Case presentation
An 8-year-old boy presents with 3 days of cough, fever, and headache. He had been seen the previous day by his primary care physician and he was told to come to the Emergency Department after a chest x-ray performed as an outpatient demonstrated findings concerning for pneumonia. Six weeks ago, he was diagnosed with a right lower lobe pneumonia and treated with oral amoxicillin but failed to clinically improve and was admitted to the hospital for further management. He improved clinically and was discharged to complete a course of oral antibiotics.
Medical history is notable for a diagnosis of reactive airway disease at 3 years of age, which mostly responded to treatment with bronchodilators. His mother observed that he seemed to have more breathing problems over the last 3 years, and he was diagnosed as an outpatient multiple times over this time period with clinical pneumonia and “bronchitis.”
Physical examination reveals a nontoxic child whose only complaint is right-sided chest pain with deep inspiration. His vital signs demonstrate a temperature of 102 degrees Fahrenheit, a heart rate of 130 beats per minute, a respiratory rate of 24 breaths per minute, a blood pressure of 127/68 mm Hg, and a pulse oximetry reading of 95% on room air. He has an unremarkable examination other than his pulmonary exam, which has decreased breath sounds on the right without crackles or rhonchi, but there is mild inspiratory and expiratory wheezing; he has no retractions or grunting.
Imaging considerations
Plain radiography
While the vast majority of pediatric patients with wheezing will have a viral etiology, the clinician should broaden the differential diagnosis in patients with persistence of respiratory symptoms. This can be divided into two major categories: structural causes and functional causes. Structural causes include vascular rings and slings, tracheomalacia, tracheal stenosis, tracheal webs, and masses. Functional causes include asthma/reactive airway disease, gastroesophageal reflux disease (especially in infants), vocal cord dysfunction (especially in adolescent patients), persistent or recurrent infection, and foreign bodies. Plain radiography is the initial imaging modality of choice for patients with persistent wheezing or other respiratory symptoms (such as tachypnea or hypoxia).
A two-view study (posterior-anterior or anterior-posterior and lateral) should be obtained when possible.
Computed tomography (CT)
CT is a second-line imaging modality for evaluating complicated lung disease, particularly lesions affecting the bronchus or if there is a concern for a bronchial foreign body. CT provides greater definition of the underlying pathology than plain film. In addition, given the typically broad differential, CT can help to give guidance on the next steps in diagnosis and treatment, and can localize pathology, to help direct bronchoscopy or surgery. If CT is being obtained for acute foreign body aspiration, intravenous (IV) contrast is not necessary. However, for more subacute processes or processes that may be infectious or related to a malignancy, IV contrast should be used to define the vasculature, differentiate vasculature from adenopathy or other mass, and to help characterize a mass, pneumonia, or abscess.
Ultrasound (US)
Unlike in the evaluation of more typical pneumonias and effusions, lung US does not provide sufficient detail for evaluation of processes involving the bronchial tree.
Magnetic resonance imaging (MRI)
This modality is not used for first-line imaging and may be employed in patients who require further clarification of plain radiographic or CT findings.
Imaging findings
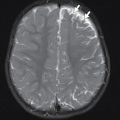
The patient underwent plain chest radiography. A selected image from this study is provided here. This examination was compared to chest radiograph from 6 weeks prior (not shown) and revealed persistent right lower lobe consolidation and volume loss with no significant interval change ( Fig. 40.1 ).


Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree