Jean Noel Buy1 and Michel Ghossain2
(1)
Service Radiologie, Hopital Hotel-Dieu, Paris, France
(2)
Department of Radiology, Hotel Dieu de France, Beirut, Lebanon
15.2.1 Leiomyoma
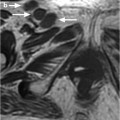
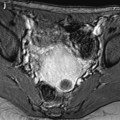
15.2.2 Leiomyosarcoma (Fig. )
15.2.3 Rhabdomyosarcoma
15.3.1 Hemangioma
15.3.2 Lymphangioma
15.3.3 Hemangioendothelial Sarcoma
15.5.1 Osteoma
15.5.2 Osteosarcoma
15.8.1 Adenomatoid Tumor
15.8.2 Peritoneal Mesothelioma
15.9.3 Gross Findings
15.10 Rete Cysts and Tumors
15.10.3 Gross Findings
15.11 Hamartomas
Abstract
Fibroma is the most common ovarian neoplasm of connective tissue origin and constitutes 2–% of ovarian neoplasms.
This group of tumor comprises a heterogeneous group of tumors that are not specific to the ovary (1).
Some of them are derived from the mesenchyme (see origin and definition of mesenchyme in chapter 1-1).
Mesenchymal tumors non specific to the ovary are composed of a single neoplastic mesenchymal element, either benign or malignant, in contrast to teratomatous or malignant mixed mesodermal tumors, which are usually composed of a number of tissue elements.
15.1 Tumors of Fibrous Tissue Origin
Fibroma is the most common ovarian neoplasm of connective tissue origin and constitutes 3%–5% of ovarian neoplasms (1).
Fibrosarcoma is very uncommon.
These tumors are described in Chap. 11.
Myxoma is a very rare tumor. At macroscopy, they are well encapsulated. Solid areas are slimy and viscous. Cystic spaces contain a viscous gelatinous material.
The tumors vary from poorly vascularized to tumors with prominent capillary vessels.
15.2 Tumors of Muscle Origin
15.2.1 Leiomyoma
It probably originates from smooth muscle present in the wall of blood vessels in the cortical stroma, in the corpus luteum, and in the ovarian ligaments at their point of attachment to the ovary.
Macroscopic and microscopic findings are identical to leiomyoma of the uterus (see Chap. 24).
On EVS, the mass is well delineated, with acoustic shadowings, and with a peripheral vascularization of regular vessels, more or less associated with a central vascularization (Fig. 15.1). Differential diagnosis is reported in Table 15.1.
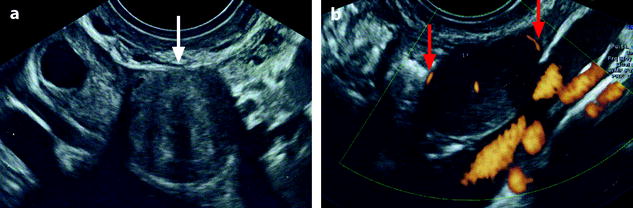
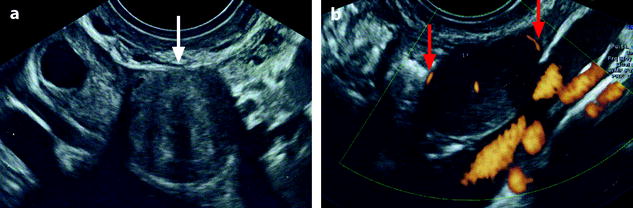
Fig. 15.1
Leiomyoma of the ovary. Forty-eight-year-old woman, with a previous history of breast carcinoma. EVS (a) displays a right ovarian mass of 1,8 cm in diameter (arrow), pushing the normal ovarian parenchyma toward the periphery. The mass is round, well delineated, a little less echogenic than the normal ovarian parenchyma, with some acoustic shadowings. On color Doppler (b), a regular peripheral rim of vessels (arrows), not usually seen in case of ovarian fibrothecoma, suggests the possibility of a leiomyoma. Coelioscopy, adnexectomy was performed. Pathology: leiomyoma of the ovary
Table 15.1
Differential diagnosis of ovarian leiomyoma
Common |
Subserosal uterine pedunculated leiomyoma |
Identical morphologic and vascular findings |
Identification or not of the ipsilateral ovary |