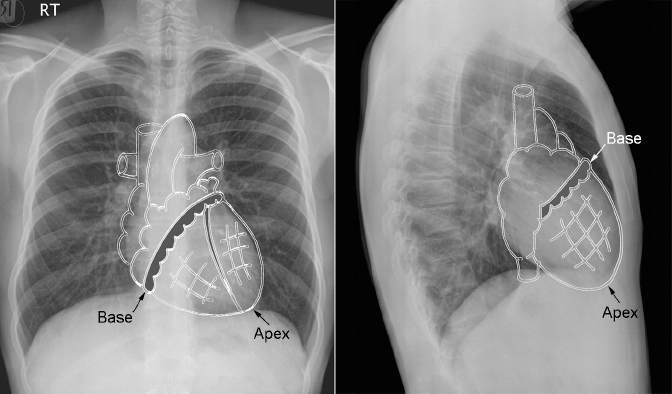
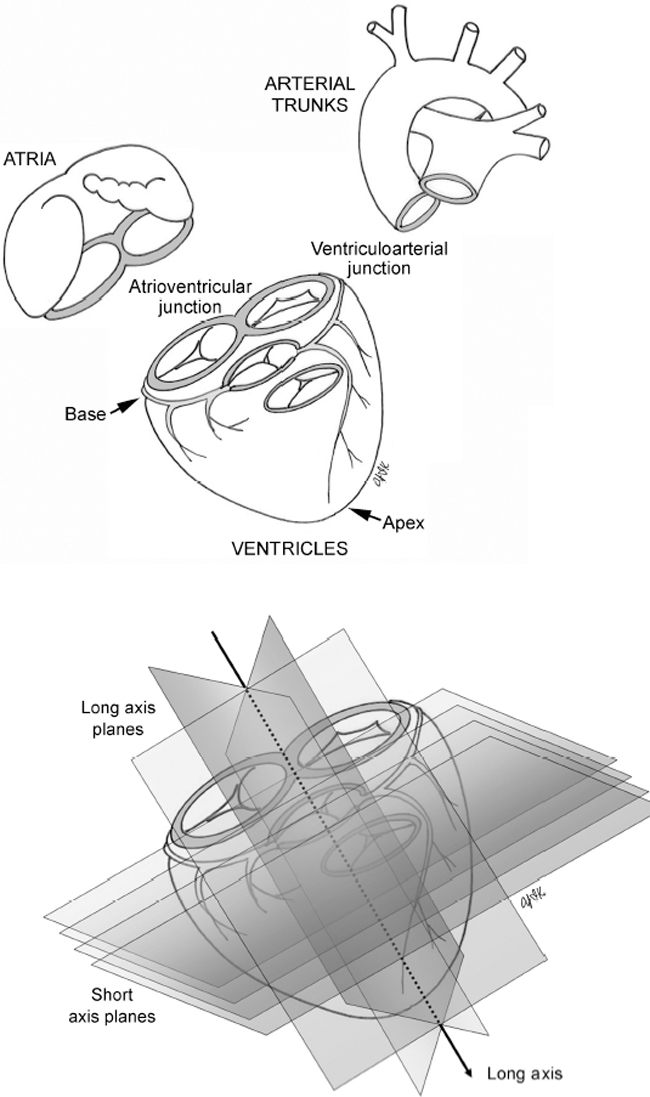
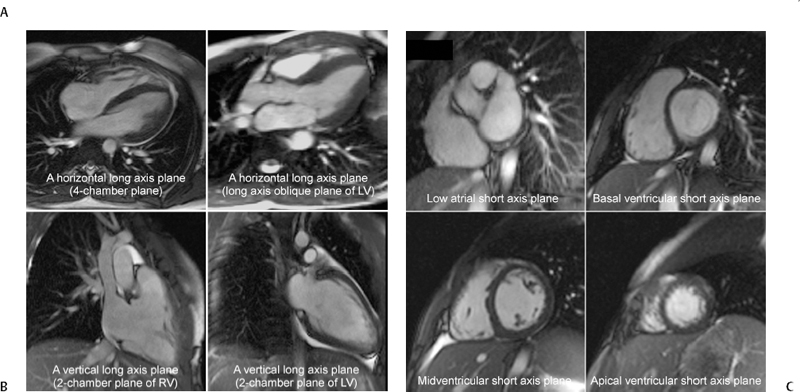
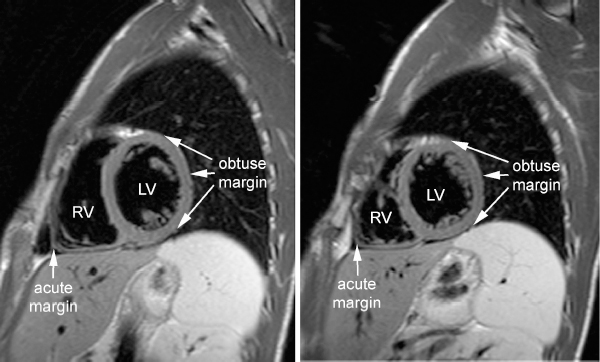
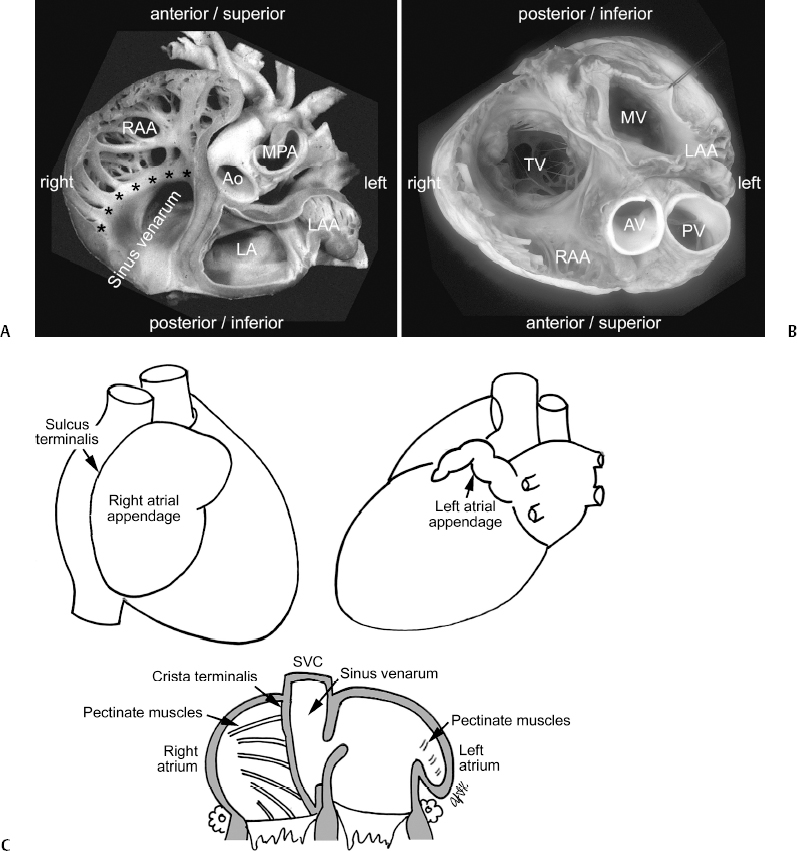
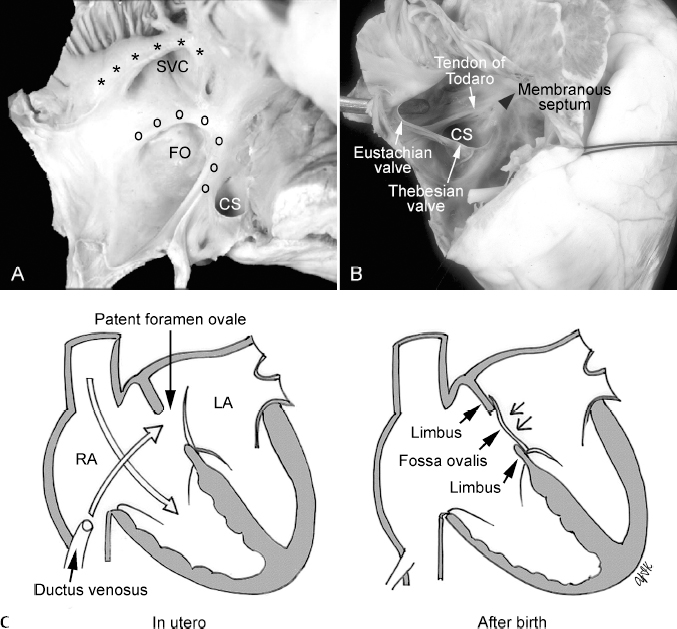
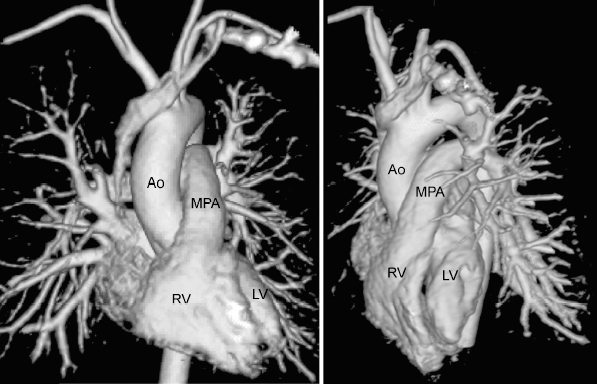
1 Normal Cardiovascular Anatomy for Imaging The heart lies within the pericardial sac in the mediastinum with two thirds placed to the left of the midline and one third to the right (Fig. 1.1). This asymmetric position of the heart within the thorax is called levocardia. The heart is shaped like an ice-cream cone that is tilted to the right and backward with its apex directed downward, to the left, and forward. The heart consists of three segments: the atria, the ventricles, and the arterial trunks (Fig. 1.2).1 The three segments are joined together at the atrioventricular and ventriculoarterial junctions that are guarded by valves. The four cardiac valves that demarcate these two junctions are arranged in a single plane. This plane is called the base of the heart or more precisely the base of the ventricles. The apex of the heart refers to the most pointed part of the ventricular mass. In the normal heart, it is composed of the tip of the left ventricle. The long axis of the heart is a line that connects the apex and the center of the base (Fig. 1.3A). The planes that are parallel to the long axis are called the long axis planes (Fig. 1.3B). The long axis planes that are oriented in a vertical plane to the body are called vertical long axis planes. The two-chamber views of the right and left ventricles are typical vertical long axis planes. The long axis planes that are oriented in a transverse plane to the body are called horizontal long axis planes. The four-chamber view is a typical horizontal long axis plane. The left ventricular long axis view is a plane midway between the vertical and horizontal planes. The planes that are perpendicular to the long axis are called the short axis planes. Examples are the atrial, basal ventricular, midventricular, and apical ventricular short axis planes (Fig. 1.3C). The ventricular part of the cardiac cone is not entirely circular. Its anterior surface is slightly convex, the posterior surface more rounded, and the inferior surface flat. The anteroinferior margin of the cardiac cone, which is composed of the right ventricle, forms an acute angle as it molds itself into the recess of the thoracic cage between the anterior chest wall and the diaphragm (Fig. 1.4). This part of the cardiac cone is therefore called the acute margin of the ventricular mass. In contrast, the posterior margin of the heart that is composed of the left ventricular free wall is called the obtuse margin as this part of the heart is more rounded. Externally, the four cardiac chambers are demarcated by grooves: the interatrial, interventricular, and atrioventricular grooves (Fig. 1.5). The atrioventricular and interventricular grooves are distinct as they contain a large amount of epicardial fat on which the major epicardial coronary arteries and veins are located. The interatrial groove is less distinct. Posteriorly, the interatrial and interventricular grooves are continuous with one another and are crossed by the atrioventricular groove. This point of intersection is called the crux cordis. Fig. 1.1 The heart is shaped like an ice-cream cone. The base of the cone is the atrioventricular junction and the apex is composed of the tip of the left ventricle. Fig. 1.2 Cardiac segments and junctions. (Modified from Anderson RH, Ho SY. Sequential segmental analysis—description and categorization for the millennium. Cardiol Young 1997;77:98–116). Fig. 1.3 Long and short axis planes of the heart. (A) Diagrammatic representation of the cardiac axis and planes. (B,C) Examples of magnetic resonance images obtained along the long and short axis planes. LV, left ventricle; RV, right ventricle. Fig. 1.4 Acute and obtuse margins of the ventricles shown on short axis magnetic resonance images. RV, right ventricle; LV, left ventricle. The base of the ventricles can be exposed by removing the atria and arterial trunks from the ventricles (Fig. 1.6). When the base of the heart is seen from above, the four cardiac valves are closely related to each other in a slanted plane. Familiarity with the arrangement of the cardiac valves in this plane facilitates the understanding of many important aspects of the cardiac anatomy. The atrioventricular valves, that is, the tricuspid and mitral valves, are located more posteriorly and inferiorly relative to the semilunar valves, that is, the aortic and pulmonary valves. The tricuspid valve is the most rightward and inferior valve and the mitral valve is the most posterior. The aortic valve has a deeply wedged position between the tricuspid and mitral valves. The pulmonary valve lies anterior and leftward of the aortic valve. The aortic valve is tilted slightly rightward and forward; the pulmonary valve is tilted slightly leftward and backward. The tricuspid, mitral, and aortic valves are firmly attached together through a dense fibrous tissue core called the central fibrous body. As will be discussed later in this chapter, the interventricular and atrioventricular membranous septum is the septal extension of the central fibrous body. The aortic and pulmonary valves, on the other hand, are loosely attached to each other. Fig. 1.5 Interatrial, interventricular, and atrioventricular (AV) grooves. The point where the atrioventricular groove is crossed by the interatrial and interventricular groove is called the crux cordis. The aortic and mitral valves are in direct contact with one another in the left ventricle. In the right ventricle, the pulmonary and tricuspid valves are apart from one another with an intervening fold of right ventricular myocardium called the crista supraventricularis.2,3 Because of the wedged position of the aortic valve between the tricuspid and mitral valves, the aortic and tricuspid valves, despite belonging to different ventricles, are in close proximity with only the membranous septum separating them. Therefore, a pathologic defect in the membranous septum brings the aortic and tricuspid valves in direct contact with each other. Fig. 1.6 Photographs and drawings showing the base of the ventricles seen from above (left panel) and below (right panel). The arterial trunks and atria are removed above the valve and the apical parts of the ventricles are removed. The tricuspid, mitral, and aortic valves are firmly attached to a dense fibrous tissue core called the central fibrous body (CFB). The mitral and aortic valves are in direct contact (asterisks) in the left ventricle. The tricuspid and pulmonary valves are separated by the intervening crista supraventricularis. The crista supraventricularis consists of the ventriculoinfundibular fold (VIF) and outlet septum (OS). The tricuspid valve (TV) consists of the septal (S), anterior (A), and posterior (P) leaflets. The mitral valve (MV) consists of the anterior (A) and posterior (P) leaflets. The aortic valve consists of the right coronary (RC), left coronary (LC), and noncoronary (NC) cusps. The pulmonary valve consists of the right (R), left (L), and anterior (A) cusps. The coronary sinus (CS) is seen along the posterior margin of the mitral valve. The right atrium is located rightward, anterior, and inferior to the left atrium (Fig. 1.7). The right atrium receives blood flow from the body through the superior and inferior venae cavae. The right atrium also receives blood flow from the myocardium through the coronary sinus and small direct coronary venous channels. The right atrium communicates with the right ventricle, which is anterior and leftward. The left atrium is a midline posterosuperior chamber in front of the vertebral column. Interposed between the left atrium and the vertebral column are the esophagus on the right and the descending aorta on the left. The carina of the trachea and the left main bronchus are located immediately above the left atrium. The left atrium receives the pulmonary veins, usually two from each lung. The left atrium communicates with the left ventricle, which is anterior and leftward. Each atrium consists of a smooth-walled main body and a trabeculated appendage or auricle. The main bodies of the right and left atria are opposed to each other centrally with the atrial septum in an oblique plane behind the ascending aortic root. The atrial appendages project laterally from the main bodies to embrace the arterial trunks from behind. The right atrial appendage is shaped like a blunt triangle and has a broad base at its junction with the main body of the right atrium. The left atrial appendage is a finger-like, crenellated tube and has a narrow orifice at its junction with the main body of the left atrium. In the right atrium, the superior and inferior venae cavae form a furrow-like confluence called the sinus venarum. Medially, the sinus venarum is bounded by the atrial septum with an indistinct demarcation. Laterally, the sinus venarum is bounded by the appendage. The C-shaped muscular ridge that demarcates the sinus venarum and appendage is the crista terminalis. Externally, this junction is demarcated by a shallow depression called the sulcus terminalis. In the left atrium, the pulmonary venous confluence does not form a furrow; therefore, there is neither a crista nor a sulcus terminalis. Fig. 1.7 Morphologic characteristics of the right and left atria. (A) The atria and arterial trunks are seen from below after the ventricles together with the atrioventricular and semilunar valves are removed (asterisks indicate crista terminalis). (B) The base of the heart is seen from above after removal of the cranial parts of the atria. Note that the pectinate muscles extend to the atrioventricular junction in the right atrium, but not in the left atrium. (C) Drawings showing the morphologic characteristics of the right and left atria. Ao, ascending aorta; RAA, right atrial appendage; MPA, main pulmonary artery; LA, left atrium; LAA, left atrial appendage; TV, tricuspid valve; MV, mitral valve; AV, aortic valve; PV, pulmonary valve; SVC, superior vena cava. ([A] Reproduced with permission of Professor Robert H. Anderson.) Superiorly, the crista terminalis extends to the atrial septum in front of the superior vena caval orifice (Fig. 1.8A). Inferiorly, the crista is transformed to a thin membranous flap that extends to the atrial septum in front of the inferior caval orifice. This membranous flap is the Eustachian valve of the inferior vena cava (Fig. 1.8B). The Eustachian valve varies in size and is often perforated. Infrequently, it reaches the superior vena caval orifice and appears as a septum with multiple perforations, which is called Chiari’s network. Immediately medial and posterior to the inferior vena caval orifice is the orifice of the coronary sinus. The coronary sinus is the terminal drainage root of most of the coronary venous blood and courses along the posterior aspect of the left atrioventricular groove to open into the right atrium immediately near the crux cordis (Fig. 1.6A). The coronary sinus orifice is either unguarded or partially concealed by a membranous flap, which is called the Thebesian valve (Fig. 1.8B). In contrast to the right atrium, the main body of the left atrium is smooth-walled without any recognizable muscular ridges or membranous valves. Usually two, infrequently one and rarely three, pulmonary veins from each lung are connected to each side of the posterior wall.4 Fig. 1.8 Anatomy of the atrial septum. (A) The atrial septum is seen from the right atrium. There is an oval depression called the fossa ovalis (FO) which is demarcated by a muscular limb (marked by “o’s”) called the limbus of the fossa ovalis. The superior vena cava (SVC) is demarcated anteriorly by the crista terminalis (asterisks). (B) The anterior wall of the right atrium is removed to show the Eustachian valve of the inferior vena cava (probed) and the Thebesian valve of the coronary sinus. The tendon of Todaro is the fibrous ridge extending from the commissure between these two valves to the atrioventricular membranous septum. The triangle of Koch is demarcated by the tendon of Todaro, coronary sinus opening, and the base of the septal leaflet of the tricuspid valve. The atrioventricular node is located in the triangle of Koch. (C) Drawings show how the foramen ovale conveys the oxygenated blood from the placenta to the left side of the heart and how the fossa ovalis is formed after birth. The tissue forming the fossa ovalis is the embryologic septum primum and the surrounding limbus is the embryologic septum secundum. SVC, superior vena cava; CS, coronary sinus; LA, left atrium; RA, right atrium. The internal walls of the atrial appendages are roughly trabeculated (Fig. 1.7). These trabeculations are called the pectinate muscles. The pectinate muscles of the right atrial appendage extend inferiorly to the posterior and lateral parts of the atrioventricular junction (Figs. 1.7B, 1.7C).5 In the left atrium, the pectinate muscles are confined to the tubular appendage and only rarely do a few tiny strands reach the atrioventricular junction. In other words, the right atrial appendageal orifice reaches the atrioventricular junction, whereas the orifice of the left atrial appendage is located at some distance from the atrioventricular junction. The atrial septum seen from the right atrium is rather complex (Fig. 1.8A). The atrial septum appears quite large when it is observed in an opened specimen. However, only a small part that appears to be interatrial is truly between the atrial chambers. The rest of the dividing wall between the atria is the infolding of tissue from the superior and posterior parietal wall of the atrium.6 The right atrial side of the atrial septum has a central depression with a surrounding muscular rim, called the fossa ovalis and limbus of the fossa ovalis, respectively. Anteroinferiorly, the limbus merges with the supratricuspid part of the septum in front of the coronary sinus orifice. The upper posterior region of the supratricuspid part of the septum is between the atria as is the floor of the fossa ovalis; the lower anterior region is between the right atrium and the left ventricle. This is because the tricuspid valve is attached to the septum more apically than the mitral valve. In the supratricuspid part of the septum, a fibrous fascicle arises from the commissure between the Eustachian and Thebesian valves and inserts into the central fibrous body (Fig. 1.8B). This is designated the tendon of Todaro,7 which is an important landmark forming the posterosuperior boundary of the triangle of Koch that contains the atrioventricular node (Fig. 1.8B). The other boundaries of the triangle of Koch are the attachment of the septal leaflet of the tricuspid valve and the orifice of the coronary sinus. The anterior apical part of the triangle is the membranous septum. The atrioventricular node is located immediately behind the membranous septum and gives rise to the atrioventricular conduction axis of His. Unlike the right atrial side, the left atrial side of the atrial septum is smooth. The only recognizable structure is a fibrous strand of tissue in its anterosuperior part. This strand represents the ventral edge of the floor of the fossa ovalis, which has fused to the limbus of the fossa ovalis after birth. The fossa ovalis is of vital importance during fetal life. In the fetus, it is a one-way valve or door-like structure with its hinge along the posteroinferior part of the limbus and its free edge against the door-frame of the limbus on the left side (Fig. 1.8C). Embryologically, the valve is the septum primum, and the limbus the septum secundum. The inferior vena caval blood flow hits the floor of the fossa ovalis and opens the valve, allowing the oxygenated blood from the placenta via the ductus venosus to pass into the left atrium, left ventricle, and aorta to perfuse the myocardium and brain. In contrast, the superior vena caval blood flows directly into the right ventricle through the tricuspid valve and then to the pulmonary arterial trunk, allowing the deoxygenated blood to reach the placenta through the ductus arteriosus, descending aorta, and umbilical arteries. The opening in the atrial septum in fetal life is called the foramen ovale. After birth, with