Fig. 31.1
[18F]FDG PET coronal images demonstrate multiple hypermetabolic lymph nodes on both sides of the diaphragm
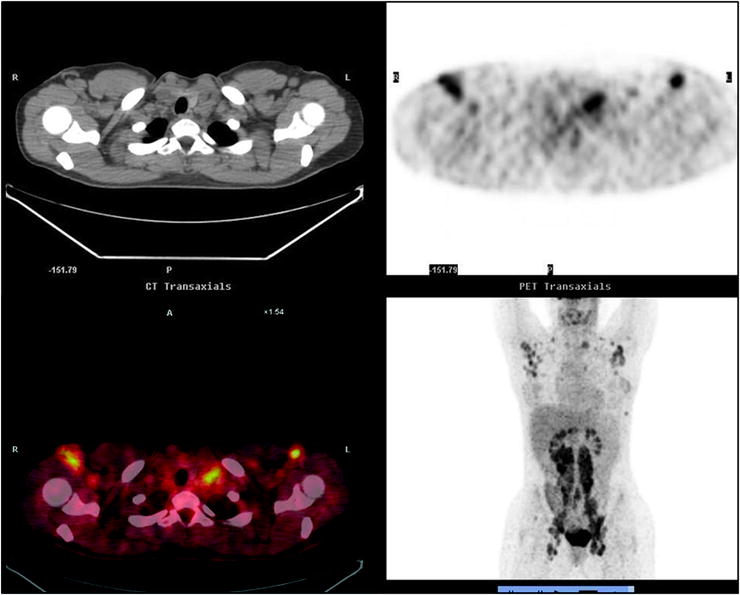
Fig. 31.2
Axial CT (left upper), [18F]FDG axial (upper right), fused [18F]FDG PET/CT (lower left), and MIP (lower right) images show [18F]FDG-avid lymph nodes in retroclavicular and axillary regions
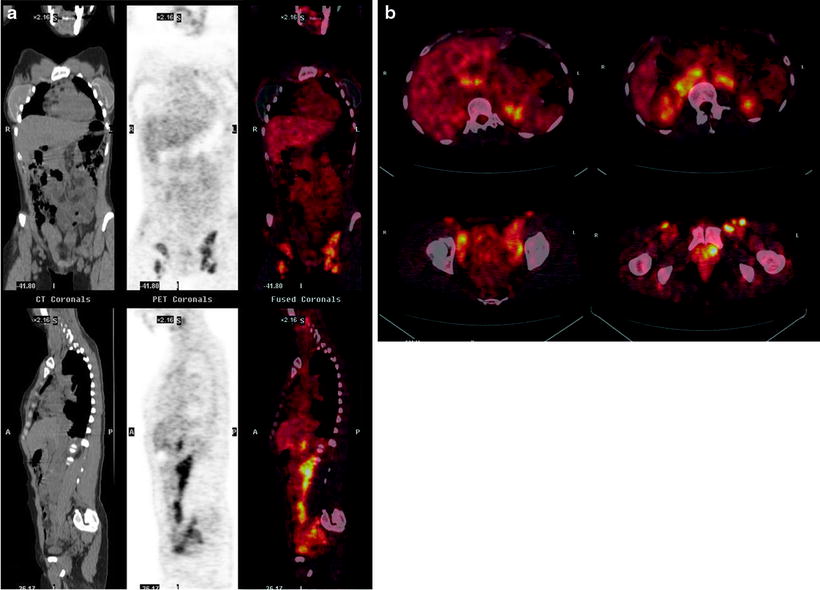
Fig. 31.3
[18F]FDG PET/CT images show multiple hypermetabolic lymphadenopathies. (a) [18F]FDG PET/CT coronal images of inguinal [18F]FDG-avid adenopathies (CT image in left panel, [18F]FDG PET image in central panel and [18F]FDG PET/CT fused image in right panel). (b) [18F]FDG PET/CT transaxial fused images of abdominal and pelvic [18F]FDG-avid nodes. (c) [18F]FDG PET/CT sagittal image of abdominal and pelvis lymphadenopathies (CT image in left panel, [18F]FDG PET image in central panel, and [18F]FDG PET/CT fused image in right panel)
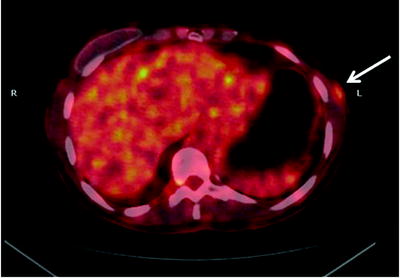
Fig. 31.4
[18F]FDG PET/CT fused transaxial image shows [18F]FDG-avid subcutaneous nodule of left lateral chest wall
Follow-Up
Following chemotherapy, [18F]FDG PET/CT was repeated to evaluate response to treatment. No sites of abnormal [18F]FDG uptake are seen, demonstrating complete response to therapy (Fig. 31.5). End of treatment [18F]FDG PET/CT should be performed at least 6–8 weeks after treatment—to minimize false-positive and false-negative results. To assess the effectiveness of therapy between cycles of treatment, patients should be studied immediately prior to the next cycle of treatment.
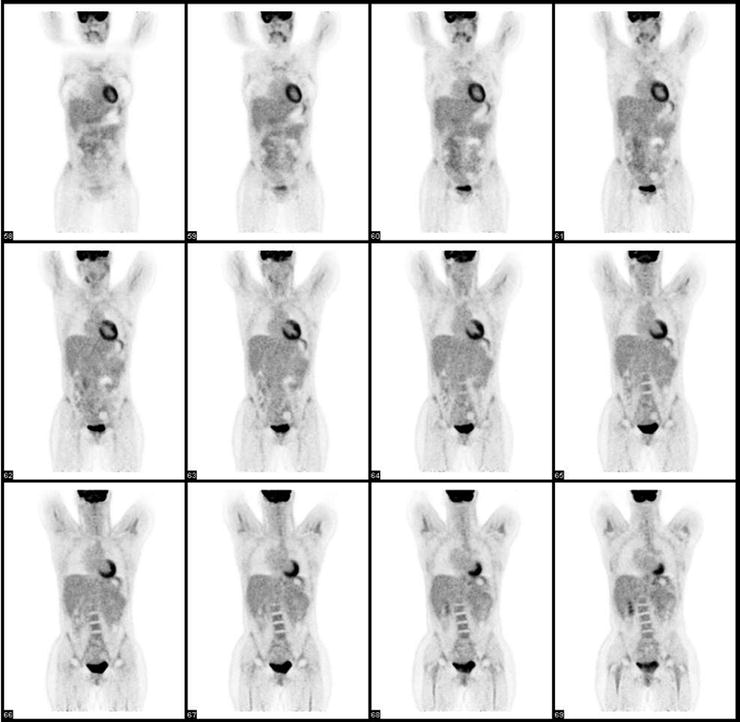
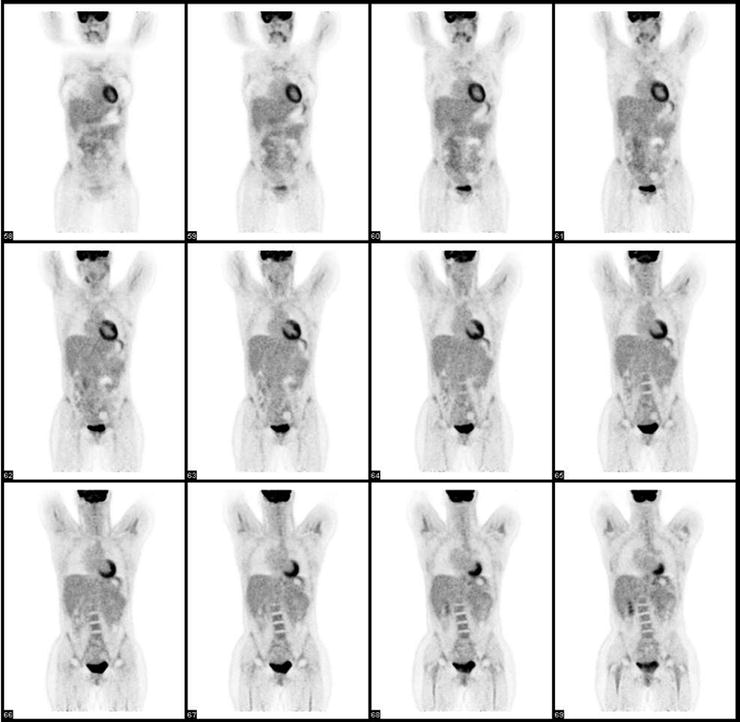
Fig. 31.5
[18F]FDG PET coronal images for treatment evaluation show the disappearance of radiopharmaceutical uptake after chemotherapy
Case 2: Multiple Myeloma
Presentation
A 62-year-old man presented with intermittent back pain that became more severe over 2 months.
Findings
CT revealed a lytic lesion in L5 (with extension into the epidural space on MRI) and a lesion in the right ilium. Biopsy of the ilium showed atypical large lymphoid/plasmacytoid cells. An [18F]FDG PET/CT was performed to evaluate the extent of disease. The known right iliac lesion with soft tissue component measuring 5 × 5 cm is [18F]FDG avid (SUVmax 26) (Fig. 31.6). The L5 lesion presents lytic component on the left side and a soft tissue component that involves the left foramina (SUVmax 6.9) (Fig. 31.7). Other hypermetabolic bone lesions are seen in the proximal sternum (SUVmax 9), ribs bilaterally, T7 involving the adjacent pleura, T9 and L4 (Fig. 31.8).
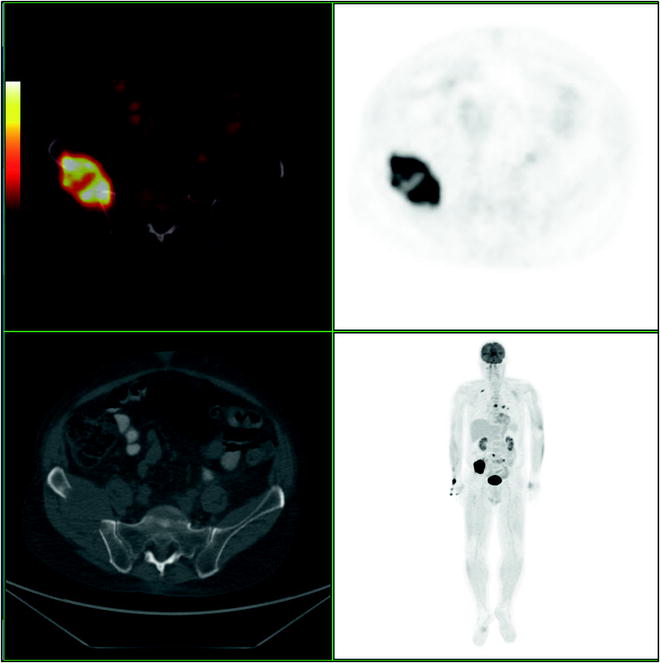
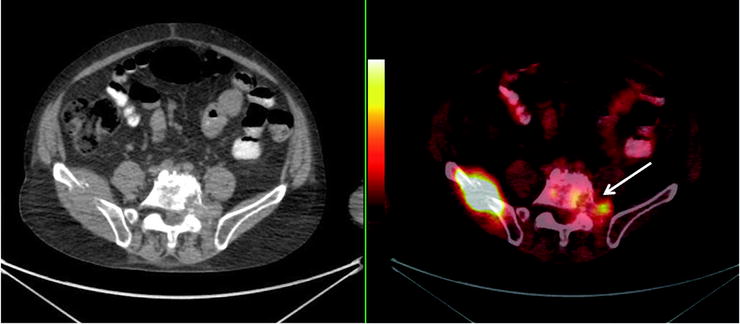
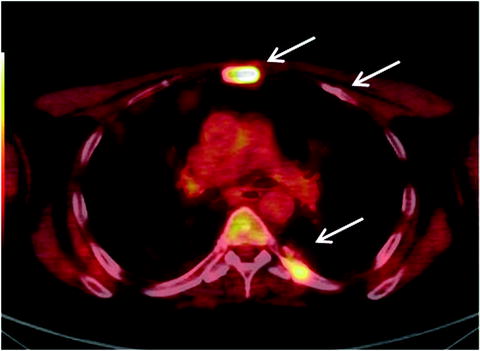
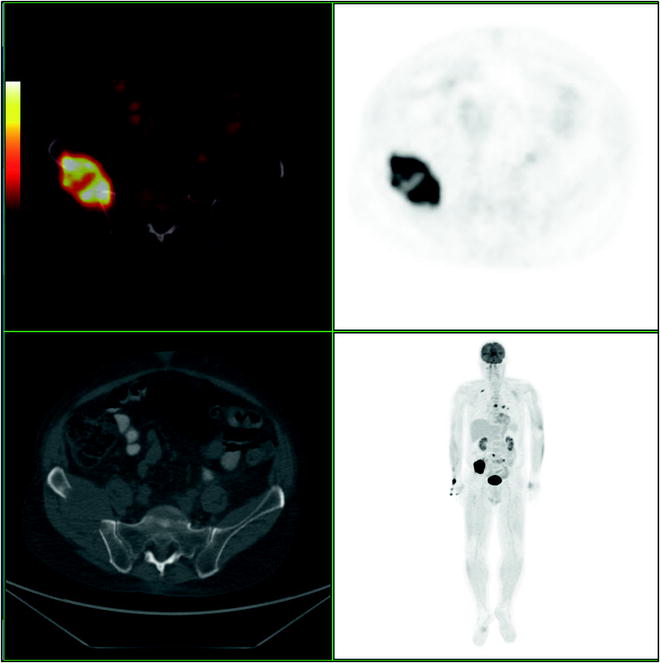
Fig. 31.6
[18F]FDG PET/CT axial fused (left upper), PET axial (right upper), and CT axial (left lower) images show a hypermetabolic lesion corresponding to the lytic right iliac mass. MIP image (right lower) shows additional lesions that are better characterized in the following illustrations
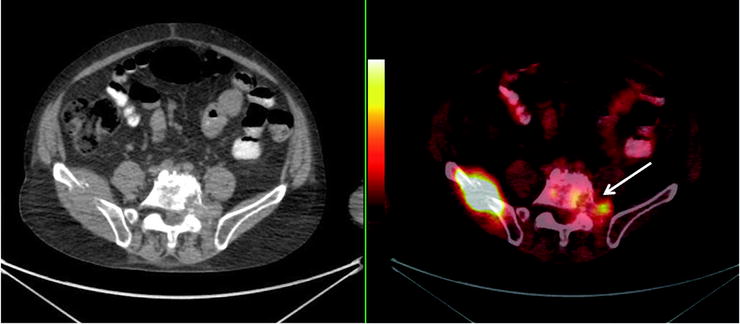
Fig. 31.7
[18F]FDG PET/CT transaxial images (CT, left panel; PET/CT fused image, right panel) demonstrate [18F]FDG-avid L5 lesion with the involvement of the left foramina (white arrow)
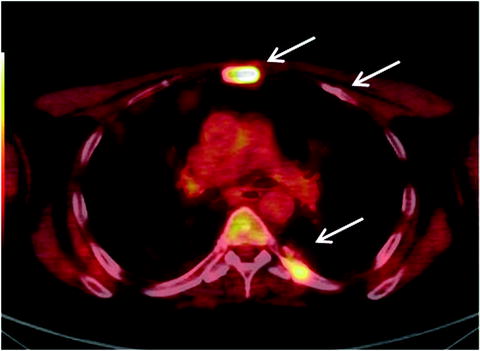
Fig. 31.8
Fused [18F]FDG PET/CT transaxial image shows hypermetabolic skeletal lesions in sternum, rib, and vertebra (arrows)
[18F]FDG PET/CT is more sensitive than skeletal X-ray evaluation of bone marrow involvement in patients with multiple myeloma. The technique may be able to predict fracture risk, particularly if the SUVmax is >3.4.
Case 3: Brain Lymphoma
Presentation
A 72-year-old woman with multifocal ductal carcinoma of the left breast previously treated with lumpectomy, external beam radiation therapy, and chemotherapy 5 years ago. She developed weakness of the right hand.
Findings
MRI of the brain revealed multiple supratentorial metastases several of which demonstrated lesional hemorrhage and edema. An extra-axial lesion involving the left cavernous sinus and the middle cranial fossa was also seen, representing a meningioma. [18F]FDG PET/CT was performed to evaluate the extent of disease (Figs. 31.9 and 31.10). PET/CT fusion images demonstrate five hypermetabolic lesions of the brain with intense [18F]FDG uptake localized, respectively, in the high left parietal lobe (1.7 × 1.7 cm, SUVmax 17), left temporo-occipital region (1.2 × 1.5 cm, SUVmax 15), right frontal cortex (1.3 × 1.3 cm, SUVmax 16), and right parietal cortex (1.6 × 1 cm, SUVmax 16) (Fig. 31.10). These supratentorial lesions are suspicious for metastases. A large lobulated lesion (Fig. 31.11) in the left frontal and temporal lobe with a rim of calcification in contact to the sphenoid bone (SUVmax 22) is also seen, suggesting a meningioma, in correlation with MRI. [18F]FDG PET/CT did not show evidence of recurrent or metastatic disease outside the brain. The patient underwent left temporal superficial brain biopsy and tumor resection which revealed diffuse large cell lymphoma with adjacent meningioma grade 1. The lumbar puncture and bone marrow biopsy were negative for the presence of malignant cells. The patient was treated with combination chemotherapy.
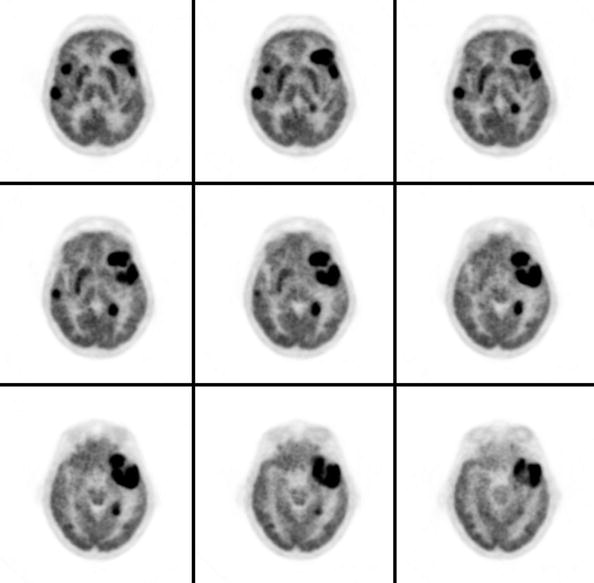
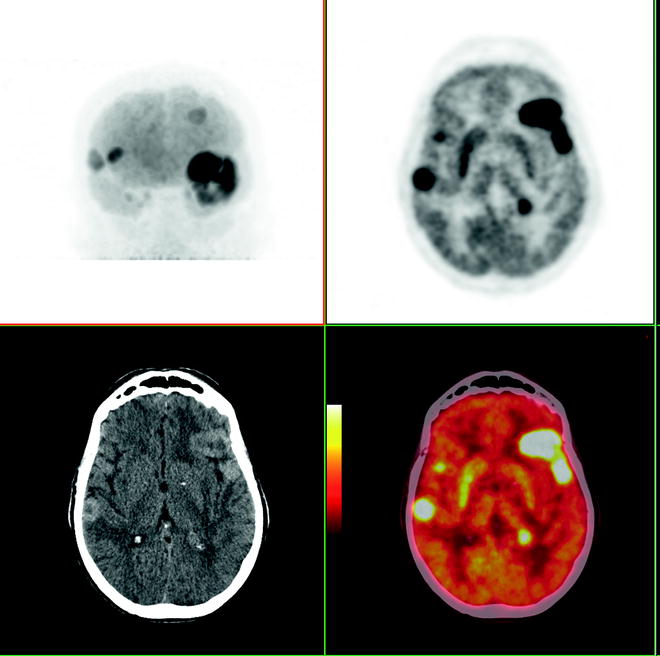
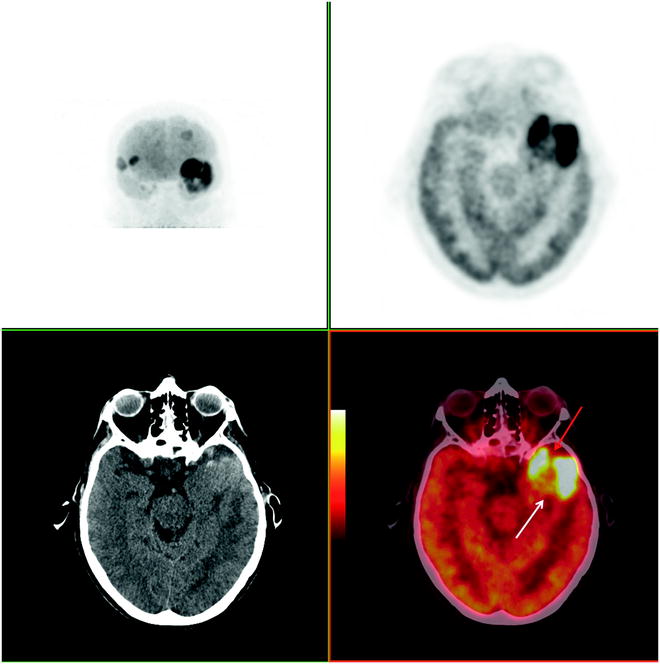
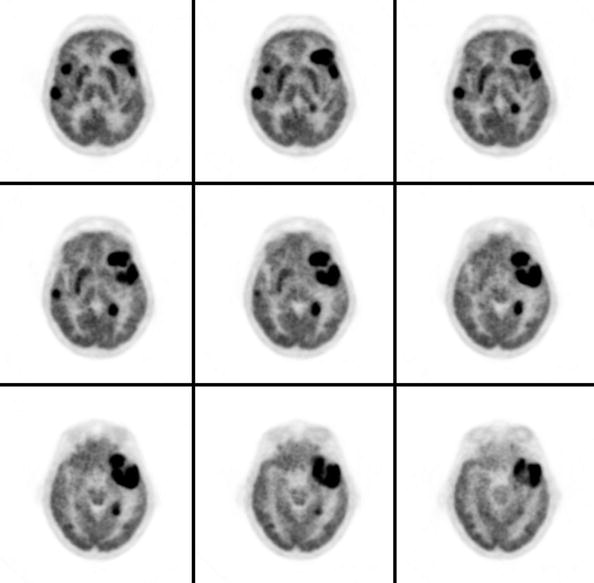
Fig. 31.9
[18F]FDG PET axial images of the brain demonstrating five hypermetabolic lesions
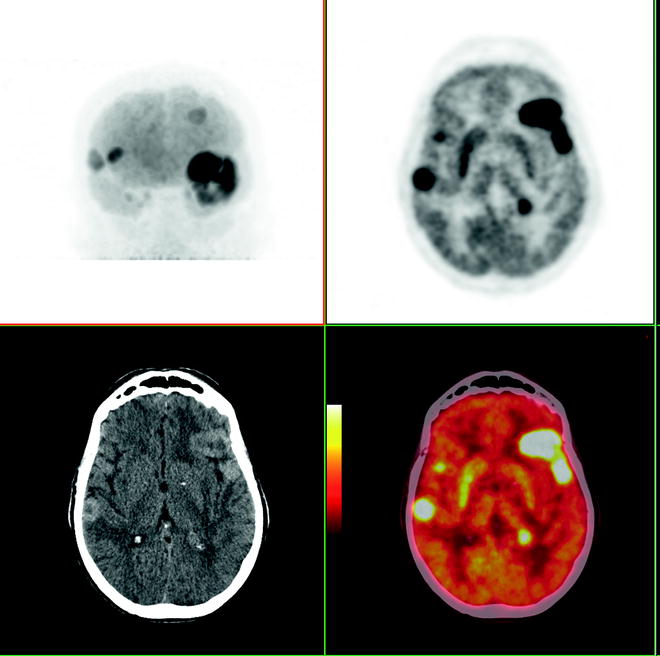
Fig. 31.10
[18F]FDG PET/CT images: upper left, MIP; upper right, axial image demonstrating five lesions; lower left, contrast enhanced CT; lower right, fused PET/CT
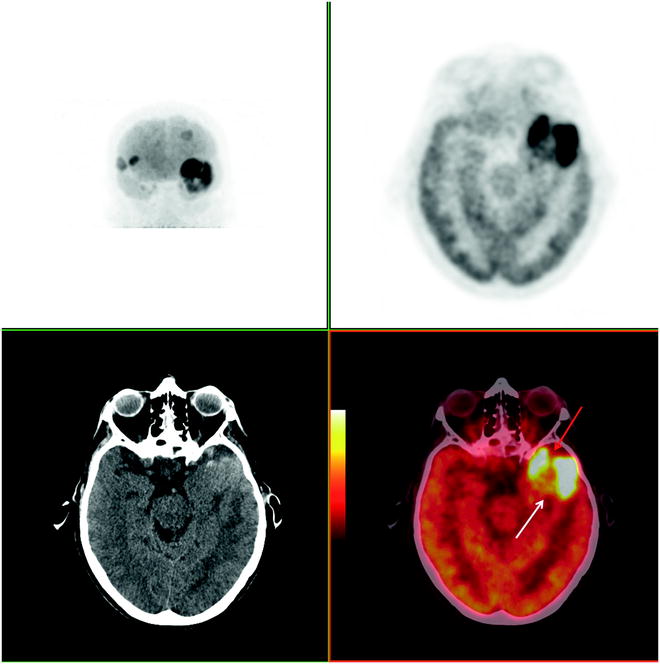
Fig. 31.11
[18F]FDG PET/CT images of primary central nervous system lymphoma (white arrow) with adjacent meningioma grade 1 (red arrow)
Discussion
This case demonstrates the value of histologic correlation of the sites of [18F]FDG localization in the evaluation of primary central nervous system lesions. In this patient with a history of treated breast cancer and a lesion with radiographic features suggesting meningioma, it is critical to determine the etiology of the lesions undergoing treatment.
Case 4: Neuroblastoma
Presentation
A 9-month-old girl presented with bilateral periorbital ecchymosis, right side exophthalmos, and abdominal distension.
Findings
CT revealed a renal mass (8 × 8 cm), retroperitoneal lymphadenopathy, as well as multiple hepatic and pulmonary lesions. CT of the head showed widespread osseous metastases and right exophthalmus. Biopsy confirmed neuroblastoma (stage IV). [123I]MIBG planar and SPECT/CT images (Fig. 31.12) show a large partially calcified left abdominal mass with pathological radiopharmaceutical uptake, representing the site of primary tumor of adrenal origin. Abnormal foci of MIBG uptake are present in both lobes of the liver, corresponding to hepatic metastasis. Multiple foci of pathological uptake in the axial and the appendicular skeleton are also seen. Bilateral lung nodules do not show focal radiotracer accumulation.
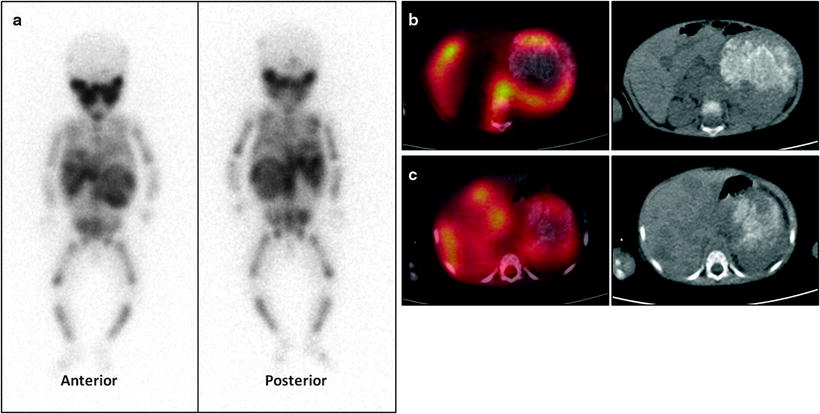
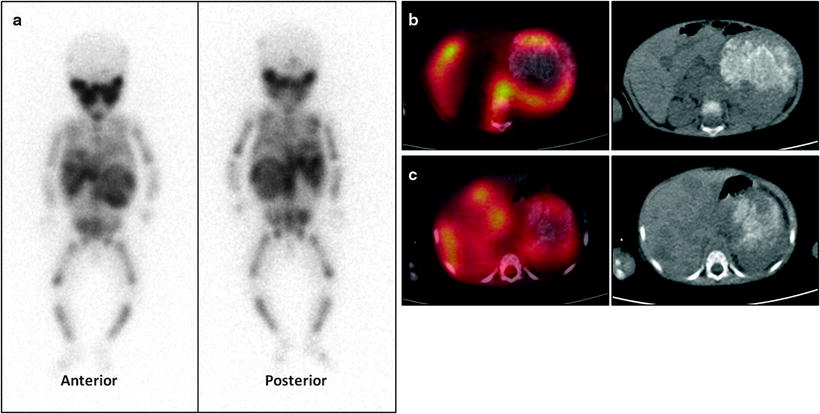
Fig. 31.12
[123I]MIBG scan. (a) Whole body image (anterior and posterior view) shows increased radiotracer uptake in the axial and appendicular skeleton. (b) Axial SPECT/CT image (fused image in the left panel and CT image in the right panel) of large partially calcified left abdominal mass. (c) Axial SPECT/CT image (fused image in the left panel, CT image in the right panel) of hepatic metastasis
As a part of initial staging [18F]FDG PET/CT was performed: images demonstrate low [18F]FDG uptake in the bone marrow of the pelvis and distal femurs and proximal tibiae (Fig. 31.13). The known abdominal mass and liver metastases do not show abnormal uptake. Bone marrow involvement was confirmed by bone marrow biopsies that revealed the presence of neuroblastoma without MYC-gene amplification.
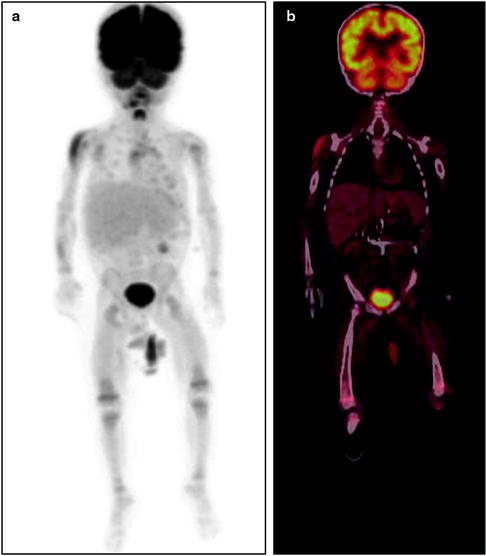
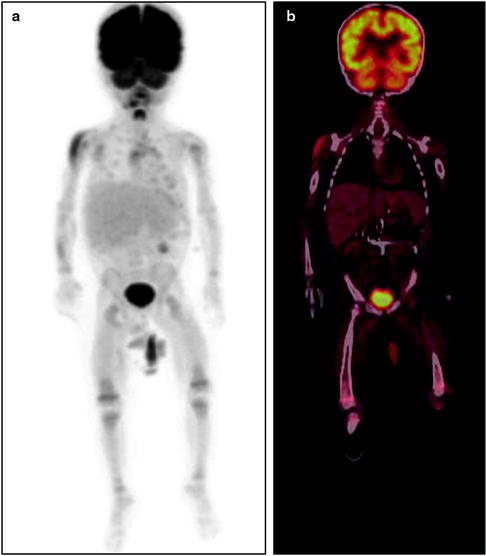
Fig. 31.13
(a) [18F]FDG MIP image demonstrates low uptake in the bone marrow of the pelvis and distal femurs and proximal tibiae. (b) [18F]FDG PET/CT fused coronal image: no abnormal uptake is seen in the known abdominal tumor or in the liver
Follow-Up
The patient was treated with neoadjuvant chemotherapy and surgery (left adrenalectomy and retroperitoneal lymphadenectomy). Follow-up evaluation after adjuvant chemotherapy showed stable disease. [123I]MIBG scan demonstrates abnormal uptake in the axial and the appendicular skeleton and in the liver (Fig. 31.14). This case demonstrates that [18F]FDG PET/CT is not as sensitive as MIBG imaging in many patients with neuroblastoma.
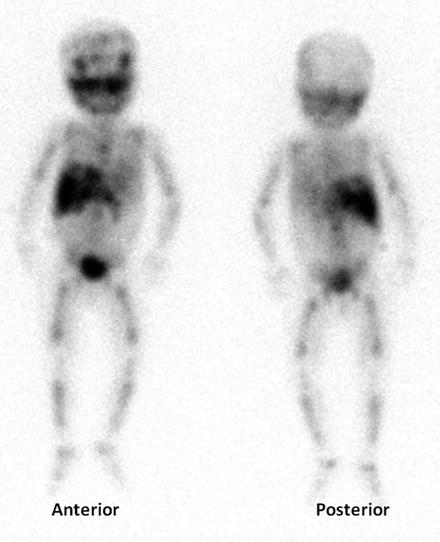
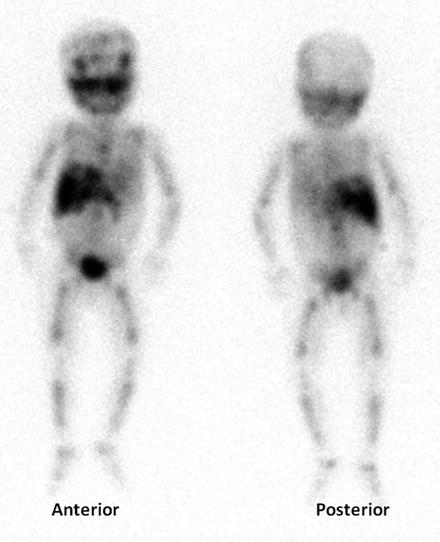
Fig. 31.14
[123I]MIBG study (whole body image) performed after chemotherapy shows the persistence of pathological uptake in the skeleton and liver
Case 5: Breast Cancer
Presentation
A 48-year-old women with inflammatory breast cancer previously treated by mastectomy and low-level axillary dissection, followed by chemotherapy and chest wall irradiation, presented with signs of recurrent breast cancer.
Findings
Findings on physical examination included a left chest wall mass with reddened overlying skin and clearly palpable axillary adenopathy. Initial staging suggested chest wall, axillary, and supraclavicular/cervical nodal disease. Core biopsy of the chest mass showed it to be high grade, ER (−), PR (−), and HER2/Neu (+) breast cancer. Skin biopsy confirmed dermal infiltration. A combination of systemic therapy and selective re-irradiation was being considered. [18F]FDG PET/CT was ordered as part of her initial staging studies. Coronal images of [18F]FDG-PET (Fig. 31.15a, b) and PET-CT fusion (Fig. 31.15c) demonstrate recurrent disease extending into the chest wall, axillary, supraclavicular, cervical, internal mammary (IM), mediastinal, and hilar lymph nodes. Image (Fig. 31.15a) shows a large L chest mass extending to the chest wall and involving skin, seen in the lateral extent of abnormal [18F]FDG uptake. In the axilla, there is diffuse, mass-like spread along the tissue planes that were part of her prior axillary dissection. PET and PET-CT fusion (Fig. 31.15b, c) also demonstrate the extension of axillary nodal disease into the deep axilla and beyond into bulky supraclavicular and cervical nodal disease. In addition, there is abnormal uptake in paratracheal, prevascular, bilateral hilar, and contralateral axillary nodal beds, strongly suggestive of metastatic cancer. An otherwise physiologic distribution of [18F]FDG uptake is seen, including uptake in the vocal cords, a normal variant.
Fig. 31.15 Coronal images of [18F]FDG-PET (a) large L chest mass and (b) axillary nodal disease. (c) PET-CT fusion of axillary nodal disease
Follow-up
The contralateral axillary disease seen on [18F]FDG PET/CT was confirmed by needle biopsy. Given the extensive spread of disease, additional radiotherapy was not used, and the patient was treated by systemic therapy alone using a combination of chemotherapy and HER2-directed therapy. This case demonstrates the value of [18F]FDG PET/CT used for restaging of recurrent and/or metastatic breast cancer and how [18F]FDG PET/CT can help direct treatment in this patient population.
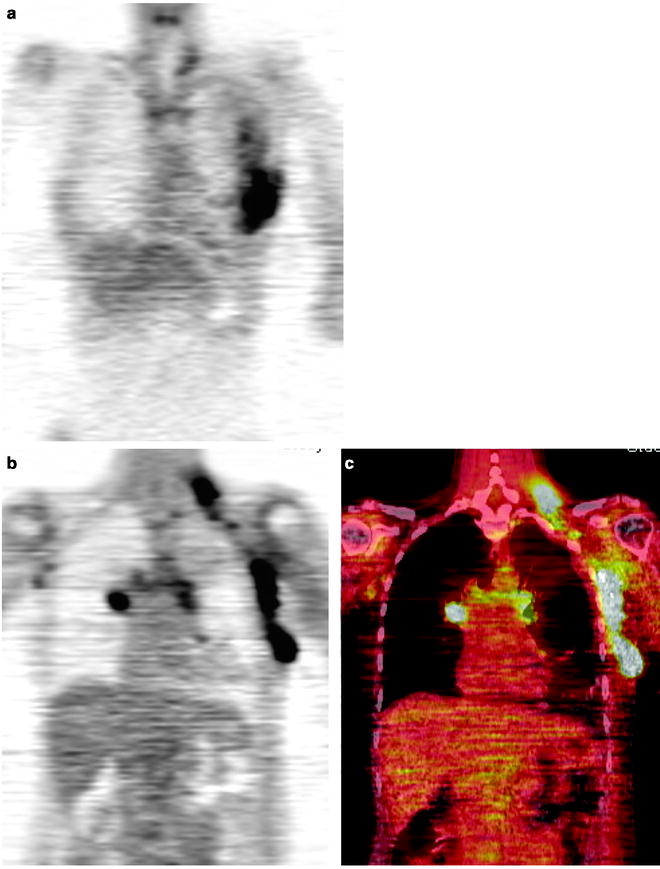
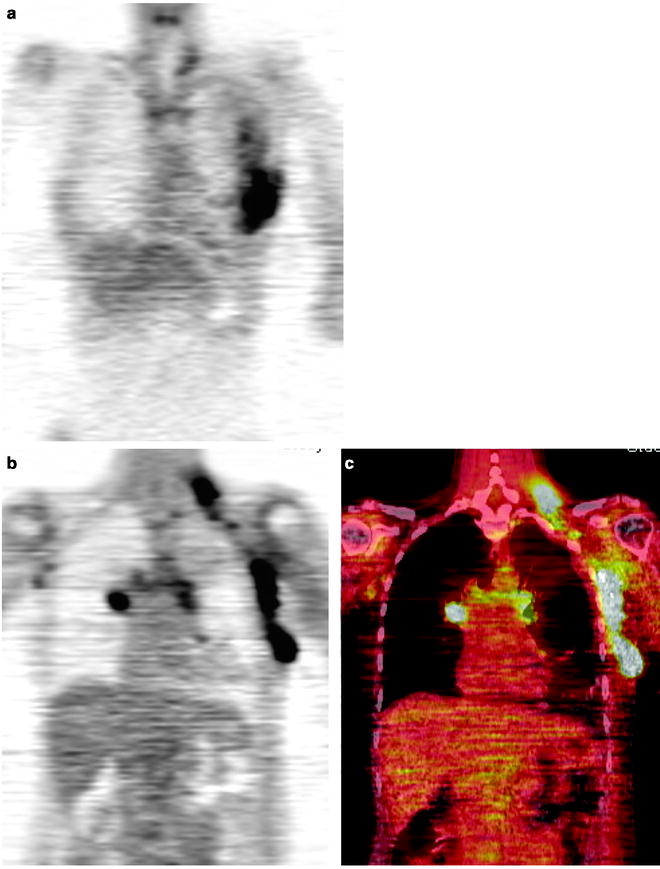
Fig. 31.15
Coronal images of FDG-PET (a) large L chest mass, and (b) axillary nodal disease. (c) PET-CT fusion of axillary nodal disease
Case 6: Paraganglioma
Presentation
A 38-year-old man presented with left-sided abdominal pain.
Findings
A CT scan showed a large retroperitoneal mass in the periaortic region. [18F]FDG PET/CT scan was done for staging. [18F]FDG PET/CT images demonstrate a large [18F]FDG-avid retroperitoneal multilobulated mass measuring 14 × 8 × 13 cm (SUVmax 41) (Fig. 31.16). Hypermetabolic adenopathy in the left neck, left paratracheal region, right retrocrural as well as para-aortic and para-caval lymph nodes are also seen (Fig. 31.17). Biopsy revealed a well-differentiated neuroendocrine tumor, consistent with paraganglioma.
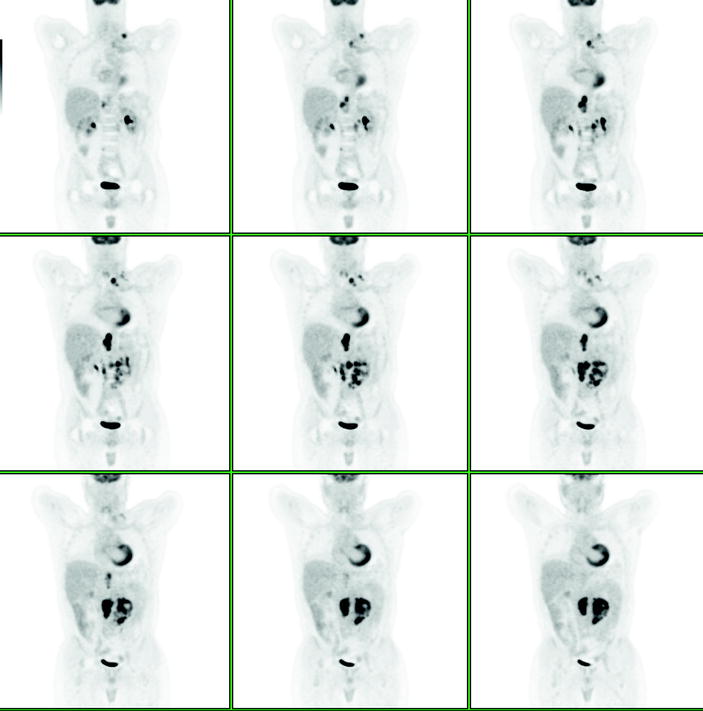
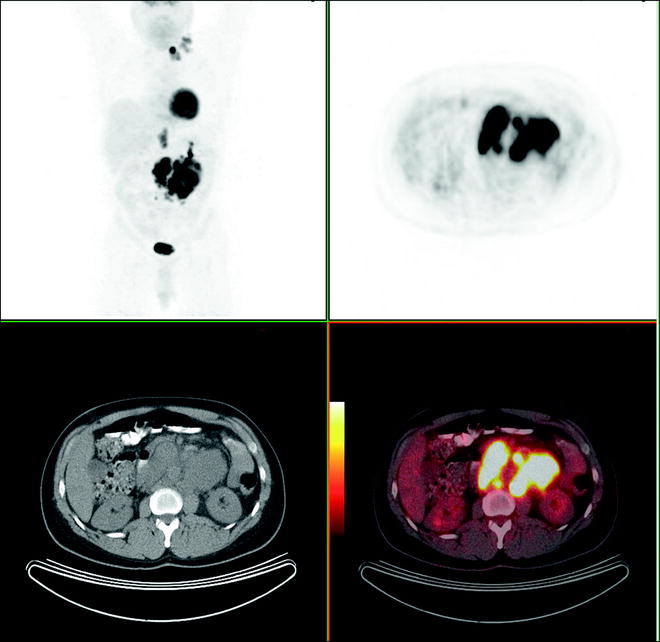
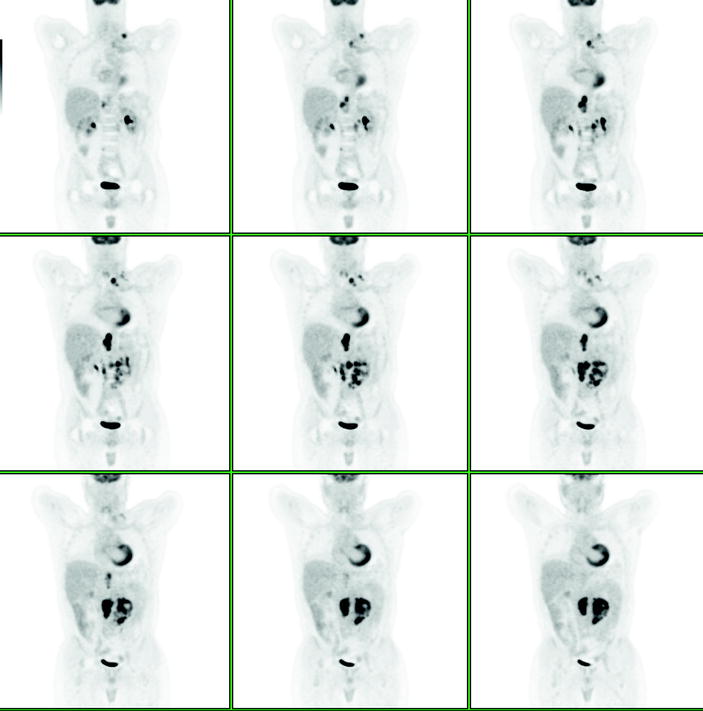
Fig. 31.16
[18F]FDG PET/CT images of a large multilobulate retroperitoneal mass with high [18F]FDG uptake
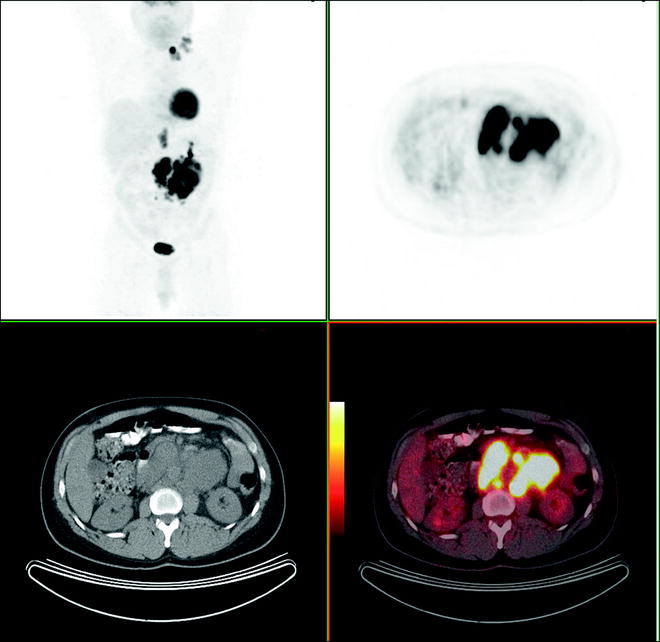
Fig. 31.17
CT and fused [18F]FDG PET/CT images of hypermetaboli adenopathy in the left neck, left upper paratracheal/thoracic region, and retroperitoneal region
The patient was treated with external beam radiation therapy. The [18F]FDG PET/CT performed to evaluate the response to therapy shows significant decrease in [18F]FDG avidity and size of irradiated left supraclavicular and retroperitoneal masses (Fig. 31.18).
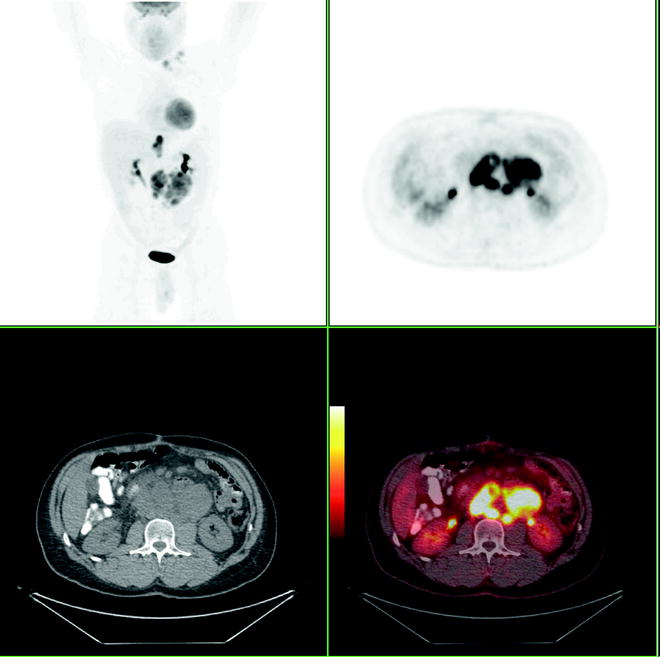
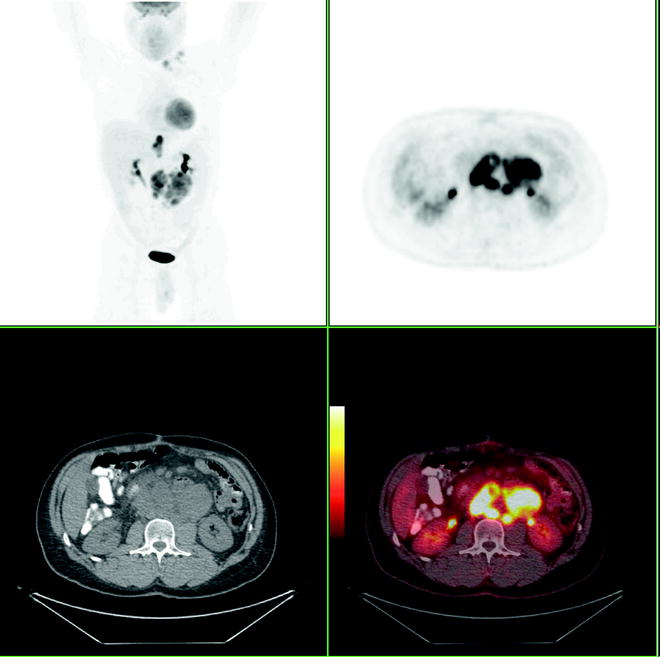
Fig. 31.18
[18F]FDG PET/CT images of paraganglioma after external beam radiation therapy, showing significant decrease in [18F]FDG activity
Discussion
This case shows that [18F]FDG PET/CT could be useful in the early assessment of response to treatment for [18F]FDG-avid lesions even in paragangliomas (that usually do not show hypermetabolic features).
Case 7: Lung Cancer
Presentation
A 72-year-old man presented with productive cough and shortness of breath.
Findings
Chest x-ray showed an infiltrate in the right middle lobe. The patient was treated with antibiotics and his symptoms improved. A subsequent CT scan revealed a right hilar mass with mediastinal and hilar adenopathy. Endobronchial biopsy demonstrated lung adenocarcinoma. An [18F]FDG-PET/CT was performed for staging (Fig. 31.19). [18F]FDG PET/CT images showed radiopharmaceutical uptake in the known primary lesion (SUVmax 16) with central photopenia, compatible with necrosis (Fig. 31.20). Additionally, an [18F]FDG-avid right hilar mass (SUVmax 11) was seen, causing collapse of the lobe due to occlusion of the middle lobe bronchus (Fig. 31.21). Hypermetabolic right and left paratracheal and subcarinal lymph nodes were also present (Fig. 31.22).
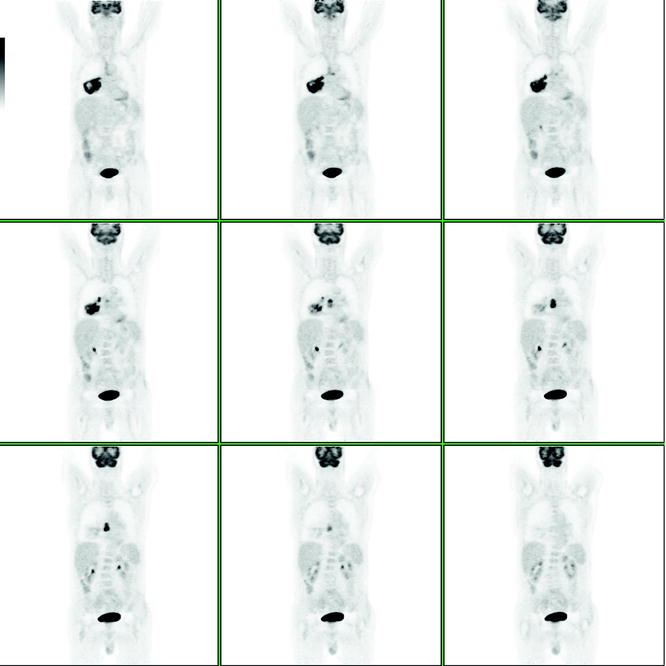
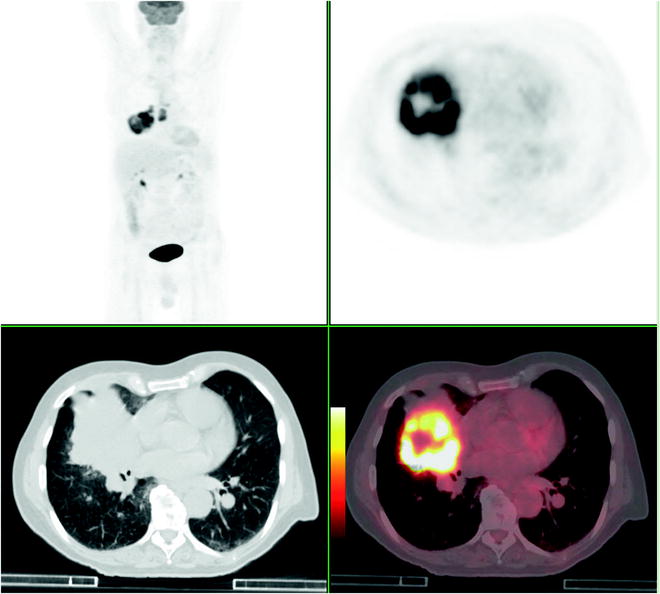
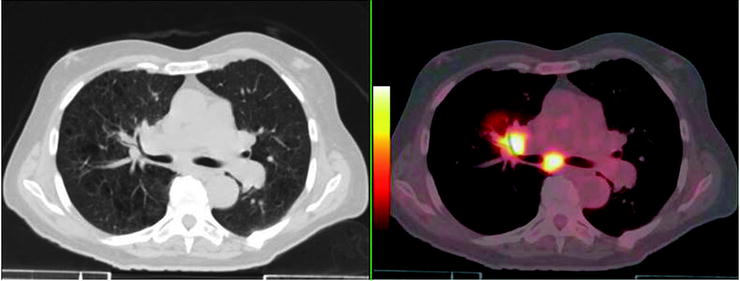
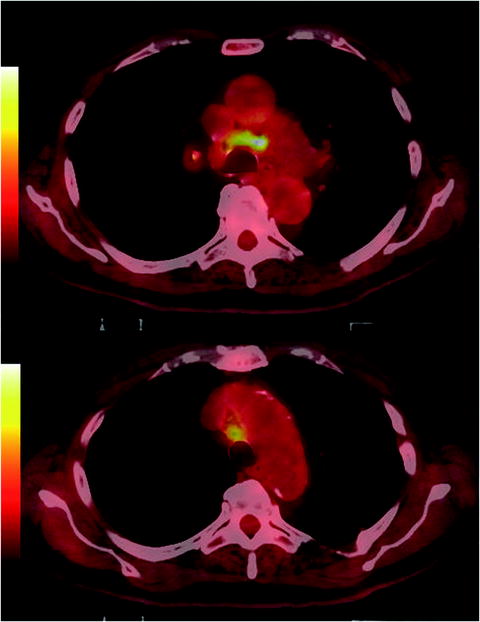
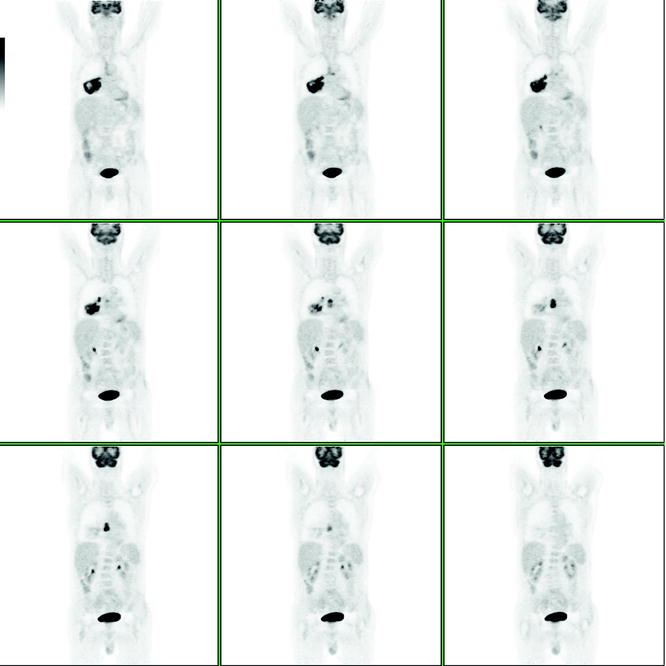
Fig. 31.19
[18F]FDG coronal images demonstrate hypermetabolic mass in the right lung and [18F]FDG-avid paratracheal and subcarinal lymph nodes
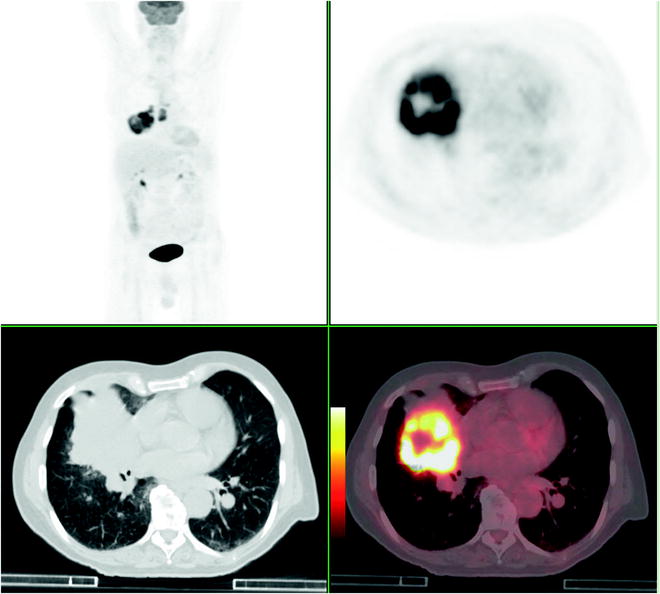
Fig. 31.20
[18F]FDG PET/CT images (upper left MIP image, upper right axial [18F]FDG image, lower left CT axial image, and lower right [18F]FDG PET/CT fused axial image). The images show a large mass in the right lower lobe with central photopenia corresponding to necrosis
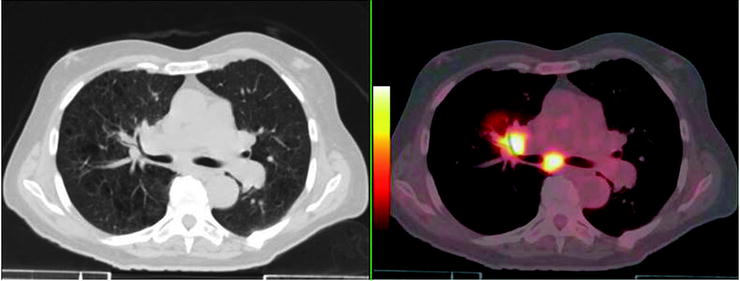
Fig. 31.21
[18F]FDG-PET/CT image (CT axial view in the left panel, [18F]FDG PET/CT fused axial view in the right panel) of [18F]FDG-avid right hilar mass (SUVmax 11) occluding the middle lobe bronchus
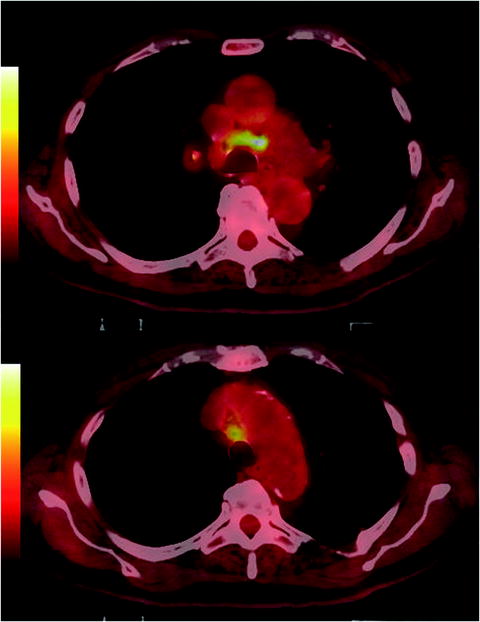
Fig. 31.22
[18F]FDG PET/CT fused axial images of hypermetabolic adenopathy in carinal region
The patient was treated with chemo- and radiation therapy. [18F]FDG PET/CT performed to evaluate response to treatment demonstrated a decrease in the size and intensity of the hypermetabolic right hilar mass (Fig. 31.23).
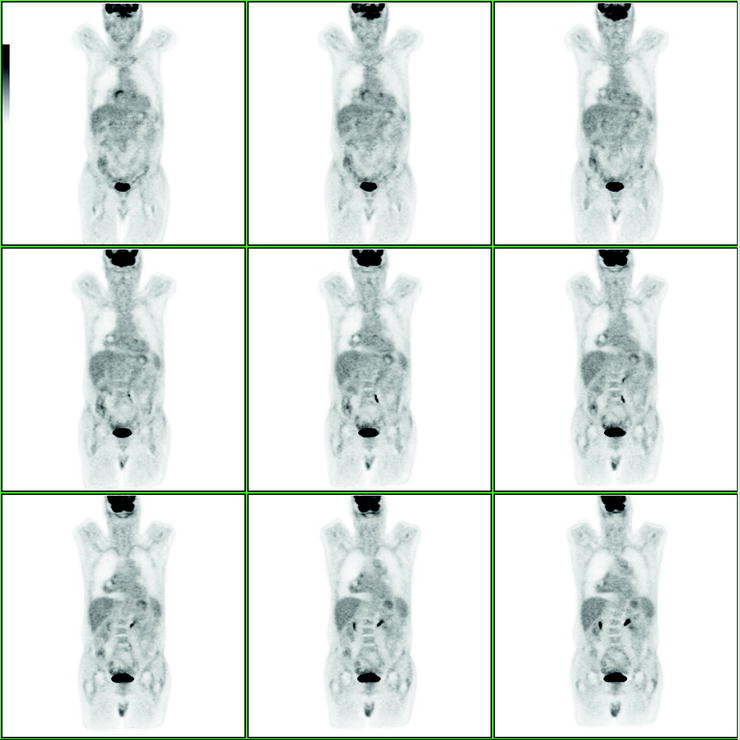
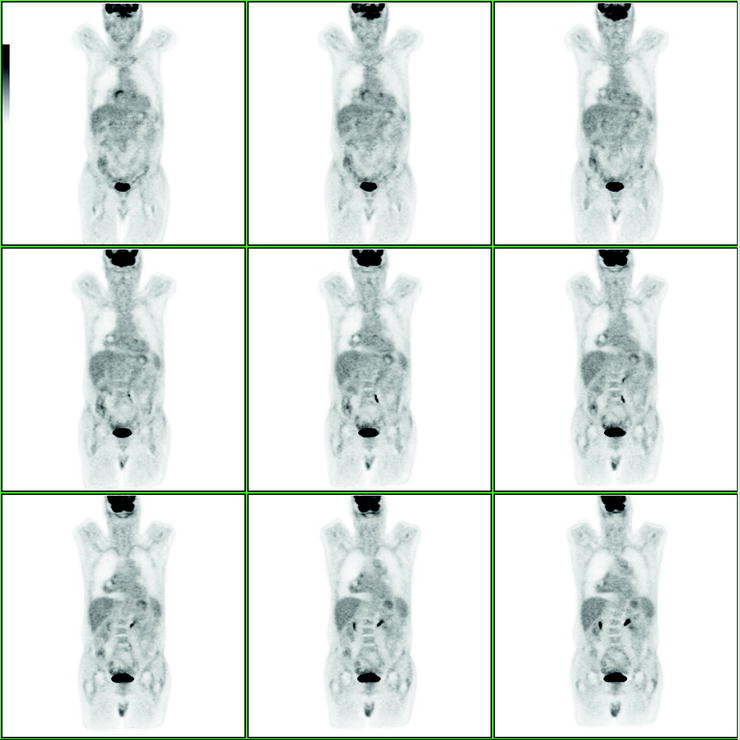
Fig. 31.23
[18F]FDG PET/CT coronal images after chemoradiation therapy demonstrates a decrease of radiotracer uptake as well as reduction in size of the right pulmonary lesion
Discussion
[18F]FDG PET/CT is useful in the initial evaluation of patients with squamous cell lung cancer and adenocarcinoma. Squamous cell cancers are generally more [18F]FDG avid than adenocarcinoma. Findings may be subtle in patients with bronchoalveolar cancer.
Case 8: Lung Cancer
Presentation
This 85-year-old male patient was referred following a chest x-ray and CT performed at a 1 month interval and showing a 5 × 5 × 4 cm RLL (right lower lobe) mass. The differential diagnosis included a pulmonary abscess, round actelectasis, and pneumonia.
Findings
Biopsy indicated the presence of NSCLC. PET/CT was performed for staging (Fig. 31.24a). Selected transaxial CT, PET and fused PET/CT slice, and MIP (maximum intensity projection) image (lower right) show an [18F]FDG-avid RLL mass (SUVmax 11.3) with a photopenic/necrotic center and an avid right hilar node (SUVmax 4.1), corresponding to T2aN1M0 disease. Due to a history of ischemic heart disease and stage 3 renal failure, the patient was considered to be at high risk for surgery and was referred for additional investigations including a cardiology work-up and CT of the brain (which the patient refused to perform). During this prolonged presurgical evaluation, the patient developed RLL pain and cough and was referred to a repeat PET/CT at a 3 months interval to the first study with the suspicion of local tumor infiltration. The second PET/CT study (Fig. 31.24b) showed marked disease progression. The main tumor mass has increased in size to 6.5 cm in diameter and is invading the chest wall. There are multiple new [18F]FDG-avid right lung lesions, pleural deposits (arrow), an anterior mediastinal node, and left adrenal metastasis (open arrow). These findings correspond to T4N2M1b disease (Fig. 31.24b).
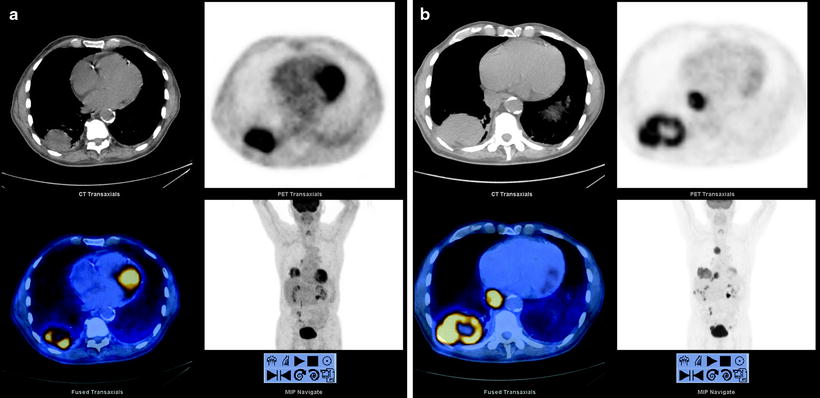
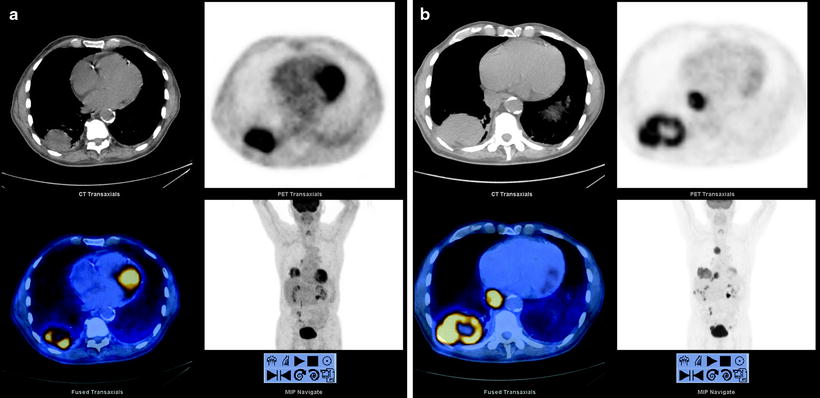
Fig. 31.24




(a) PET/CT was performed for staging for this patient’s tumor. (b) The second PET/CT study showed marked disease progression
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree