Neurologic Interventions, Ultrasound-Guided Regional Anesthesia Ultrasonography is increasingly employed as an imaging and guidance modality for regional anesthesia and is becoming an important tool in the everyday practice of anesthesiology. When ultrasound-guided nerve blocks were introduced in the mid-1990s, the advantages of this new technique were obvious.1,2 Ultrasound guidance enables the operator to visualize targeted structures and selectively block them. A large number of ultrasound-guided nerve block techniques were described in subsequent years. The clinical application of ultrasound-guided nerve blocks requires state-of-the-art imaging equipment and an adequate level of training. The operator should be well versed in the anatomy of the targeted structures and have the technical expertise necessary to image the structures of interest with the ultrasound machine. After Carl Koller performed the first ocular local anesthesia in 1884, the practice of regional anesthesia relied for more than a century on surface landmarks, reference lines, and intersecting lines for orientation purposes. But human anatomy is highly variable and cannot always be accurately predicted, with the result that many peripheral nerve blocks were unsuccessful. Sonography was introduced as a means of solving this problem. A Doppler ultrasound blood-flow detector was first used in 1978 to facilitate the supraclavicular brachial plexus block.3 Sonography was first used for the direct imaging guidance of a brachial plexus block in 1994, again using the supraclavicular approach.1 During the past 10 years, ultrasound technology has continued to evolve in its application to regional anesthesia techniques. New scanners and software have also been developed with the goal of facilitating peripheral nerve blocks. Published data Since the first ultrasound-guided peripheral regional anesthesia was performed in 1994,1 this field has continued to develop from year to year. Ultrasound guidance has resulted in higher success rates, lower complication rates, and improved patient safety and comfort.4–7 Several randomized studies and case series have been published in the past decade dealing with the improvement of ultrasound-guided peripheral nerve blocks. Regional anesthesia can be used in surgical patients either as an adjunct to general anesthesia or as a stand-alone anesthesia procedure when possible contraindications are taken into account. Procedures in the distribution of the brachial plexus (e.g., a radial fracture or shoulder arthroscopy) can be performed by targeting the anesthesia to specific nerves that are visualized with ultrasound.8 Of course, this same principle can be applied to procedures in the distribution of the lumbosacral plexus, such as the ultrasound-guided placement of a femoral nerve catheter during major knee surgery.9 Ultrasound can also direct the placement of a catheter for postoperative analgesia10 and to facilitate postoperative mobilization of the treated limb. Single-shot techniques should employ long-acting local anesthetics and should be supplemented by the use of nonopioid analgesics (e.g., ibuprofen, diclofenac, metamizole). Refusal of informed consent is recognized as a general absolute contraindication to the use of regional anesthesia. Clinically overt coagulation disorders are generally a contraindication to proximal peripheral nerve blocks, although a nerve block may still be performed in selected cases where the benefit outweighs the risk. Regarding the use of anticoagulant medications, there are no randomized studies or guidelines like those for spinal anesthesia techniques, except for the psoas compartment block. Only recommendations have been published. There are some illustrative case reports, however, showing that peripheral nerve block catheters were used safely in patients on anticoagulant medication.11 On the other hand, there is an increased theoretical risk that injury to the epineurium will cause hematoma or microhematoma formation in patients on anticoagulant medication. The German Society of Anesthesiology and Intensive Care Medicine has published recommendations on the use of peripheral nerve blocks for regional anesthesia in patients receiving thromboembolic prophylaxis. Available data form the basis of the following guidelines for peripheral nerve blocks in settings of thromboembolic prophylaxis and antithrombotic medication12: Whenever possible, the same precautionary measures followed for spinal anesthesia should also apply to peripheral nerve blocks. If these measures cannot be implemented, a careful risk–benefit analysis should be conducted for each individual case. Considerations in performing a peripheral nerve block in a patient on anticoagulant medication should be discussed with the patient and documented in writing. All techniques that involve a deliberate vascular puncture (e.g., transarterial techniques) should be avoided. Patients taking aspirin, NSAIDs, or low–molecular-weight heparin (in the absence of other coagulation-inhibiting agents and no clinical signs of coagulopathy) are considered better candidates for regional anesthesia than patients treated with fondaparinux, clopidogrel, or ticlopidine. Superficial nerve blocks that are easily accessible to compression, and the very rare blocks that require vascular puncture, can be performed more safely in patients on anticoagulant medication than can deep nerve blocks in joints not accessible to compression. The following blocks can usually be performed safely in patients on thromboembolic prophylaxis or antiplatelet drugs: Axillary plexus block (excluding the transarterial technique) Interscalene plexus block (use only techniques that do not risk vertebral artery puncture, such as the Meier technique) 3-in-1 block (femoral nerve block) Distal sciatic nerve block (posterior or lateral approach) All nerve blocks about the elbow and knee and distal to those joints An infection at the puncture site is an absolute contraindication, although ultrasound can be used to locate a different puncture site that is outside the infected area but still gives access to the site of the desired nerve block. Catheter placement is contraindicated in patients with a systemic infection (and possible bacteremia).13,14 An existing neurologic deficit in the area of the proposed peripheral nerve block is only a relative contraindication. Precise, detailed documentation and evaluation of the patient’s neurologic status is essential. An immediate postoperative evaluation of neurologic function is necessary to exclude a reversible cause.15 In the out-of-plane technique, the needle is inserted and advanced in a short-axis plane perpendicular to the ultrasound image plane (▶ Fig. 29.1). The needle is imaged in cross-section as an echogenic structure with a distal acoustic shadow. In most cases only the needle tip can be visualized. The angle of needle insertion is adjusted according to the depth of the target structures: the needle is inserted at a low angle for superficial blocks and at a steeper angle for deeper blocks. A steeper insertion angle allows better visualization of the needle tip than a flatter angle. Fig. 29.1 Out-of-plane technique of needle insertion. In the in-plane technique, the needle is inserted in a long-axis view that is in-plane with the ultrasound beam (▶ Fig. 29.2). The entire needle can be visualized, but only if the plane of needle insertion precisely coincides with the ultrasound image plane. In this technique the needle tip can be localized at any time, significantly reducing the risk of neurovascular injury.16 A low insertion angle will provide better needle visualization than a steeper angle. The distance from the insertion site to the target structure is 2 to 3 times longer in the in-plane technique than in the out-of-plane technique. Fig. 29.2 In-plane technique of needle insertion. Given the multitude of neural structures that exist in the human body, nerves have a variety of ultrasound appearances depending on their location. Proximal nerves appear as hypoechoic structures with a hyperechoic rim (e.g., interscalene brachial plexus C5 to T1). Nerves at more distal sites appear hyperechoic (e.g., ulnar nerve) due to a larger proportion of connective tissue between the neurons. But echogenicity also varies with the ultrasound beam angle, a phenomenon known as anisotropy. Nerves also present typical geometric shapes at ultrasound, which may be described as round, oval, or triangular. Thus, the exact description of a nerve imaged with ultrasound depends on its geometry and echogenicity. Muscles appear sonographically as heterogeneous structures with interspersed hyperechoic lines (intramuscular septa) or as homogeneous structures. Generally speaking, muscles have a fibrolamellar appearance when imaged with ultrasound. A number of manufacturers offer ultrasound systems specially designed for use in anesthesiology (e.g., ▶ Fig. 29.3). Nerve blocks can be guided with small portable ultrasound machines or with larger stationary systems, which often provide better contrast resolution. Fig. 29.3 Logiq E9 ultrasound system. Manufacturers such as Pajunk and Braun supply a variety of different injection needles and catheters for use in regional anesthesia (▶ Fig. 29.4, ▶ Table 29.1). These devices may consist of single-injection needles, with or without nerve stimulation, or catheter sets for administering continuous regional anesthesia. Fig. 29.4 Regional anesthesia needles. The interscalene brachial plexus block was first described by Winnie in 1970.17 It is used for the reduction of shoulder dislocations, for shoulder arthroscopy, for shoulder replacement arthroplasty as an adjunct to general anesthesia, and for intra- and postoperative shoulder mobilization. The technique can also be used for procedures on the lateral clavicle and upper arm. Whether the block is used alone or combined with general anesthesia depends on the operation, since the inside of the upper arm is partially supplied by portions of the intercostobrachial nerve (T12), requiring an additional block. An incomplete block during shoulder surgery18 is attributable to incomplete anesthesia of the suprascapular nerve (C5). But all the roots of the brachial plexus (C5–T1) can be visualized with ultrasound and can be selectively blocked under sonographic guidance. The indications for an interscalene brachial plexus block are as follows: Reduction of a shoulder dislocation Anesthesia and analgesia for shoulder surgery and for operations involving the lateral clavicle and upper arm The interscalene brachial plexus block has the following contraindications: Contralateral phrenic nerve palsy Contralateral recurrent laryngeal nerve palsy Possible complications include the following: Horner syndrome (blockade of the stellate ganglion: myosis, ptosis, and enophthalmos) Phrenic nerve palsy: the phrenic nerve (C4) runs down the anterior border of the anterior scalene muscle. Recurrent laryngeal nerve palsy Bezold–Jarish reflex: in some patients, the beach-chair position used for shoulder surgery evokes bradycardia and hypotension that may lead to circulatory collapse and cardiac arrest.19 The patient is positioned supine with the head resting on a soft gel cushion and turned slightly toward the contralateral side. The skin site is aseptically prepared as described in Chapter ▶ 8. To define the neural structures of the brachial plexus, the transducer is placed parallel to the clavicle in the supraclavicular fossa. The subclavian artery is identified as a pulsating vascular structure. The pleura appears as a hyperechoic structure below the subclavian artery. The brachial plexus appears lateral to the subclavian artery as a cluster of small hypoechoic structures with a hyperechoic outer rim (▶ Fig. 29.5). Sliding the transducer cephalad will trace the brachial plexus into the interscalene groove and display 3 to 5 hypoechoic round or oval structures arranged in a string-of-beads pattern: the C5–T1 nerve roots. The needle is advanced in a lateral-to-medial direction using either the out-of-plane or in-plane technique. Injecting 20 mL of local anesthetic is usually sufficient to block the nerve roots. Following spread of the local anesthetic, a catheter can additionally be placed to facilitate postoperative mobilization of the shoulder and arm. Fig. 29.5 a, b Ultrasound appearance of the interscalene portion of the brachial plexus (C5–T1).MSC, sternocleidomastoid muscle; MSM, middle scalene (MSM); MSA, anterior scalene; AC, carotid artery; VJI, internal jugular vein. Goebel et al20 conducted a randomized, placebo-controlled study in 70 patients to investigate postoperative analgesia following the placement of an interscalene plexus catheter. The patients who received 0.2% ropivacaine by continuous infusion for postoperative analgesia had less need for opioid rescue medication during the first 24 hours after shoulder surgery than the group of patients who received a 0.9% saline solution via the catheter. The interscalene plexus block and catheter placement were performed under ultrasound guidance. Mariano et al21 studied 32 patients who also received an interscalene plexus catheter for postoperative analgesia, but the posterior approach described by Pippa22 was used. The nerve block was performed with ultrasound assistance. The study indicates that either approach can provide an effective blockade of the interscalene brachial plexus. The supraclavicular technique of the brachial plexus block was first described by Kulenkampff in 1911. Because this approach entails a risk of pneumothorax due to its proximity to the pleura, several attempts have been made to refine the technique.23,24 Ultrasound guidance can be used to direct the needle to the target site under vision and minimize the risk of this complication. The supraclavicular brachial plexus block is used to produce anesthesia and analgesia of the upper arm, forearm, and hand (e.g., humeral shaft fracture, elbow fracture or dislocation). The supraclavicular nerve block has the following contraindications: Contralateral phrenic nerve palsy Contralateral recurrent laryngeal nerve palsy Possible complications are as follows: Pneumothorax Horner syndrome Phrenic nerve palsy Recurrent laryngeal nerve palsy The patient is positioned supine with the head placed on a soft gel cushion and turned slightly toward the contralateral side. The skin site is prepared as described in Chapter ▶ 8. The anesthesiologist stands at the head of the table and places the transducer in the supraclavicular fossa parallel to the clavicle. The subclavian artery is identified as a pulsating echo-free structure (▶ Fig. 29.6). Just below the subclavian artery, the first rib appears as a hyperechoic line with an acoustic shadow. Lateral to the subclavian artery are small, hypoechoic oval structures representing the nerve bundle of the supraclavicular plexus. Angling the transducer reveals a second hyperechoic white line, offset from the first, which represents the pleura. It is critically important to identify both lines in order to distinguish the pleura from the first rib and reduce the risk of pneumothorax. Angling the transducer alters the ultrasound image as the hyperechoic line with the posterior shadow moves laterally and the second hyperechoic line appears below the subclavian artery. The needle is inserted in a lateral-to-medial direction using the in-plane technique, which is preferred as it gives better visualization of the needle tip. Just 20 mL of local anesthetic is sufficient to produce adequate anesthesia and analgesia, making certain that both the posterior and anterior portions of the supraclavicular plexus are anesthetized. The needle is initially directed toward the first rib to avoid piercing the pleura. Then the needle is retracted and the anterior branches of the supraclavicular plexus are anesthetized. Fig. 29.6 a, b Subclavian vein (VS), subclavian artery (AS), lateral brachial plexus. Perlas et al25 studied 510 patients who received a supraclavicular brachial plexus block for upper limb surgery. A successful block was achieved in 94.6% of the cases reviewed. A medial-to-lateral approach was used in 361 patients and a lateral-to-medial approach in 149. The medial-to-lateral approach was associated with 2 cases of iatrogenic vascular injury and 2 cases of postoperative numbness that persisted for days after the surgery. No puncture-related complications occurred with the lateral-to-medial approach. There were no instances of pneumothorax in either group. We accordingly also prefer the lateral-to-medial approach. The needle was introduced by the in-plane approach for better visualization of the needle tip. The infraclavicular brachial plexus block is a simple method of producing anesthesia and analgesia of the upper limbs. It is useful in cases where a high arm block is desired for surgery. The needle is inserted using the in-plane technique. One disadvantage of the infraclavicular nerve block is the risk of iatrogenic pleural injury and the development of pneumothorax. One advantage from an anatomical standpoint is the more proximal level of the approach. In contrast to the axillary approach, this eliminates the need for separate anesthesia of the musculocutaneous nerve, which emerges from the lateral fascicle. Indications for the infraclavicular brachial plexus block are anesthesia and analgesia from the distal upper arm to the hand. The infraclavicular brachial plexus block has the following contraindications: Contralateral pneumothorax Contralateral phrenic nerve palsy Contralateral recurrent laryngeal nerve palsy Previous contralateral pneumonectomy Possible complications include: Pneumothorax Horner syndrome Phrenic nerve palsy
29.1 History and Development
29.2 Indications
29.3 Contraindications
29.3.1 Patient Refusal
29.3.2 Clinically Overt Coagulopathy and Anticoagulant Medication
29.3.3 Infections at the Puncture Site
29.3.4 Neurologic Deficit
29.4 Needle Insertion Techniques
29.4.1 Out-of-Plane versus In-Plane Technique


29.5 Ultrasound Imaging of Nerves and Muscles
29.5.1 Nerves
29.5.2 Muscles
29.6 Materials and Equipment
29.6.1 Ultrasound Machines

29.6.2 Anesthesia Needles and Catheters
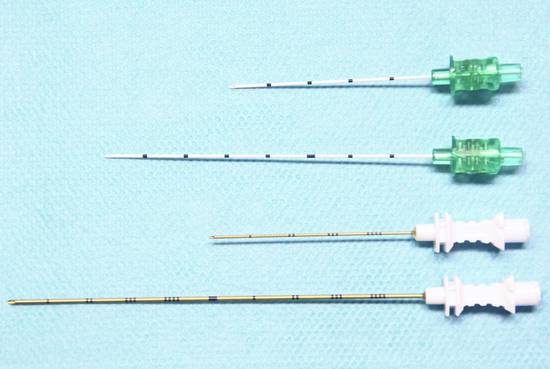
Company
Needle gauge
Needle length (mm)
Needle tip
Special features
Pajunk
22
50
Faceted bevel, Sprotte
“Cornerstone” reflectors reflect ultrasound beam without energy loss
Braun
22
50/80
15° bevel geometry, 30° bevel geometry
Pajunk
19
50
Faceted bevel, Sprotte, Tuohy
Suitable for catheter technique
Pajunk
19
100
Faceted bevel, Sprotte, Tuohy
Suitable for catheter technique
29.7 Regional Anesthesia at Specific Sites: Upper Limb
29.7.1 Brachial Plexus
Interscalene Brachial Plexus Block
Indications
Contraindications
Complications
Patient Position
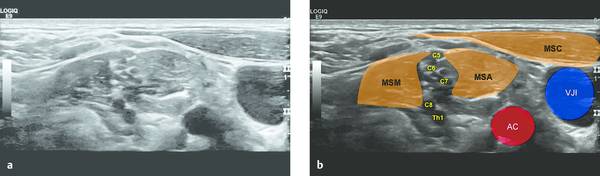
Sonography
Literature on the Interscalene Brachial Plexus Block
Supraclavicular Brachial Plexus Block
Indications
Contraindications
Complications
Patient Position
Sonography

Literature on the Supraclavicular Brachial Plexus Block
29.7.2 Infraclavicular Brachial Plexus Block
Indications
Contraindications
Complications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








