29
Neurologic Applications
Eugene C. Lin and Abass Alavi
Positron emission tomography (PET) is useful in lateralizing epileptogenic foci in patients with equivocal clinical, electroencephalographic (EEG), and magnetic resonance imaging (MRI) examinations. PET does not add value in patients localized by ictal scalp EEG and MRI.2
- Ipsilateral PET hypometabolism is an indicator for good postoperative outcome in the presurgical evaluation of drug-resistant temporal lobe epilepsy. Ipsilateral PET hypometabolism has a predictive value of 86% for good outcome (80% in patients with a normal MRI and 72% in patients with a non-localized scalp EEG).2
- PET is more accurate for temporal epilepsy.
- Interictal PET
- Temporal lobe epilepsy. Sensitivity 84%, specificity 86%
- Extratemporal lobe epilepsy. Sensitivity 33%, specificity 95%
- Interictal PET is more sensitive than interictal single-photon emission computed tomography (SPECT) but less sensitive than ictal SPECT.
- SPECT. Temporal epilepsy:
- Ictal SPECT. Sensitivity 90%, specificity 73%
- Interictal SPECT. Sensitivity 66%, specificity 68%
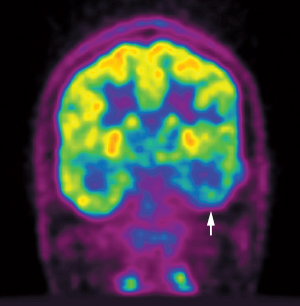
- In the interictal state, the involved region will be hypometabolic (Fig. 29.1). The extent of hypometabolism may be a dynamic process related to the frequency of seizures.7 During ictus, the involved region is hypermetabolic.
- Temporal lobe hypometabolism usually involves the entire temporal lobe.
- Lateral hypometabolism may be more pronounced.
- Even if a focal lesion is present on anatomical images, the temporal lobe hypometabolism is usually diffuse.
- MRI negative PET is accurate even when there is no MRI evidence of mesial temporal sclerosis.8 In patients with a negative MRI, the hypometabolism tends to involve the inferolateral temporal lobe rather than the mesial temporal lobe.9
- Contralateral temporal lobe. Rarely, the temporal lobe contralateral to the seizure focus may appear mildly hypermetabolic.
- Interpretation criteria. In patients with suspected temporal lobe epilepsy, any degree of hypometabolism on visual inspection should be considered significant. A quantitative difference of 15% or more between the temporal lobes is usually significant.10
- Extratemporal hypometabolism. Ipsilateral extratemporal hypometabolism is relatively common.
- The hypometabolism is most common in the thalamus and very uncommon in the occipital lobes and basal ganglia. The greatest degree of hypometabolism is seen in the ipsilateral frontal lobe.11
- Bilateral cerebellar hypometabolism is common, which is likely related to chronic use of antiepilepsy drugs. Crossed cerebellar diaschisis contralateral to the seizure focus can also be seen.12
- Extratemporal areas of cortical hypometabolism are usually contiguous with each other and the main site in the temporal lobe.
- Extratemporal hypometabolism is less severe than the temporal hypometabolism.
- Thalamic hypometabolism1
- Ipsilateral thalamic hypometabolism is associated with long-standing epilepsy and secondary generalization of seizures.
- Contralateral thalamic hypometabolism is a predictor of a higher risk of postoperative seizures.
- Prognosis. Unilateral focal temporal hypometabolism is associated with a good surgical outcome. Symmetric bilateral temporal, extratemporal, or thalamic hypometabolism is associated with a higher incidence of postoperative seizures.13
- Localization. PET is primarily useful in lateralizing the epileptogenic focus rather than in exact localization. As hypometabolism often diffusely involves the temporal lobe and extends into extratemporal regions, hypometabolism on PET should not guide the extent of surgical resection without further supportive evidence.8
- Intracranial electrodes. Intracranial electrode insertion can cause areas of hypometabolism.
- PET should be performed before intracranial electroencephalogram.
- Subclinical seizures. Unrecognized subclinical seizure activity during the administration of FDG can result in false-positive apparent hypometabolism in the contralateral temporal lobe (relative to the ictal hypermetabolism in the involved temporal lobe). Therefore, patients should be monitored if possible before the dose is injected.
- Children. Interictal hypermetabolism in the seizure focus can occur in children, but rarely in adults.
- Focal cortical malformations. Focal cortical malformations can be associated with decreased, normal, or increased uptake. Focal subcortical heterotopia and lobar dysplasia can be associated with increased uptake on interictal PET.14
PET is the most valuable imaging study for patients with suspected Alzheimer disease (AD) with mild to moderate cognitive impairment, who (1) meet standard criteria for dementia without identifiable cause after full work-up or (2) exhibit progressive cognitive dysfunction during a period of observation.
PET can be helpful in
- Differentiation. Differentiating AD from other dementias
- Diagnosis. Aiding in the diagnosis of early AD
- Prognosis. The degree of hypometabolism seen on PET correlates with rate the degree of cognitive decline after the study.
- PET. Sensitivity 86%, specificity 86%17
- PET is sensitive for differentiating both AD versus normal and AD versus non-AD disorders.
- Early AD. Decreased metabolism in the parietotemporal areas predicts decline, with an overall accuracy of 86% and sensitivity and specificity ranging from 75 to 100%.15,18
- SPECT. PET is ~15 to 20% more accurate than SPECT.15
- PET is superior to SPECT in differentiating AD from vascular and other dementias.
- Interpretation criteria for a positive study19
- Bilateral symmetric temporoparietal hypometabolism (Fig. 29.2)
- Parietal activity is usually decreased more than temporal activity.
- Posterior cingulate cortex hypometabolism
- Hypometabolism may be asymmetric or unilateral early during the disease (Fig. 29.3).
- Hypometabolism can involve frontal lobes in advanced disease (Fig. 29.4).
- Frontal lobe abnormalities are not seen without temporoparietal disease.
- Preserved metabolism in the sensorimotor and visual cortices (Fig. 29.2), cerebellum, basal ganglia, and thalamus
- Cerebellar activity remains constant throughout the stages of the disease; therefore, it can be used as a reference point for generating semiquantitative in dices for affected sites.
- Glucose metabolism is lower throughout the cortex in patients with AD compared with normal individuals.20
- Differentiation from other dementias. AD can usually be differentiated from
- Frontotemporal dementia (Pick disease).15 Frontal and temporal hypometabolism is the dominant pattern (Fig. 29.5).
- Reduced activity in the posterior cingulate cortex seen in AD is not noted in frontotemporal dementia.21 Anterior cingulate hypometabolism is often seen in frontotemporal dementia.22
- Frontotemporal dementia affects the anterior and me dial temporal more than lateral temporal cortices.
- The greatest decrease is often in the medial frontal cortices.
- There is relative sparing of parietal lobes in frontotemporal dementia.
- Vascular dementia (multi-infarct dementia). Multiple focal cortical and subcortical defects are seen in this type of dementia.
- Areas of decreased metabolism differentiating vascular dementia from AD are the deep gray nuclei, cerebellum, primary cortices, middle temporal gyrus, and anterior cingulate gyrus.23
- Note that these defects should be accounted for by areas of abnormal signal on MRI. If these defects have no MRI correlate, this pattern could suggest a primary neurodegenerative disorder rather than vascular dementia.15
- However, frontal lobe metabolism is usually decreased in patients with white matter signal abnormalities on MRI secondary to subcortical ischemic vascular disease, regardless of the location of the signal abnormalities.24
- Early versus late-onset AD. Glucose metabolism is most severely affected in the parietal, frontal, posterior cingulate cortices, and subcortical area in early-onset AD and in the limbic system and medial frontal lobe in late-onset AD.25,26 The overall hypometabolism in early-onset AD is greater in magnitude and extent.26
 Seizure Localization1
Seizure Localization1 Dementia: Alzheimer Disease15,16
Dementia: Alzheimer Disease15,16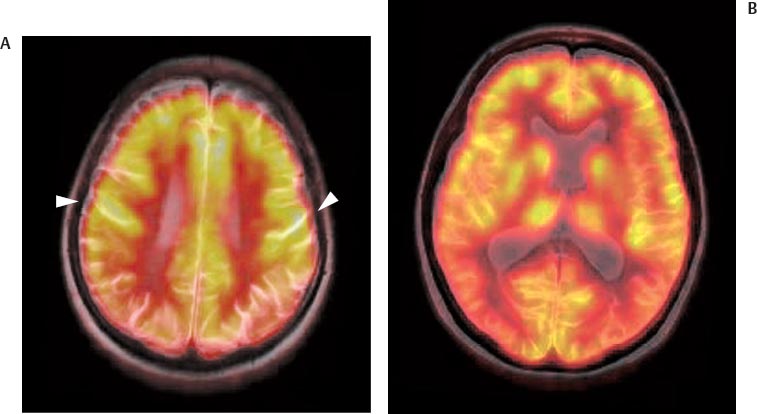
![]()