Chapter 16 Nuclear medicine
 The radiation dose from any diagnostic procedure should be as low as reasonably practicable, consistent with diagnostic results.1
The radiation dose from any diagnostic procedure should be as low as reasonably practicable, consistent with diagnostic results.1 This is governed in nuclear medicine by the administration of strictly controlled amounts of radioactivity under a licensing arrangement and the use of optimum imaging conditions.2
This is governed in nuclear medicine by the administration of strictly controlled amounts of radioactivity under a licensing arrangement and the use of optimum imaging conditions.2 Any person working within the nuclear medicine environment should have an awareness of the practical radiation protection considerations.
Any person working within the nuclear medicine environment should have an awareness of the practical radiation protection considerations. Nuclear medicine studies require the administration of less than a microgram of the radioactive substance under test. This has the advantage that it does not interfere with the physiological pathways but demonstrates their function.
Nuclear medicine studies require the administration of less than a microgram of the radioactive substance under test. This has the advantage that it does not interfere with the physiological pathways but demonstrates their function. The radioactive substances may be given in one of two forms: in their radionuclide form or attached to a drug and known as a radiopharmaceutical.
The radioactive substances may be given in one of two forms: in their radionuclide form or attached to a drug and known as a radiopharmaceutical. The radiopharmaceutical or radionuclide determines which system or organ the radioactive substance targets.
The radiopharmaceutical or radionuclide determines which system or organ the radioactive substance targets. Most radioactive substances used in diagnostic imaging emit gamma radiation, which can subsequently be detected externally to the patient, and an image is produced of the uptake in the specific area.
Most radioactive substances used in diagnostic imaging emit gamma radiation, which can subsequently be detected externally to the patient, and an image is produced of the uptake in the specific area. Nuclear medicine studies can often detect certain disorders earlier than other diagnostic imaging procedures because they rely on functional rather than structural changes.
Nuclear medicine studies can often detect certain disorders earlier than other diagnostic imaging procedures because they rely on functional rather than structural changes.INTRODUCTION
Nuclear medicine is concerned with providing diagnostic information about patients following the administration of a radioactive product. The patient is imaged using a gamma camera. Images are produced of the distribution of the radioactive substance within different organs and systems. This can be compared with normal distribution to diagnose if a medical condition is present and assess its extent or severity.
Key terms
RADIONUCLIDES USED IN MEDICAL IMAGING
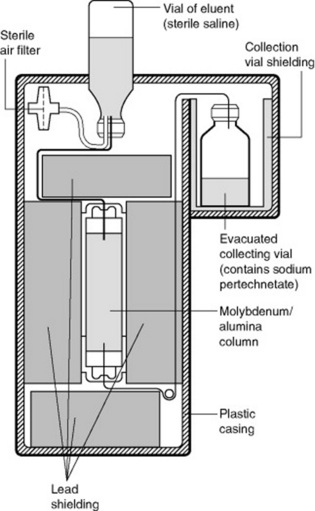
TECHNETIUM
OTHER RADIONUCLIDES USED IN DIAGNOSTIC IMAGING
81mKrypton
Krypton is used for scanning the lungs as it can show the ventilation. It is metastable like technetium and also a pure gamma emitter. It has an energy level of 190 keV, but has a half-life of 13 seconds. This means that the radionuclide has to be produced and then administered directly to the patient. In this case the patient inhales the radionuclide. Air is passed over a column of rubidium, which results in krypton being produced.
EQUIPMENT
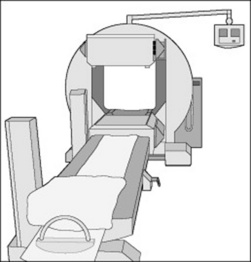
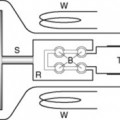
The basic design of a gamma camera has not significantly changed for over 40 years and the use of devices such as sodium iodine crystals and photomultiplier tubes are the main reasons why nuclear medicine images have such low resolution in comparison to CT. However, technology advancements may see the development and production of solid-state gamma cameras in the future. The modern gamma camera consists of a large detector (or two detectors in dual head systems, Fig. 16.4), which is positioned as close to the patient as possible during examinations.
Many nuclear medicine departments will utilise one gamma camera to undertake a range of examinations. Some larger departments may employ a dual and a single head gamma camera to perform clinical examinations. Dual head gamma camera systems allow the operator to perform certain examinations (e.g. whole body bone scans) quicker than single head units, which is particularly useful for patients who may be in considerable discomfort.
The basic components of a modern gamma camera detector unit are: