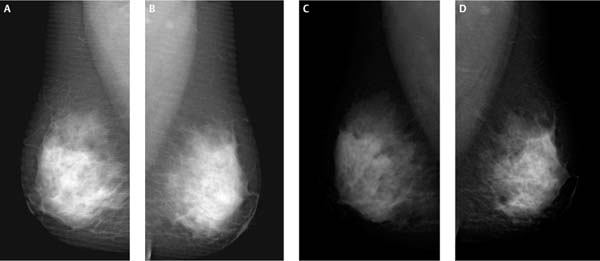
4 Normal Anatomy Normal breast anatomy is well displayed with digital mammography. The breast fibroglandular tissue is framed by numerous short arched lines. The internal pattern of the breast consists of fibroglandular tissue that forms a matrix of short curvilinear lines and longer trabecular lines that are oriented to the nipple. These lines coalesce to form a thin attachment to the nipple. The skin and the subcutaneous tissues generally are more visible with digital mammography than with screen-film technique.1,2 The skin is usually uniform and gradually thickens closer to the nipple. Variations in normal structures that are displayed by digital mammography can be confusing to imagers accustomed to screen-film displays. Although the nipple-areolar complex is generally symmetric bilaterally, there is sometimes normal or chronic asymmetric skin thickening or nipple inversion. Asymmetry may be due to poor patient positioning or compression. Even with good technique, the nipple-areolar complex may be asymmetric. In these cases, it is important to evaluate closely the skin, nipple, and subareolar fibroglandular tissue. On screening digital images, you can magnify, window, and level the display of this area to search for asymmetries, suspicious calcifications, or architectural distortion. Old films, even if they are screen-film, are useful for comparison because the asymmetry may prove to be chronic. If the patient is recalled, the nipple and skin should be visually inspected and compared with the contralateral side, and the patient should be questioned concerning nipple irritation, discharge, or skin changes. Spot magnification views are more sensitive for identifying subtle architectural distortions or suspicious calcifications. Besides providing better display of the skin and nipple, digital mammography is better at revealing structures in the retromammary space. Furthermore, digital mammography produces better image contrast and exposure with fewer artifacts.1,2 However, like screen-film mammography, digital mammography still requires monitoring for adequate clinical quality (Fig. 4–1). Figure 4–1 Mediolateral oblique (MLO) views. (A) Right MLO, (B) left MLO with grid lines, (C) right MLO, and (D) left MLO without grid lines. This study had been started when the technologist immediately noted that there were grid lines in the image that were due to improper lack of movement of the grid. After the grid mechanism was fixed, the lines were no longer present. Every year, the number of postprocessing methods and hanging protocol options available on digital workstations grows. The numerous choices may be daunting to those who are faced with developing a display protocol for the first time. One way to develop a protocol is to observe the activities that are currently performed when reading mammograms. These activities will vary depending on whether screening or diagnostic mammograms are being read. Additionally, the frequency of activities should be noted. For example, an activity that is performed on 100% of screening mammograms should clearly be part of a routine protocol. An activity that is performed less than 10% of the time may be omitted from the protocol and performed as needed. Initially, a screening protocol includes display of the four screening views. For soft copy digital screening, a preferred postprocessing program should be identified as the default for all screening exams to avoid missing any subtle abnormalities. The radiologist should then review these images in the same manner that the imager scans screen-film images. The current screening views are then displayed with a previous screening exam. If earlier exams are recorded on film, the radiologist reads the film from a multiviewer or light box adjacent to the soft copy workstation. The monitors should be adjusted to minimize reflected glare. If earlier exams are digital, then the earlier exam should be compared side by side on the digital soft copy display monitors. There are several different methods that can be used to display current and old exams. If you prefer large images, then the two mediolateral oblique (MLO) views from the earlier exam can be placed next to the two current exam MLOs on two monitors. If you do not mind smaller images, you may prefer to see four views—two craniocaudal (CC) views and two MLOs—from the earlier exam compared with the four views (two CCs and two MLOs) in the current exam; these eight images may be displayed in two horizontal rows, each containing four images. The actual size of each image is only slightly smaller than the usual screen-film image. When comparing the current exam to earlier exams, you can identify any subtle new asymmetry and assess the chronicity of lesions that have been identified with the initial evaluation of the screening views.
 Digital Mammographic Technique of Normal Breast
Digital Mammographic Technique of Normal Breast
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree