- •
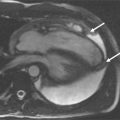
Optimal visualization of normal vascular anatomy with magnetic resonance angiography can be achieved with gadolinium-enhanced three-dimensional (3D) techniques, phased array surface coils, and parallel imaging.
- •
Three-dimensional reconstruction techniques are typically used and consist of multiplanar reformatted images and full or subvolume maximum intensity projection images in various planes.
This chapter reviews the normal arterial and venous anatomy as well as some of the more common normal variants for the extracranial circulation in the form of an anatomic atlas. All images were obtained on state-of-the-art 1.5T and 3T whole-body scanners. Gadolinium-enhanced 3D techniques were used for all cases using phased array surface coils and parallel imaging. To optimally visualize the individual vascular territories, the most appropriate 3D reconstruction techniques were used. These consist of multiplanar reformatted images and full or subvolume maximum intensity projection images in various planes, in addition to source images.















Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree