55 Neuraxial Block
Introduction
In many patients, epidural and spinal blocks are routine procedures guided by loss of resistance and confirmation of free flow of cerebrospinal fluid, respectively. However, in patients with obesity or advanced age, these neuraxial blocks can be more challenging and may benefit from imaging guidance. Ultrasound imaging has been reported useful for guiding neuraxial anesthetics in patients with prior surgical instrumentation or scoliosis. Ultrasound can estimate the location and level of spinous interspaces. There also is evidence that ultrasound guidance improves the learning curve and reduces epidural failure rates of resident in training.1,2 However, there remain current limitations to the use of ultrasound technology to guide neuraxial blocks.
Selection of the correct interspace is important to the success of subarachnoid block. The interspace selected for injection of spinal anesthetic drugs affects the resultant distribution. The failure rate at lower lumbar interspaces can be as high as 7%.3,4 These failures probably relate to the site of the injection with respect to the peak of the lumbosacral curve. One of the potential benefits of ultrasound is to help establish the correct interspace for neuraxial block.
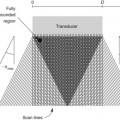
Longitudinal paramedian imaging planes provide the best visualization of neuraxial structures.5 With these views, the width of the acoustic window (the intervertebral space) is largest relative to the shadowing of the corresponding vertebral bone. Several authors have described the epidural space and adjacent bone to have a sawtooth configuration in this parasagittal view.6 The “saw sign” of longitudinal paramedian views inclines toward the skin surface in the caudal direction.
Midline transverse imaging planes are often used for offline markings for midline approaches for lumbar epidurals and spinals. This transverse view has been described as having a “flying bat” appearance.7 In this view the articular processes (the rounded mamillary processes) of the facet joints form the ears of the bat and indicate the widest part of the interlaminar space. Although transverse imaging planes most closely resemble midline approaches, this view is limited by overhanging bone of the spinous processes and shadowing by the interspinous ligaments. Transverse imaging planes have been shown to be effective at lumbar interspaces for marking the needle insertion point and estimating needle depth to loss of resistance. However, these views are not helpful at midthoracic levels because of the narrower acoustic windows across the midline produced by the steep inclination of the spinous processes. In addition, the thoracic region lacks of prominent articular processes that can serve as sonographic landmarks. It can be difficult to obtain symmetric midline transverse views of the neuraxis (in particular, the rounded articular processes) in patients with scoliosis due to rotation of the spine.
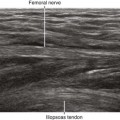
Ultrasound is an accurate imaging modality for depiction of the dura mater. The dura appears highly echogenic on ultrasound scans, defined by a single- or double-layer hyperechoic signal.8 It can be difficult to resolve the echo signals of the ligamentum flavum and posterior dura, and therefore this signal is sometimes referred to as the posterior complex (Table 55-1). The anterior complex consists of the anterior dura, posterior longitudinal ligament, and vertebral body. This produces a wider hyperechoic band that is deeper and parallel to the first band (the equals sign). Because the subarachnoid space contains few endogenous scatterers of ultrasound, it appears echo free on ultrasound scans (Table 55-2).
Table 55-1 Anatomic Structures that Comprise the Posterior and Anterior Echo Complexes as Seen in Longitudinal Paramedian View of the Neuraxis (the “Equals Sign”)*
| Ultrasound Image | Structure |
|---|---|
| Posterior complex | Get Clinical Tree app for offline access 
|