Fig. 10.1
Schematic illustration depicting compression point 1, where the nerve exits from deep to the obliquus capitis, wrapping around as it moves cranially and superficially (With permission from Janis et al. [4])
Fig. 10.2
Schematic illustration depicting compression point 2, the entrance of the nerve into the semispinalis muscle (With permission from Janis et al. [4])
Fig. 10.3
Schematic illustration depicting compression point 3, where the greater occipital nerve exits from the semispinalis muscle (With permission from Janis et al. [4])
Fig. 10.4
Schematic illustration depicting compression point 4, where the nerve enters the trapezius (With permission from Janis et al. [4])
Fig. 10.5
Schematic illustration depicting compression point 5, where the nerve enters the trapezius insertion (With permission from Janis et al. [4])
Fig. 10.6
Schematic illustration depicting compression point 6. Different types of greater occipital nerve–occipital artery relationships are shown. SC single cross, HI helical intertwining (With permission from Janis et al. [4])
1.
The space between the vertebral bones of C1 and C2
2.
The atlantoaxial ligament as the dorsal ramus emerges
3.
The deep to superficial turn around the inferiolateral border of the obliquus capitis inferior muscle and its tight investing fascia
4.
The deep side of semispinalis capitis, where initial piercing can involve entrapment in either the muscle itself or surrounding fascia
5.
The superficial side of semispinalis capitis, where completion of nerve piercing muscle and its fascia again poses risk
6.
The deep side of the trapezius as the nerve enters the muscle
7.
The tendinous insertion of the trapezius at the superior nuchal line
8.
The neurovascular intertwining of the GON and the occipital artery
Traumatic extension injuries (i.e., whiplash) have also been proposed as potential causes, although a definitive mechanism by which such injury could occur has yet to be fully elucidated (Fig. 10.7) [7–9].
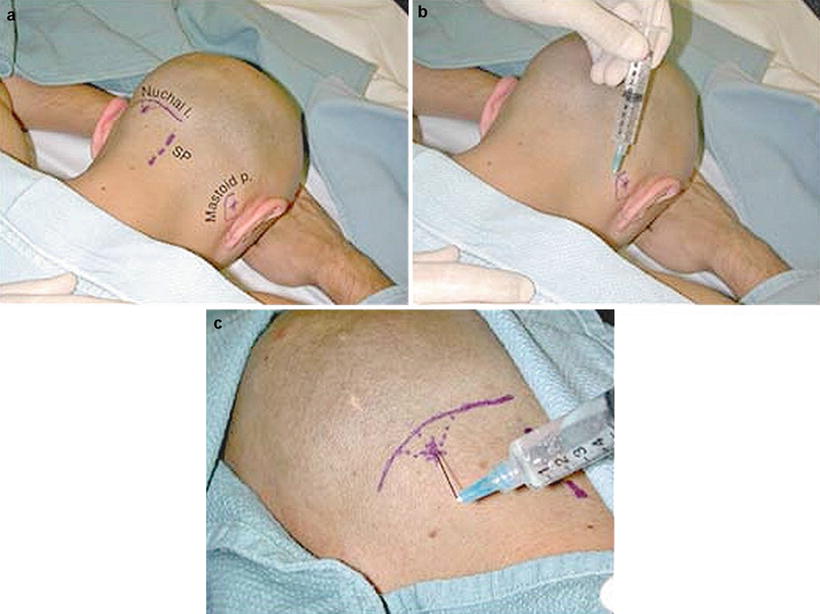
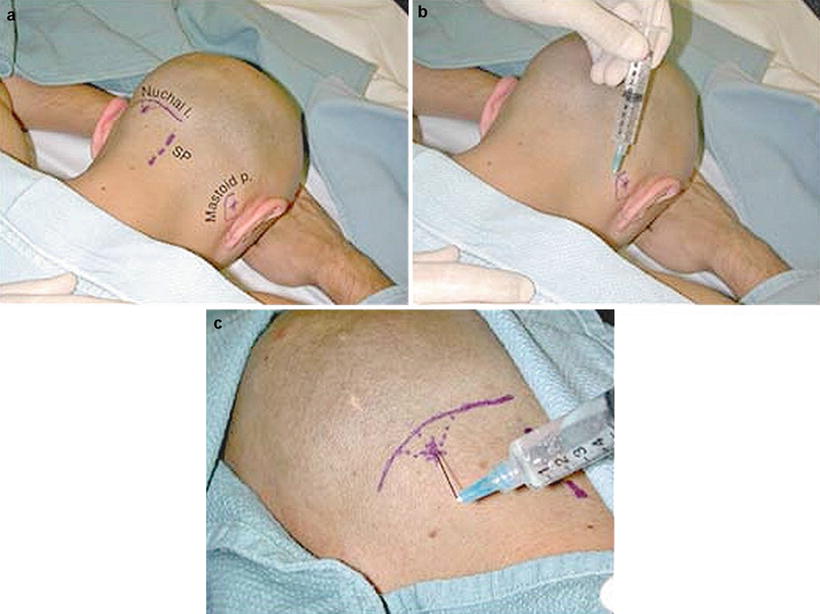
Fig. 10.7
(a) Surface anatomy of the occipital area. (SP spinous processe). (b) Lesser occipital nerve injection at the mastoid process. (c) Greater occipital nerve blockade at the superior nuchal ridge. Anatomic landmarks for greater and lesser occipital nerve block (From Chelly [6]. Copyright ©2009 Lippincott Williams & Wilkins)
Technique
As with all interventional procedures, a thorough and in-depth understanding of the relevant anatomy is an absolute a priori requirement to both successful neural blockade and minimization of potentially deleterious consequences. Unfortunately, despite the common frequency with which this block is internationally performed, there exists no standardized protocol for performing the procedure in either daily clinical practices or peer-reviewed medical literature.
Anatomical landmark identification [3, 10], point of maximal tenderness isolation [11], typical headache pain reproduction [11], ultrasonic Doppler flowmetry-assisted occipital artery localization [12], nerve stimulator guidance [13], and ultrasound image assistance [9] have all been employed in an effort to reproducibly identify the appropriate injection site. Nevertheless, the exact location for deposition of injectate varies widely in published studies in terms of both mediolateral and rostrocaudal orientation. All too often, no formal protocol is described at all, with authors simply stating that medications are injected in the “region of the greater occipital nerve” [14]. Clinically these discrepancies in localization may be serendipitously alleviated somewhat by the not inconsequential injectate volumes employed, frequently five or even as many as 10 ml [15]. As such, any notion of specificity is rendered suspect at the very least and quite implausible at most, as in so doing yields procedures more akin to general field blocks than selective peripheral neural blockade.
Many authors employing landmark identification suggest palpation of the occipital artery, which frequently courses just lateral to the nerve. However, several pertinent issues may conspire to obscure such identification. One, anatomical variations to conventionally accepted neurovascular association are common. Two, the zone of palpation lies cephalad to typical hairlines, which may make palpation infeasible in the overly hirsute. Three, the occipital artery quite often lacks the vasodynamic bounding of more sizable vessels and thus may not be easily discernable, especially in patients of excess habitus. For these reasons, ultrasonic Doppler flowmetry may be employed to increase the likelihood of arterial localization, with purported increases in success rate and density of blockade, along with decreases in symptoms of vascular uptake as compared to more traditional approaches.
Although multiple techniques have been described, the clinical or statistical superiority of one method over competing approaches has never been validated. The practitioner, therefore, is left with myriad options from which to choose, depending on their personal experience, comfort level, and skill set. At the very least, it would appear that identification of the inion is a prerequisite to block performance, as is a topographical appreciation for the underlying subcutaneous and intermuscular course of the nerve.
Isolating a suitable location for injection is only one aspect of the procedure, however, which leads to the choice of injectate. Published study protocols have varied widely, including the use of both short- and long-acting local anesthetics, sometimes but not always including epinephrine, with or without a number of different steroids, plus or minus additives including but not limited to opioids and alpha-2 agonists. Botulinum toxin has also been employed with some success. Additionally, the chosen injectate volumes are far from uniform, with a single milliliter employed in some trials and as much as 10 ml in others.
What this implies, of course, is that there is either insufficient evidence at this stage to ascribe superiority of one medication regimen over another or, perhaps equally likely, there is simply no appreciable advantage to be elucidated. For instance, Naja et al. [16] injected 3 ml of a 10-ml mixture that included 3 ml of lidocaine 2 %, 3 ml of lidocaine 2 % with epinephrine 1:200,000, 2.5 ml of bupivacaine 0.5 %, 0.5 ml of fentanyl 50 mcg/ml, and 1 ml of clonidine 150 mcg/ml. The authors suggest that this mixture demonstrates superior longevity that exceeds the expected duration of action of the local anesthetic alone. However, Arner et al. [17], using 0.5 % bupivacaine alone, obtained analgesia that exceeded the expected duration of effect in 18/38 consecutive patients treated for peripheral neuralgia. Thus, the incremental improvements in dose response attributable to additives remain uncertain.
Lastly, there exists some evidence to substantiate the efficacy of frequently repeated injections over single interventions to achieve prolonged analgesia. Naja et al. [18] performed occipital nerve blocks repeatedly in 47 patients with cervicogenic headache and were able to achieve a 6-month period of pain relief in 96 %. Interestingly, the authors found that the number of blocks required to reach this end point could be predicted by adding one injection for every 3 years of headache history. Similarly, Caputi and Firetto [19] succeeded in obtaining a 50 % or greater reduction in the total pain index in 23/27 patients using repetitive local anesthetic-only blocks in the treatment of chronic migraineurs.
Indications
1.
Occipital neuralgia
2.
Cluster headache
3.
Cervicogenic headache
4.
Migraine
8.
Postconcussive headaches
12.
Rescue treatment for headaches proving recalcitrant to other measures
13.
As an adjuvant to medication-overuse headache
Likely Ineffective
1.
Tension headache
2.
Hemicrania continua
3.
Chronic paroxysmal hemicrania
Contraindications
1.
Patient refusal
2.
Bleeding diathesis
3.
Local or systemic infection
4.
Local neoplastic disease
Evidence-Based Review
In recent years, numerous studies have been published demonstrating the efficacy of GONB in multiple chronic pain and other conditions. Quite surprisingly, however, there are few randomized, double-blind, placebo-controlled trials, and the preponderance of evidence available is confounded by methodological discrepancies in diagnosis, technique, treatment, and outcome. Regardless, the available evidence does suggest that several conditions are likely to respond favorably to GONB. Perhaps this ambiguity in diagnostic response is more attributable to insufficient understanding of underlying pathophysiology and resultant overlap in ascribed diagnoses. Alternatively, the functional anatomical convergence of the occipital afferents and the trigeminal nerve complex in the proximal cervical spinal cord may render multiple distinct disease states susceptible to the same intervention. Evidence for this theory is supported by multiple findings. Goadsby et al. [22] showed that the cervical dorsal horn and trigeminal nucleus caudalis show increased metabolic activity during stimulation of the occipital nerve, suggesting that the second-order neurons overlap in their nociceptive processing. This finding was supported by the work of Piovesan et al. [23], who elicited pain in the distribution of the trigeminal nerve, including parasympathetic activation suggestive of trigeminal autonomic activation, during sterile water injection over the greater occipital nerve. More recently, Busch et al. [24, 25




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