breathing of air and establishment of the pulmonary circulation, the increased left atrial blood flow and pressure result in functional closure of the door of the foramen ovale against the limbus of the fossa ovalis. Subsequently, the foramen ovale closes completely by fibrous adhesions. Not infrequently, the fusion is incomplete, leaving the foramen ovale patent. A patent foramen ovale (PFO) is seen in over 25% of both autopsy and healthy adult studies.8,9 The presence of a PFO has no adverse consequence in otherwise healthy adults. However, a systemic venous thrombus can migrate into the systemic arterial circulation during a Valsalva maneuver. Patients who suffer a stroke or transient ischemic attack in the presence of a PFO and without any other cause are considered for prophylactic medical therapy and/or surgical or nonsurgical closure of the PFO to reduce the risk of a recurrent embolic event. Mostly, the right ventricle is located anterior and rightward of the left ventricle. The right ventricle is pyramidal in shape, and the left ventricle is a truncated ellipsoid (Fig. 1.9). In short axis planes, the left ventricle is circular, whereas the right ventricle is crescentic encircling the left ventricle (Figs. 1.4, 1.6B). The left ventricle is approximately three times thicker than the right ventricle. Fig. 1.9 Morphology and spatial relationship of the right and left ventricles. Volume rendered contrast-enhanced magnetic resonance angiograms are reconstructed as seen from front and the left side. The right ventricle (RV) is pyramidal; the left ventricle (LV) is elliptical. Note that the ventricular outflow tracts and arterial trunks spiral around each other. Ao, Ascending aorta; MPA, main pulmonary artery. Fig. 1.10 (A) Interior of the right and left ventricles. Note the difference in trabeculation patterns of the ventricles. The trabecular septomarginalis (TSM) is the most-stout trabeculation on the septum. The pulmonary and tricuspid valves are separated by an intervening muscular crest that is called the crista supraventricularis (CSV). The aortic and mitral valves are in direct contact (asterisks). The mitral valve is supported by two stout papillary muscles called the anterolateral and posteromedial papillary muscles (ALPM and PMPM, respectively). The tricuspid valve (TV) consists of the septal (S), anterior (A) and posterior (P) leaflets. They are supported by the medial, anterior, and posterior papillary muscles (MPM, APM, and PPM, respectively). The membranous part (m) of the ventricular septum is transilluminated from the right side. The atrioventricular (AV) septum is present because of the offset attachment of the mitral valve (MV) and tricuspid valve leaflets to the septum. The ventricular septum is arbitrarily divided into the inlet, apical, trabecular, and outlet parts. (B) Rendered drawing of interior of the right and left ventricles. Ao, ascending aorta; MPA, main pulmonary artery; AV, atrioventricular. Each ventricle consists of three anatomic and functional units: the inlet, apical trabecular, and outlet components (Fig. 1.10
 General Consideration
General Consideration
 Base of the Ventricles
Base of the Ventricles


 Atria
Atria
 Ventricles
Ventricles

![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree