circumscribed, sharply demarcated from adjacent normal testicular tissue, with a friable cut surface and minimal hemorrhage and necrosis (From MacLennan et al. (2003), with permission)
The cells of spermatocytic seminoma are arranged in large sheets in an edematous background, sometimes intersected by broad fibrous bands. Tumors consist of three cell types: small, medium, and large, the small cells resembling mature lymphocytes and the medium cells measuring 15–20 um in diameter (Fig. 7.9). The medium cells are the most numerous cell types and have pale nuclei and finely granular cytoplasm. The large cells can be up to 100 μm in diameter and sometimes contain more than one nucleus. The nuclei of some medium and large cells sometimes exhibit filamentous nuclear chromatin, similar in appearance to that of primary spermatocytes in meiotic prophase. The membranes of all cell types are indistinct, and abundant mitotic figures are usually present. No lymphocytic infiltrates or granulomatous changes are seen.
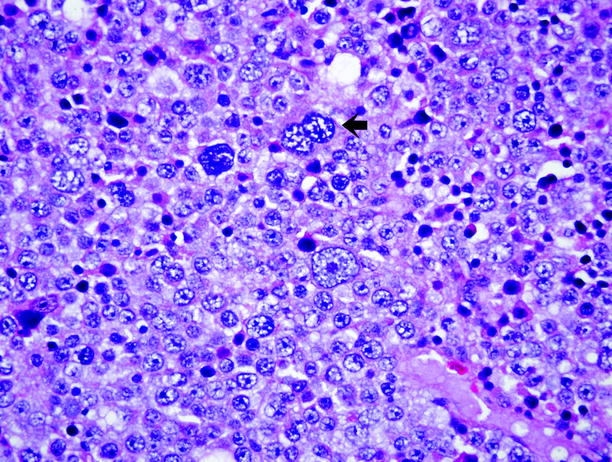
Fig. 7.9
Spermatocytic seminoma. This image shows the three tumor cell types: small, medium-sized (intermediate), and giant cells. Arrow indicates a giant cell with filamentous chromatin
Fewer than 1 % of cases metastasize. There are rare reports of sarcoma arising in spermatocytic seminomas, often with a fatal outcome.
Embryonal Carcinoma
General Information
Embryonal carcinoma is so named because its cells resemble early embryonic epithelial cells. It occurs in a younger population than seminoma and usually affects males aged 25–35 years.
Embryonal carcinoma is a component in 87 % of mixed germ cell tumors. In pure form, it accounts for only 2–3 % of all germ cell tumors.
Presenting symptoms include testicular enlargement with or without pain, gynecomastia, or symptoms attributable to metastases. Pure embryonal carcinoma does not cause elevation of serum AFP. Serum β-HCG level is elevated in 60 % of patients with this tumor.
The treatment and outcomes in embryonal carcinoma depend on clinical stage. About 70 % of stage I patients are cured by orchiectomy alone. Of patients who have or develop non-bulky stage II disease, 95 % are cured by various combinations of retroperitoneal lymphadenectomy and/or chemotherapy, and those with bulky stage II disease have a cure rate of 70–80 %.
Embryonal carcinoma is more aggressive than seminoma. Invasion of the tunica albuginea and extension into the epididymis can occur in about 20 % of cases and result in contour abnormality of the testis.
Imaging
Ultrasound
Embryonal carcinoma often exhibits heterogeneous echotexture (71 %), irregular or ill-defined margins (45 %), and cystic components (61 %). Echogenic foci represent areas of hemorrhage, calcification, or fibrosis.
If a true cyst with an epithelial lining is identified, this finding is suggestive of teratoma or a mixed germ cell tumor with a component of teratoma.
Magnetic Resonance Imaging
On MRI, nonseminomatous tumors are usually heterogeneous both on unenhanced and contrast-enhanced T1-weighted images and on T2-weighted images; enhancement patterns are more heterogeneous than seminomas.
Areas of hemorrhage and areas of necrosis can be detected in the majority of tumors.
Low-signal-intensity halo surrounding tumor represents a fibrous capsule and is typically associated with nonseminomatous tumors.
Tumor heterogeneity and heterogeneous enhancement are the most valuable findings for characterization of nonseminomatous lesion.
Hemorrhage within the tumor can be seen as areas of high signal intensity on T1-weighted images.
Pathology
Embryonal carcinoma is characteristically pink-tan to gray-white, bulging, friable, hemorrhagic, and extensively necrotic, with an average size of 2.5 cm (Fig. 7.10). It tends to be poorly circumscribed, and 25 % invade extratesticular soft tissues.

Fig. 7.10
Embryonal carcinoma. Tumor is sharply demarcated and extensively necrotic
Histologically, tumor cells form solid sheets, tubules, and papillae. Tumor cells are large, round or polygonal, with modest amounts of clear, pink, or basophilic cytoplasm. Cell nuclei are large, vesicular and irregular, with coarsely clumped chromatin and one or more prominent nucleoli (Fig. 7.11).
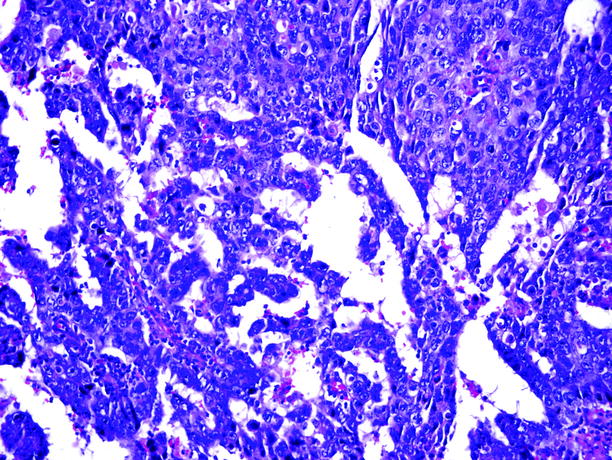
Fig. 7.11
Embryonal carcinoma. Tumor cells are arranged in poorly formed glands and papillary structures. They are overlapping and dark, with limited cytoplasm and indistinct cell membranes
Cell membranes are indistinct, and nuclei are crowded and overlapping. Mitotic figures are abundant, and apoptotic bodies are usually present. Necrosis and vascular invasion are commonly observed.
Syncytiotrophoblasts, singly or in small clusters, are often present in embryonal carcinoma, accounting for the high frequency of serum β-HCG elevation in these patients (60 %).
Yolk Sac Tumor (Endodermal Sinus Tumor)
General Information
This germ cell neoplasm derives its names from its resemblance to developing extraembryonic mesenchyme in humans; its glomeruloid structures resemble the endodermal sinuses of the rat placenta.
It occurs in postpubertal males and also in children under the age of 9 years, with a median age of 18 months. Although registry data indicate that it is more common than teratoma in the pediatric age group, combined series of pediatric testicular germ cell tumors from large centers indicate that teratomas far outnumber yolk sac tumor in children. Adults with yolk sac tumor have an average age between 25 and 30 years. Yolk sac tumor is pure in children, but in postpubertal males, it is virtually always a component of a mixed germ cell tumor rather than a pure neoplasm.
Patients usually note painless testicular enlargement, and serum AFP is usually elevated.
More than 90 % of children with yolk sac tumor survive 5 years. Metastatic yolk sac tumor in adults responds less favorably to chemotherapy than other forms of non-teratomatous germ cell tumors and hence has a worse prognosis.
Imaging
Ultrasound
The ultrasound appearances of yolk sac tumor are nonspecific; they are inhomogeneous and may contain echogenic foci secondary to hemorrhage or hypoechoic areas due to necrosis. Microcystic appearance may also be seen.
Magnetic Resonance Imaging
Isointense to hypointense to normal testicular tissue on T1-weighted images and hypointense on T2-weighted images—these findings are nonspecific.
Pathology
Pediatric yolk sac tumor is usually circumscribed, with a mucoid homogeneous, solid tan or gray-white cut surface, and little or no hemorrhage or necrosis (Fig. 7.12). Yolk sac tumor in adults is usually a component of a mixed germ cell tumor; those that have substantial elements of yolk sac tumor tend to be poorly circumscribed, soft to firm, and gray-white to tan, with considerable necrosis, hemorrhage, and cystic degeneration.
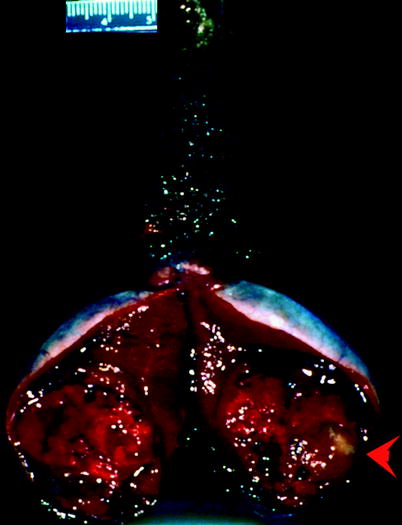
Fig. 7.12
Yolk sac tumor. Tumor is extensively hemorrhagic; a portion of the tumor has a glistening, gray, mucoid cut surface (arrow) (From MacLennan et al. (2003), with permission)
Microscopically, yolk sac tumor exhibits a number of architectural and cytologic patterns. Most common is the reticular pattern, consisting of a meshwork network of variably sized empty spaces representing cytoplasmic vacuoles and microcysts (Fig. 7.13). The endodermal sinus pattern is characterized by papillary fibrovascular structures lined by cuboidal or columnar cells, situated within circumscribed cystic spaces; these structures are called “Schiller–Duval bodies” and are distinctive for yolk sac tumor (Fig. 7.14).
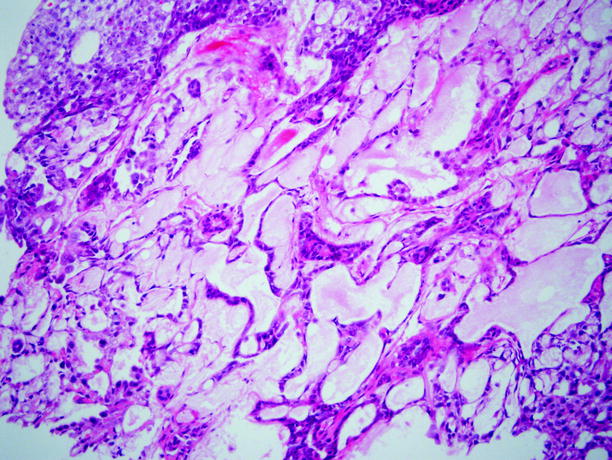
Fig. 7.13
Yolk sac tumor. This is an example of the microcystic or reticular pattern, one of the commonest of the many architectural variations seen in yolk sac tumor
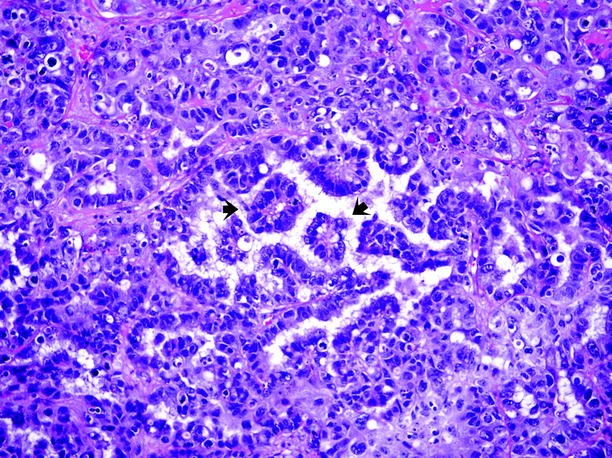
Fig. 7.14
Yolk sac tumor. This image shows several “Schiller–Duval” bodies, indicated by arrows, comprised of fibrovascular cores lined by neoplastic cells, lying within a circumscribed cystic space
Larger “macrocysts” are noted in some tumors. Tumor cells may be arranged to form sheets, glandular structures, or anastomosing villoglandular structures. Pink hyaline globules and eosinophilic deposits of extracellular basement membrane material are frequently noted in yolk sac tumors (Fig. 7.15).
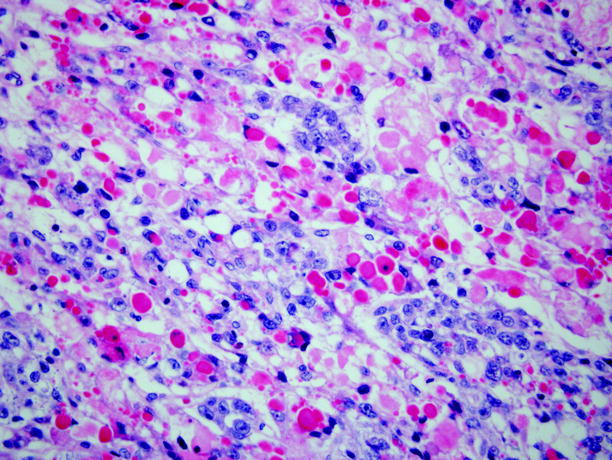
Fig. 7.15
Yolk sac tumor. Hyaline globules of variable size, staining light pink to dark red, are a characteristic finding of yolk sac tumors but may also be seen in other types of germ cell tumor. They sometimes show positive staining for α-fetoprotein
Teratoma
General Information
Teratoma is the other common testicular germ cell neoplasm in children, occurring usually in children less than 4 years of age, with a median age of 13 months.
In children, it occurs in pure form, but in adults, pure teratoma is rare, accounting for only 2–3 % of testicular neoplasms. However, teratomatous components are present in more than 50 % of all adult mixed germ cell tumors; consequently, serum AFP level is elevated in 38 % of adult patients with testicular teratoma, and β-HCG level is elevated in 25 % of adult patients with testicular teratoma.
Metastases can be observed in one-third of patients with adult teratoma at the initial presentation. With a single possible exception, teratoma in children has not been reported to metastasize and is considered benign. In postpubertal patients, testicular teratoma is considered malignant and can be associated with metastases that may be teratomatous, but the metastases may also consist of other types of germ cell neoplasm, such as embryonal carcinoma, reflecting the totipotential nature of the original malignant germ cell in the testis that produced a teratoma locally, but metastasized as an embryonal carcinoma.
Rarely, teratomas harbor nongerminal malignancies, such as rhabdomyosarcoma, squamous cell carcinoma, primitive neuroectodermal tumor (PNET), enteric-type adenocarcinoma, and angiosarcoma.
Metastases from secondary malignancies tend to be resistant to chemotherapy directed at the primary germ cell neoplasm.
Carcinoid tumor of the testis is extremely rare and is considered a monodermal form of teratoma. About 15–25 % of testicular carcinoid tumors are admixed with other elements of teratoma.
Imaging
Ultrasound
At gray-scale ultrasound, teratomas tend to be well-defined complex masses with cystic change.
Echogenic foci, with or without shadow, represent calcification, cartilage, immature bone, and fibrosis (Fig. 7.16).
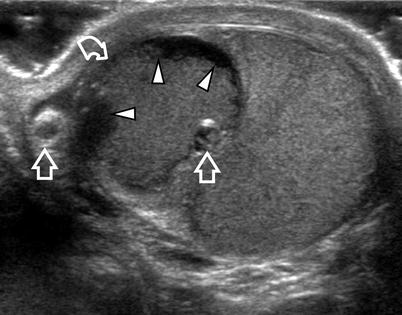
Fig. 7.16
Surgically proved mature teratoma in a 30-year-old patient. Transverse oblique US scan showing a markedly heterogeneous mass (curved arrow) with cystic areas, fluid–debris levels (arrowheads), and echogenic foci (arrows)
A diffuse parenchymal texture change with broad bands of dense echogenic foci associated with an acoustic shadow may be seen with teratomas.
Magnetic Resonance Imaging
On MRI, teratomas can contain low-signal-intensity areas, most likely due to calcification within the tumor, on both T1-weighted and T2-weighted images.
Pathology
Pure teratoma varies considerably in size and is typically solid and cystic, sometimes with areas of hemorrhage or necrosis and without apparent infiltration of paratesticular structures (Fig. 7.17).
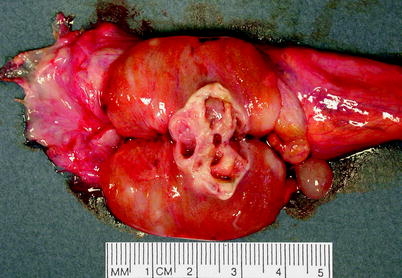
Fig. 7.17
Teratoma. Tumor is sharply demarcated and with characteristic solid and cystic components. This example was a pure teratoma in a postpubertal male
The cystic spaces contain mucoid fluid, serous fluid, or keratinous debris. Cartilage or fibrous tissue may be found in solid areas.
Microscopically, teratoma is composed of somatic-type elements resembling postnatal tissues derived from ectoderm (such as squamous or neuronal tissue), endoderm (such as respiratory or gastrointestinal-type glands), and/or mesoderm (such as cartilage, muscle, or fat) (Fig. 7.18).
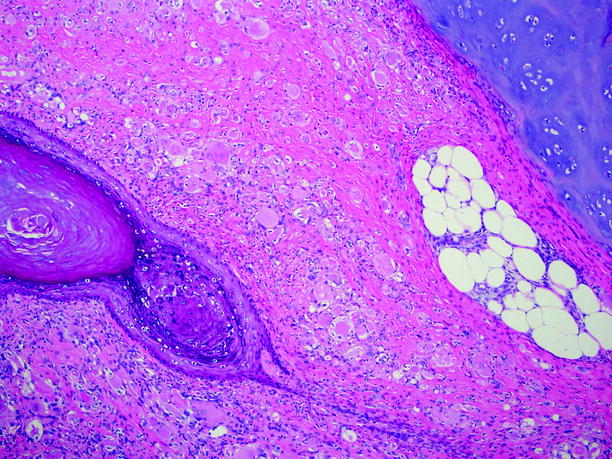
Fig. 7.18
Teratoma. At left is an aggregate of keratinizing squamous epithelial cells. Cartilage and fat are evident at upper right
The presence of immature elements, such as immature neuroepithelium, embryonic tubules, blastema, or immature soft tissues, is often noted, but such findings are of no known prognostic significance.
Choriocarcinoma
General Information
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree