6
Normal Variants and
Benign Findings
Eugene C. Lin and Abass Alavi
As a rule, most inflammatory or infectious processes are visualized by positron emission tomography (PET) because activated white cells have increased glycolysis. Thus, it is not possible to exhaustively list all potential non-neoplastic causes of fluorodeoxyglucose (FDG) uptake. Correlation with clinical data and other imaging studies should alert the interpreter in many cases to potential false-positive findings in such settings. The discussion in this chapter will focus on the range of normal sites of FDG uptake and the common noninfectious/inflammatory causes of increased uptake. Artifacts specific to PET/computed tomography (CT) will be discussed in Chapter 8.
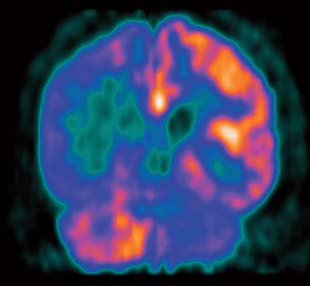
It is important that physicians who interpret PET brain scans review a large number of normal images before interpreting studies in patients with neuropsychiatric disorders.1
- Normal pattern of uptake
- The normal brain has high FDG uptake in the gray matter, with a gray to white matter activity ratio from 2.5 to 4:1.
- The basal ganglia usually has slightly more uptake than the cortex.
- Mild focal areas of increased activity2 can be seen normally in the
- Frontal eye fields
- Posterior cingulate cortex
- Wernicke region (posterosuperior temporal lobe)
- Visual cortex (see Chapter 29)
- Age-related changes. Cortical metabolism decreases with age, particularly in the frontal lobes. In contrast, metabolic activity of the basal ganglia, visual cortices, and cerebellum remain unchanged.
- Renal function. Patients with renal failure have decreased FDG uptake in the cortex and white matter compared with those with normal renal function.3
- Symmetry of uptake. There are often minimal asymmetries in uptake between areas in the left and right hemispheres. Asymmetric uptake should be interpreted with caution unless
- There is a significant difference between the two sides that correlates with clinical findings. For example, any level of asymmetry in the temporal lobes in a patient with epilepsy should be considered a potential focus for seizure activity. Quantitatively, a difference of 10 to 15% is often considered significant, but clinical correlation is paramount.
- The asymmetry is fairly extensive and seen on multiple slices.
- Comparison with single-photon emission computed tomography (SPECT)
- FDG uptake usually correlates with uptake of SPECT perfusion tracers, except in cases where metabolism and perfusion are uncoupled (e.g., luxury perfusion postinfarct).
- The magnitude of hypometabolism seen on PET is usually greater than that of hypoperfusion seen on SPECT.
- Cerebellar uptake of FDG is variable but in general is less than that seen on SPECT. This differs from brain SPECT images, where consistently the cerebellum appears more active than other brain structures.
- Crossed cerebellar diaschisis. The glucose metabolism in the cerebellar hemisphere contralateral to a supratentorial abnormality (tumor, infarct, or trauma) is frequently decreased (Fig. 6.1) in the acute phase of the disease and may change over time. This does not indicate cerebellar pathology.
- Diaschisis is thought to be related to interruption of the corticopontocerebellar pathway.
- Ipsilateral pontine hypometabolism and preservation of metabolism in the contralateral dentate nucleus have been reported.4
Spinal cord uptake is variable. Mild spinal cord uptake is normal.
- Ventricular uptake
- Fasting state. For noncardiac PET studies done during fasting, myocardial metabolism shifts from utilizing glucose to utilizing fatty acids. Therefore, in theory myocardial uptake on fasting PET studies should be minimal. However, in many cases there will be substantial myocardial FDG uptake on fasting PET studies.
- Outpatients, men, younger patients, patients with heart failure, and patients receiving benzodiazepines tend to have more myocardial uptake.5,6 Diabetic patients and patients receiving bezafibrate or levothyroxine tend to have less myocardial uptake.5,7
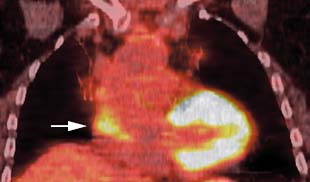
- An irregular pattern of ventricular uptake is not uncommon. Focal areas of increased and decreased uptake should not be considered sites of disease in the absence of a supporting cardiac history.
- The myocardial uptake pattern demonstrates a large spatial and temporal variability, and a patient without cardiac disease can demonstrate substantially different patterns of myo-cardial FDG uptake on serial studies (Fig. 6.2).8
- Decreased septal activity has been noted as a common caption variant in fasting patients (Fig. 6.3). However, left bundle branch block can also cause decreased septal uptake.9
- Insulin effect. Increased myocardial activity is seen after insulin administration or insulin release secondary to a recent meal (myocardial glucose receptors are insulin sensitive). This is seen in conjunction with intense skeletal muscle uptake (as seen in Fig. 4.1, p. 34).
- Right ventricular uptake. There is greater uptake in the left ventricle than the right ventricle. Typically, right ventricular uptake is minimal unless there is hypertrophy.
- Papillary muscle uptake. Papillary muscle uptake is often seen in conjunction with uptake in the left ventricular wall. Occasionally, papillary muscle uptake can be seen in isolation (Fig. 6.4).10 In these cases, the uptake could mimic an intraventricular neoplasm or thrombus. Note that there are no septal left ventricular papillary muscles, and left ventricular uptake arising from the septum cannot represent papillary muscle (Fig. 6.4).
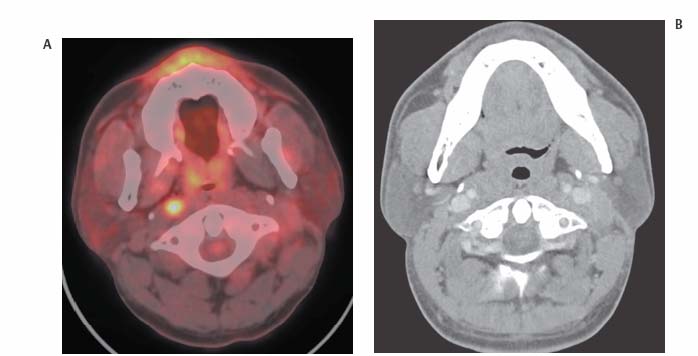
- Atrial uptake
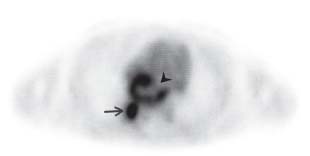
- Atrial uptake can be irregular and focal. Focal atrial FDG uptake can mimic a mediastinal node (Fig. 6.5). This is particularly true on axial images in the subcarinal region. Therefore, correlation with sagittal and coronal PET images and CT is necessary before diagnosing subcarinal nodal uptake on axial images.
- Ringlike atrial uptake can mimic a large necrotic subcarinal node (Fig. 6.6). This is easily differentiated by correlation with all imaging planes and CT.
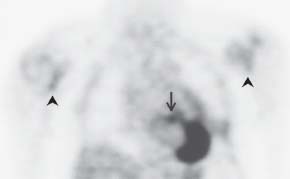
- Increased right and left atrial uptake is associated with atrial fibrillation.11–13 Right atrial uptake (Fig. 6.7) is usually more prominent.12
- Perfusion imaging. If perfusion imaging is performed with nitrogen 13 ammonia, lateral wall activity is normally decreased compared with the septum.14 This is of unknown etiology.
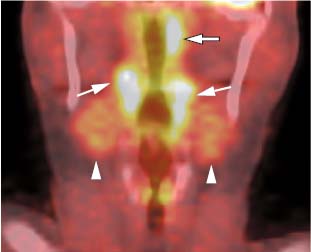
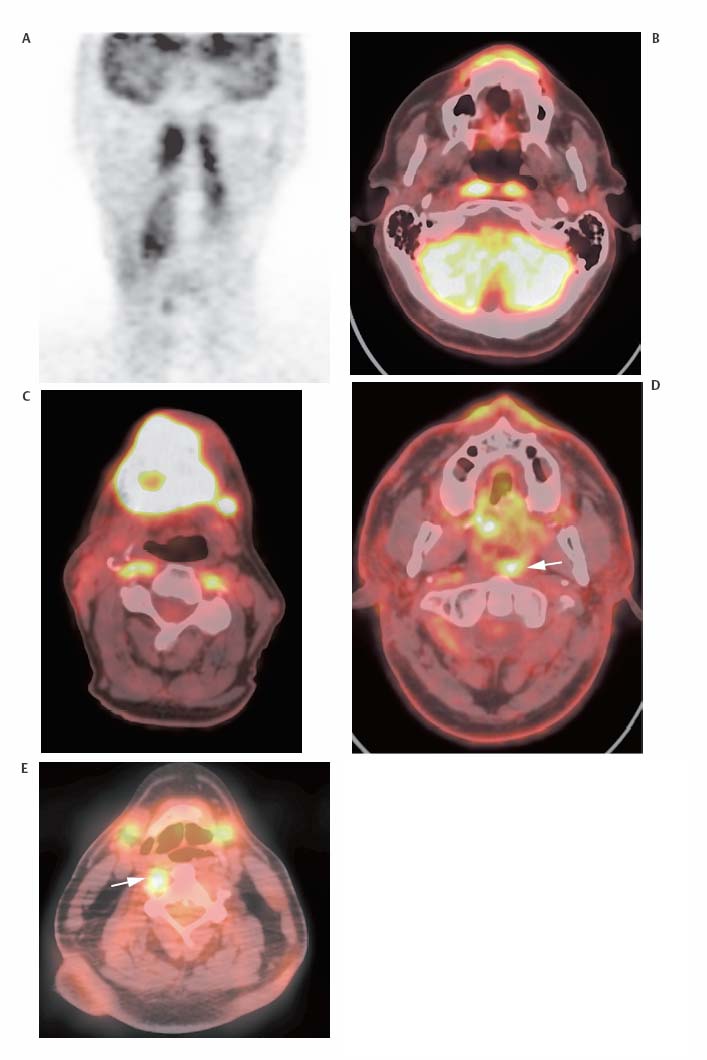
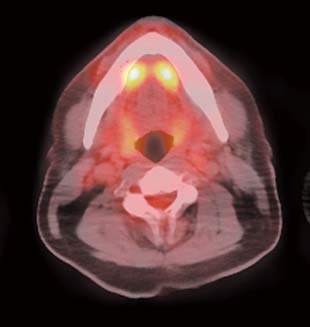
- Normal uptake (sagittal). On sagittal images, there is normally an inverted C shape composed of the mylohyoid muscles and sublingual glands, soft palate, and tonsils (Fig. 6.8). These are the most common areas of normal uptake.
- Mylohyoid muscles and sublingual glands (axial). On axial images, uptake in the mylohyoid muscles and/or sublingual glands can form an inverted V medial to the mandible. Due to their proximity, it is difficult to distinguish whether uptake is in the sublingual glands, mylohyoid muscles, or both. Sublingual uptake is more superior and focal (Fig. 6.9), whereas mylohyoid uptake is more inferior and linear (see Fig. 8.6, p. 92).
- Soft palate (axial). The soft palate can appear as a prominent focus of activity on axial images (Fig. 6.10).
- Soft palate uptake is more prominent in males.15
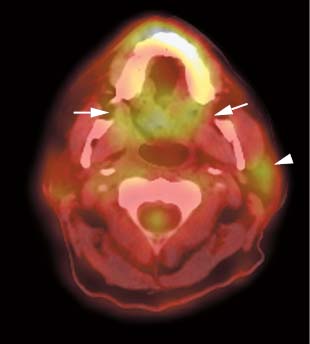
- Tonsils (coronal). Normal uptake in the palatine and lingual tonsils (Figs. 6.8 and 6.11) forms two vertical linear bands of uptake on coronal images. This may be prominent in cold/temperate climates and is also prominent in children.
- There is less uptake with increasing age in the palatine tonsils.15
- Salivary glands. Salivary gland uptake is more variable than tonsillar uptake.15 Salivary gland uptake if seen is usually less than tonsillar uptake (Fig. 6.11).
- There is less uptake with increasing age in the sublingual glands.15
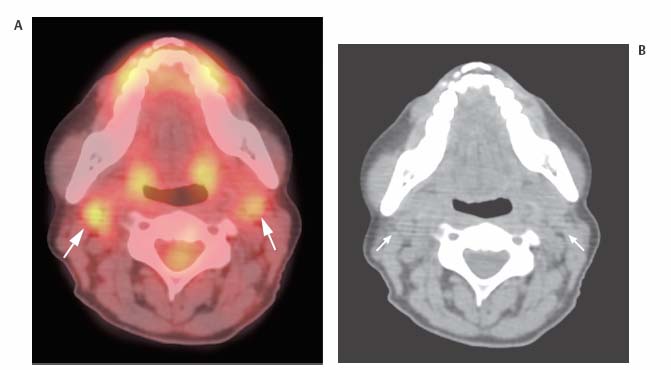
- The submandibular glands are in close proximity to submandibular nodes, and submandibular nodal uptake can be difficult to distinguish from normal glandular uptake even with PET/CT (Fig. 6.12).
- Nasopharyngeal uptake. Nasopharyngeal uptake is some times seen as a normal variant (Fig. 6.8), although larger degrees of uptake could be secondary to inflammation or tumor. Uptake in the lateral pharyngeal recess can be symmetric or asymmetric.
- Asymmetric uptake. Asymmetric uptake in the lateral pharyngeal recess (Fig. 6.11), cervical nodal uptake, and asymmetric wall thickening in the lateral pharyngeal recess on CT are associated with nasopharyngeal carcinoma.16
- However, in patient populations where nasopharyngeal carcinoma is less frequent, asymmetric uptake in the lateral pharyngeal recesses is often inflammatory.
- An SUV cutoff of > 3.9 and a lateral pharyngeal recess to palatine tonsil uptake ratio of > 1.5 are helpful in differentiating benign from malignant lateral pharyngeal recess uptake.16
- However, in patient populations where nasopharyngeal carcinoma is less frequent, asymmetric uptake in the lateral pharyngeal recesses is often inflammatory.
- Tongue. Tongue uptake can occasionally be seen, particularly if the patient speaks after FDG injection. In children, adenoid tissues are commonly visualized at the base of the tongue.
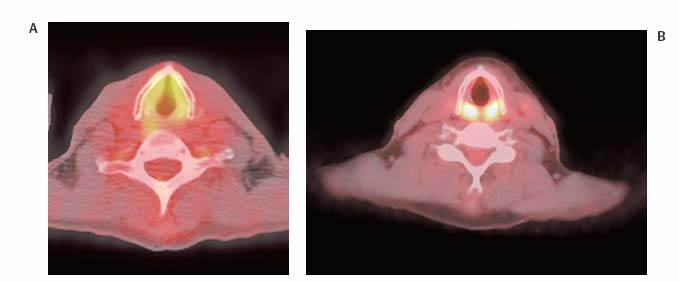
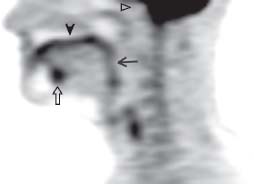
- Laryngeal uptake. Laryngeal muscle uptake is a normal variant and is pronounced if the patient speaks soon after FDG administration. It can have a horseshoe-like appearance with uptake in both the vocal cords and cricoarytenoid muscles or appear as two foci of posterior uptake in the cricoarytenoid muscles (Fig. 6.13). Normal activity is most pronounced posteriorly.
- It is better to use asymmetry of uptake rather than absolute uptake in the larynx as a criterion of abnormality.
- However, laryngeal uptake may be asymmetric secondary to postoperative changes or vocal cord paralysis (Fig. 6.14).
- Anterior uptake is more concerning than posterior uptake.
- Muscle uptake. Muscular uptake is common, particularly in the sternocleidomastoids. Less commonly, uptake is seen in the longus colli muscles. This can be asymmetric and potentially mimic neoplasm (Fig. 6.15).17 However, before attributing uptake to asymmetric longus colli activity, retropharyngeal adenopathy (Fig. 6.16) should be excluded, as it can have a similar appearance on axial images.
- Diffuse uptake. Mild diffuse thyroid uptake can be a normal variant. Greater degrees of diffuse uptake are seen in Graves disease and chronic thyroiditis (Fig. 6.17).18,19 In particular, diffuse thyroid uptake is often associated with chronic lymphocytic (Hashimoto) thyroiditis. This is not affected by thyroid hormone therapy. The SUV does not correlate with the degree of hypothyroidism.20
- SUV. The normal thyroid has a mean SUV of 1.5 ± 0.2.21
- Graves disease. Increased thyroid uptake in Graves disease is relatively uncommon; increased skeletal muscle and thymus activity is actually more commonly seen in this disorder.22
- Focal uptake. Focal uptake is nonspecific and can be seen in both benign and malignant nodules (see Chapter 14).
- Thyroid nodule mimics. Correlation with anatomic imaging is necessary before diagnosing peripheral thyroid nodules on PET.
- Lymph node. A medial lymph node adjacent to the thyroid can mimic a thyroid nodule (see Chapter 14).
- Parathyroid abnormality. Both parathyroid adenomas and hyperplasia can cause focal increased uptake mimicking a thyroid nodule. The normal parathyroids are not visualized on FDG PET.
- Glenohumeral joint. Glenohumeral joint activity can mimic axillary adenopathy on axial and coronal images (Fig. 6.18). It can be distinguished by its linear appearance and location immediately medial to the humeral head. This finding may not always be a normal variant, as it is often associated with joint pain.
- Dose extravasation. Extravasation at the injection site can cause ipsilateral axillary node uptake due to particle formation and phagocytosis at the draining lymph nodes.
- Premenopausal. Diffuse low-grade uptake is seen in glandular breast tissue in premenopausal women (Fig. 6.19). The SUV in dense breasts is higher than in nondense breasts; however, the uptake in dense breasts is still very low (SUV around 1).23
- Postmenopausal. Postmenopausal women on hormone replacement therapy may also have glandular uptake. The breast uptake should be less than the liver in postmenopausal women who are not on hormonal therapy.24
- Lactation. Prominent diffuse uptake is seen during lactation.
- Nipple. Nipple uptake is commonly seen.
- Breast implants. Mildly increased uptake can be seen around breast implants, which appear as negative defects.
- Focal uptake. Focal uptake is seen due to a wide range of benign conditions but commonly represents malignancy (see Chapter 16).
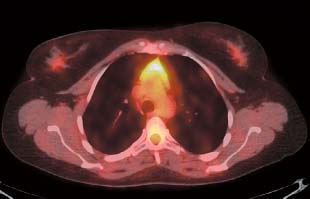
- Children. Thymus uptake is a normal variant in children.
- Adults. In adults, thymic uptake (Figs. 6.19 and 6.20) can be seen with thymic hyperplasia or if a substantial amount of normal thymic tissue remains after adolescence. The thymus can be distinguished from anterior mediastinal adenopathy by its characteristic inverted V shape. In addition, photopenic clefts are often seen extending through the thymic tissue.
- Age. Although thymic uptake is usually seen in young adults, it has been reported in patients up to 54 years old.25
- Clinical scenarios. Thymic uptake is occasionally seen soon after chemotherapy and is common following radioiodine treatment for thyroid cancer.
- Malignancy. If the uptake is focal, intense (greater than cerebellum or bladder or high SUV), or if the thymic shape is distorted, the possibility of malignancy should be considered.
- SUV26
- The average SUV in thymic hyperplasia is 1.9.27 However, SUV measurements as high as 3.8 have been reported in thymic hyperplasia.
- Thymomas typically have higher SUVs than thymic hyperplasia.27 However, the SUVs seen in thymic hyperplasia may overlap with those in thymoma.
- Invasive thymomas do not have higher SUVs than noninvasive thymomas.
- Thymic carcinoma usually has higher SUVs than thymoma.
- SUV cutoffs to differentiate thymic carcinoma from thymoma are variable ranging from 5 to 10.28
- Uptake in thymic carcinomas tends to be homogeneous, whereas uptake in thymomas is often heterogeneous.28
- Graves disease. Increased thymus uptake is common in Graves disease. A clue to the diagnosis is seeing increased skeletal muscle uptake and thyroid uptake (less likely) in conjunction with the thymic uptake.22
- Superior mediastinal activity. A normal variant can be seen secondary to superior extension of the thymus.29 In these cases there is a soft tissue nodule anteromedial to the left brachiocephalic vein, which can have increased FDG uptake, particularly in children and young adults who have thymic hyperplasia after chemotherapy. Although this nodule may not be connected to the thymus, it should have a similar SUV.
- Normal gradient of uptake. The lungs typically have minimal or no activity on attenuation-corrected images. Lung activity increases from the anterior to the posterior and from the superior to the inferior segments, particularly if the lungs are not fully inflated. This is more prominently seen on nonattenuation-corrected images.
- Increased uptake. A wide range of infectious/inflammatory processes can cause diffuse or focal increased uptake. Some rare causes of uptake are
- Diffuse uptake. Drug toxicity in cancer patients, radiation pneumonitis, acute respiratory distress syndrome30
- A neoplastic etiology of diffuse uptake is lymphangitic carcinomatosis (Fig. 6.21).31
- Nodular uptake.32–34 Bronchiolitis obliterans organizing pneumonia, lung infarction, amyloidosis
- Focal uptake without a CT correlate. There should almost always be a correlative finding on CT for focal FDG uptake in the lung. If substantial motion artifact is present, small lung nodules may not be identified. If no correlative finding is identified on a CT without motion, a small focus of focal FDG uptake could represent a clot injected during FDG administration (Fig. 6.22).
- Radiation pneumonitis. Radiation pneumonitis can cause very intense uptake before radiographic changes are seen. This should be suspected in the proper clinical setting if the uptake has a linear margin (Fig. 6.23). However, the lung is a relatively slow-reacting tissue to radiation, and radiation-induced elevation in FDG uptake typically does not occur until months after completion of radiotherapy.35 Uptake (usually pleural) in the contralateral shielded nonirradiated lung is common after radiation.36
- Atelectasis. Severely atelectatic lung can have increased activity (Fig. 6.24). However, PET is helpful in cases of postobstructive atelectasis, as the central obstructing tumor will have more uptake than the distal atelectasis (Fig. 6.25).
- False–positive results. Very rare causes of false-positive results are hamartoma, round atelectasis, and pleural fibrosis. In the majority of cases, these entities do not have significant uptake.37
- Mild bilateral hilar nodal uptake is very common (Fig. 6.26). This appearance is almost never associated with malignancy.
- Uptake in a central pulmonary embolus could mimic hilar adenopathy.
- Patterns of esophageal uptake (Fig. 6.27)
- Mild diffuse esophageal uptake is often a normal variant.
 General Principles
General Principles Brain
Brain Spinal Cord
Spinal Cord Heart
Heart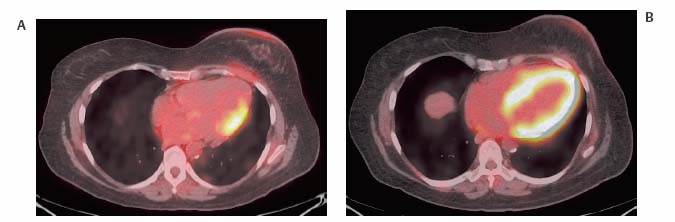

 Head and Neck
Head and Neck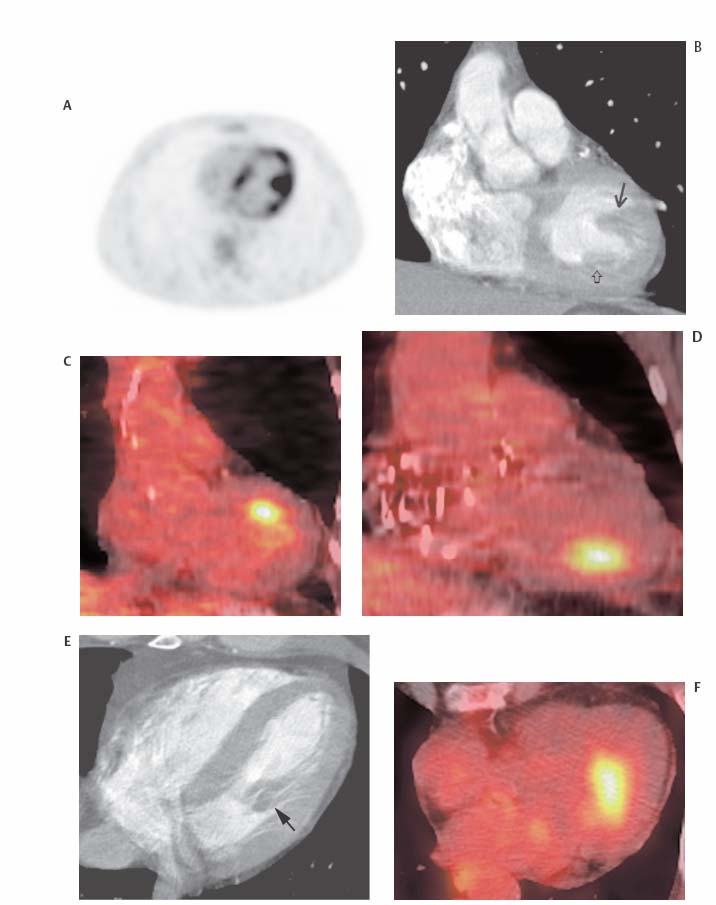

 Thyroid
Thyroid
 Axilla
Axilla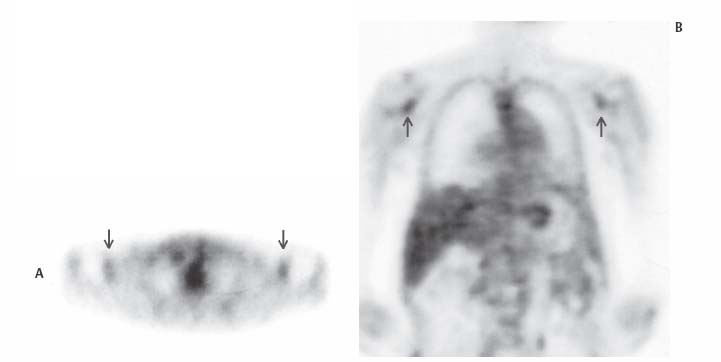
 Breast
Breast
 Thymus
Thymus Hila
Hila Esophagus
Esophagus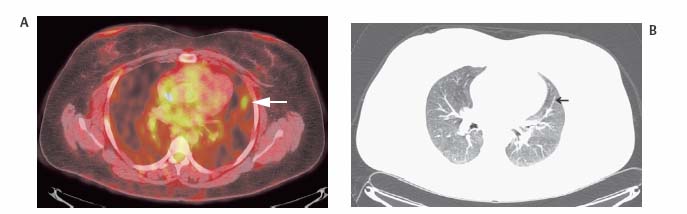
![]()