Infection of the vertebral column represents up to 20% of all osteomyelitis and is the most common infection of the axial skeleton. The presentation is often insidious. It is not uncommon for symptoms to be present for 6 to 8 weeks before being diagnosed. If ignored or misdiagnosed, infection of the spine can have a chronic, destructive, and significantly debilitating course. The general characteristics of spinal infections are summarized in Table 7-1 .
| Infection | Characteristics | Common Location |
|---|---|---|
| Vertebral osteomyelitis | Elderly and debilitated Male predominance | Lumbar more common than thoracic |
| Spinal epidural abscess | Hematogenous gram-positive cocci | Thoracic more common than lumbar |
| Diskitis | Adult postdiscectomy most common Rare in pediatrics; often accompanies chronic infections (e.g., cystic fibrosis) | Lumbar more common than thoracic |
| Granulomatous disease | Rare in developed countries | Thoracic approximately equal to lumbar |
Infection is commonly spread hematogenously, although direct extension from adjacent infection such as pneumonia or pyelonephritis is also possible. In 60% to 70% of patients the most common infectious agents encountered are gram-positive cocci, especially skin flora such as Staphylococcus (in about 60% of positive cultures), and less commonly Streptococcus with Peptostreptococcus , Escherichia coli , and Proteus . Although often implied by examination findings, a definitive infectious source is identified in less than 50% of patients with pyogenic spinal osteomyelitis. In unusual circumstances, such as immunodeficiency or patients from underdeveloped countries, one should consider atypical agents such as fungi or Mycobacteria .
Patients at risk include older adults, intravenous drug abusers, those with chronic illness, and those with a recent history of surgery, especially of the back or genitourinary system. Insidious onset of diffuse back pain (in 90%) and fever (in 50% to 70%) should suggest spinal infection. A history of recent back or genitourinary surgery, intravenous drug use, or infection of the soft tissue or respiratory or genitourinary system should increase the likelihood of spinal infection. Infection involves the vertebral body in 95% of cases, with the posterior elements being involved in less than 5%. Although neurologic symptoms such as radiculopathy may be present, they are uncommon and often present later in the course as the infection spreads from the disk and vertebra to the epidural, subarticular, and external foraminal spaces. Weight loss may also be present, but this constitutional symptom is less helpful in that it may also be associated with both inflammatory and neoplastic disease.
When thinking about where to look for infectious involvement of the vertebrae, it is helpful to consider the pathophysiologic manifestations. Blood-borne organisms seed from the vascular system. Intervertebral disks are the largest avascular organs in the body. The nucleus pulposus of the disk receives nutrients typically by diffusion from the subchondral vascular bed of the vertebral end plate. In addition, the outer annulus fibrosis has a direct capillary supply via spinal canal arteries, also contributing nutrients across the concentric fibrous layers of the annulus. The blood-borne organism is able to establish itself at the more vascular outer free margin of the disk and at the end plate in the capillaries of the subchondral vascular bed. From here the organism can spread contiguously into the more avascular central disk and into the adjacent bony vertebrae. Using this model, it is understandable that the earliest changes of infection should appear at the disk margin closest to the vascular source anteriorly and anterolaterally, as well as anywhere along the disk-margin interface. Advanced infection is characterized by an abnormal intervertebral disk and abnormal adjacent vertebral end plates.
Diagnostic Imaging
Plain Film
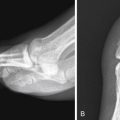
Initial imaging in the emergency department (ED) may include plain film and/or nonenhanced computed tomography (CT). Both are directed at identifying bony changes that may indicate infection of the vertebral bodies. Plain film has limited sensitivity because of many overlying confluent shadows and other technical difficulties in obtaining an image. Gross findings such as vertebral sclerosis, vertebral collapse with acute angulation of the spine (e.g., Pott disease with gibbous deformity [ Fig. 7-1 ]), or paraspinal soft tissue mass may be helpful, but the sensitivity is low and the images do not provide a complete evaluation of this potentially multifocal process.

Multidetector Computed Tomography
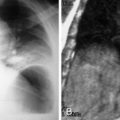
Sagittal reconstructions from CT provide greater diagnostic detail with respect to large-scale or multilevel osteomyelitis ( Fig. 7-2 ). On CT the acute or active infection may show low-attenuation paraspinal swelling and edema, focal fluid collections, fat stranding, or gas ( Fig. 7-3 ). Contrast administration may produce enhancement of the actively inflamed tissue with nonenhancing areas of central liquifactive debris in early abscess formation, if present. Attention should also be directed to adjacent organ systems such as the kidneys or lungs to provide clues to the origin of infection.