Percutaneous Sclerotherapy of Cysts
16.1 Percutaneous Sclerotherapy of Liver Cysts
16.1.1 Epidemiology and Etiology
The incidence of liver cysts is age-dependent and was up to 5% in our study of 20,000 consecutive patients. Other authors have reported similar values of 1 to 3%.1,2
Liver cysts with a multifactorial cause may consist of cystic dilatations of intralobular bile ducts, which are more common in females (von Meyenburg anomalies), or may be an expression of congenital changes. A polycystic liver has a high association with renal cysts (75%, again depending on age). Associations with cysts in other organs are much less common. A small percentage of patients have coexisting anomalies (e.g., spina bifida).
Symptoms are rare and usually do not appear until the fourth or fifth decade of life. However, palpable organ enlargement may create a pressure sensation; compression of the gastrointestinal tract, veins (peripheral edema), and portal venous vessels (signs of portal hypertension); and other problems that may require treatment. Spontaneous or trauma-induced rupture (or intracystic hemorrhage) may be a source of unexplained pain.
16.1.2 Symptoms
Liver cysts are asymptomatic in most patients. The most common symptom is pain, which may be accompanied by abdominal distention after meals. Other symptoms are dyspepsia and weight loss. Small meals can help to prevent undesired excessive gastric filling. Cyst infection and intracystic hemorrhage occasionally occur. Biliary tract obstruction has been observed in isolated cases.
16.1.3 Indications
The need for treatment depends on the symptoms, the size of the cyst (>50–100 mm), and the risk of rupture (large superficial cysts). Asymptomatic cysts generally are not treated. Exceptions are small subcapsular cysts located at sites exposed to mechanical stresses (beneath the ribs or sternum), which may occasionally cause complaints. Other causes of pain should be excluded (gastritis, ulcer disease, cholelithiasis, pancreatitis, vertebragenic pain, etc.). It is important to recognize an atypical gallbladder location, segmental biliary tract dilatation, or portal vein thrombosis prior to interventional treatment, especially in patients with a polycystic liver. The diagnosis and treatment of cystic pancreatic lesions are described in Chapter ▶ 22.3
16.1.4 Contraindications
Interventional treatment is contraindicated in patients with positive echinococcal serology, who would require PAIR (puncture–aspiration–injection of alcohol–reaspiration, see Chapter ▶ 17) or some other preliminary treatment.4 Planned liver transplantation is another relative contraindication.
16.1.5 Interventional Materials and Equipment
Necessary materials and equipment are described in Chapters ▶ 2 and ▶ 15 and in the text.5 The following are required:
Local anesthesia (standard technique)
Various drainage sets are available such as a nephrostomy set (OptiMed), 6.6F (2.2 mm) with a metal wire and dilator
Sclerosing agent of choice: 1% polidocanol (Aethoxysklerol, Kreussler Pharma), Reg. No. A 1122–2
Adhesive tape for catheter fixation
Suture material (generally unnecessary): Ethicon Mersilene green, FSL 30 mm 3/8c (Johnson & Johnson)
16.1.6 Sclerosing Agents
As described for other interventions, cysts can be sclerosed with 96% alcohol,6 1% polidocanol (preferred for its local anesthetic properties, less painful than alcohol), or 10% (to 30%) NaCl solution. Tetracycline, doxycycline, and minocycline are common pleurodesis agents that may also be considered7,8; 50% acetic acid has been used for renal cysts.9
16.1.7 Treatment Options
Surgical interventions are available for the symptomatic reduction of liver cyst size (by cyst fenestration or resection), although there is a potential for significant postoperative complications.10 Another treatment option is ultrasound-guided percutaneous cyst aspiration followed by the instillation of a sclerosing agent.
16.1.8 Technique for Percutaneous Sclerotherapy of a Liver Cyst
Skin Preparation and Local Anesthesia
Skin preparation and local anesthesia follow standard protocols described elsewhere in this book (e.g., Chapter ▶ 15).
Cyst Aspiration and Drain Insertion
A Chiba needle (20 gauge, 220 mm) is introduced into the cyst under ultrasound guidance and advanced into the distal third of the cyst, stopping short of the far wall.11 The trocar is removed to permit a diagnostic aspiration. When an adequate sample has been collected, a 0.018-inch metal guidewire with a soft tip is inserted into the cyst and coiled 1 to 3 times to secure its placement. The needle is removed, leaving the wire inside the cyst, and the tract is dilated over the wire (using the dilator contained in the set) to accommodate a 6F (or 5F) catheter, which is passed deep into the cyst with a slight twisting motion. When it has been confirmed that the catheter is inside the cyst with its tip on the far wall, the wire is removed. The catheter may now be fixed to the skin with adhesive tape (or sutures), depending on further intended measures.
Generally the cyst contents will drain spontaneously through the 6F catheter, which is left indwelling for several hours or overnight. Alternatively, the cyst contents may be completely evacuated with syringes and the aspirated volume measured. If the fluid is clear or amber-colored, it is highly unlikely that the cyst communicates with the biliary tract. One aliquot should be routinely collected for cytologic analysis (blood count [cell count], microbiology, and biluribin level are optional). A yellowish or dark-greenish tint suggests a biliary communication and cause; these cysts should be aspirated and drained and the bilirubin level determined. The optional instillation of radiopaque contrast medium (or SonoVue [Bracco]12) may be done to exclude a connection with the biliary tree. Contrast medium should not enter the bile ducts; if it does, sclerotherapy is contraindicated. A feared complication is sclerosing cholangitis, which has been observed following the intracystic injection of scolicidal solution.13 Biliary tract communication will cause cysts to refill within a remarkably short time, often in a matter of hours or days.
Brown or reddish-brown cyst contents suggest an (old) intracystic hemorrhage. Other types of discoloration will additionally require bacteriologic testing if a prior infection is suspected. Complicated cysts should be copiously irrigated with sterile 0.9% NaCl before they are sclerosed with 1% polidocanol, which reportedly has slight bactericidal activity.
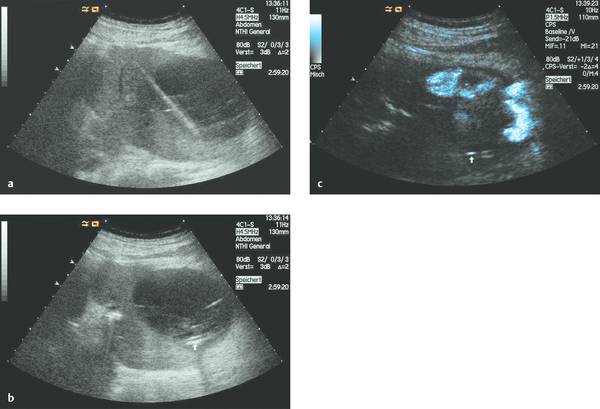
16.2 Sclerotherapy Technique
Before sclerotherapy, correct drain placement is confirmed by administering 10 to 20 mL of 0.9% NaCl and reaspirating under ultrasound guidance (▶ Fig. 16.1). Next the sclerosing agent is administered. In the case of polidocanol, for example, the solution is instilled over 15 to 60 minutes followed by reaspiration. If reaspiration is unsuccessful, it can be facilitated by respiratory maneuvers, coughing, position changes, repositioning (retraction or rotation) of the drain, or the immediate infusion of 0.9% NaCl into the cyst to dilute its contents. The drain is removed following complete evacuation (or after about 2 hours).