Fig. 1
Anteroposterior radiograph of the pelvis demonstrates areas of sclerosis in both sacral ala (arrows) consistent with insufficiency fractures
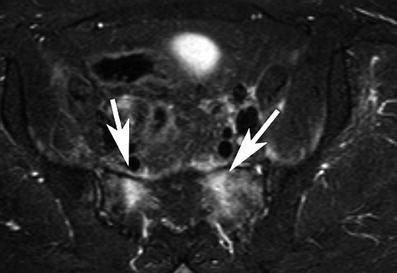
Fig. 2
Axial MRI (STIR-sequence) of the pelvis demonstrating bone marrow edema pattern in bilateral sacrum compatible with bilateral insufficiency fractures

Fig. 3
Axial MRI (T1-w-sequence) demonstrating signal loss in both sacral ala compatible with bilateral insufficiency fractures in a 55-year-old woman after radiotherapy of the pelvis for cervical carcinoma

Fig. 4
AP radiograph of both hip joints shows insufficiency fractures (arrows) in the left parasymphyseal region and the left periacetabular region. Total hip replacement is an additional predisposing causative factor

Fig. 5
Coronal CT-reformation of the sacrum demonstrates sacral insufficiency fractures at S1 with fracture lines and sclerosis. Posterior spinal fusion Th12-S1 with loosening of T12 pedicle screws

Fig. 6
AP radiograph of the sacrum after orthopaedic trans-sacroiliac screw fixation of bilateral sacral insufficiency fractures at the S1 level
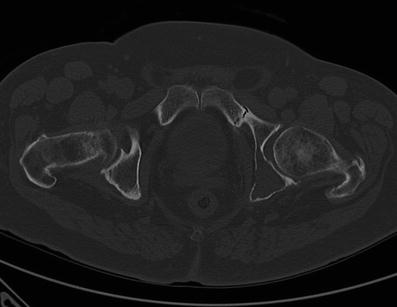
Fig. 7
Axial CT image at the level of the hip joints demonstrates insufficiency fracture of the left pubic bone (arrow), note also osteolysis of the left posterior acetabulum due to multiple myeloma in this 55-year-old male (arrowhead)
It should also be noted that multiple pelvic insufficiency fractures are frequently found, particularly in the presence of pubic or acetabular fractures, and careful search for concomitant fractures is warranted. In a previous study in 70.3 % of cases with pelvic insufficiency fractures, multiple fracture sites were present. In the case of pubic fractures in 90 % concomitant fractures were present. Also, 76 % of acetabular fractures had concomitant fractures present (Cabarrus et al. 2008).
1.5.2 Lower Extremity
Insufficiency fractures of the fibula are typically found in patients with underlying rheumatic diseases, mainly rheumatoid arthritis (Alonso-Bartolome et al. 1999; Yamamoto et al. 2002) (Figs. 8, 9). Insufficiency fractures are also frequently found at the metatarsal bones in particular in the setting of inflammatory arthropathies (Fig. 10). Also these may be diagnosed in patients with severe osteoporosis, high-dose corticosteroids, or methotrexate therapy. Patients with marked joint deformity are also at high risk for developing insufficiency fractures (Maenpaa et al. 2002). Less frequently, in up to 25 %, insufficiency fractures at the femoral shaft can occur, predominately in elderly patients with osteoporosis (Martin-Hunyadi et al. 2000) (Fig. 11). Insufficiency fractures at the tibia (Fig. 12a–c) may be found as an early manifestation of bone failure in patients after renal transplantation as reported by a previous study (Franco et al. 2003). The main causes are preexisting renal osteodystrophy, glucocorticoid therapy, and hyperparathyroidism, whether residual or secondary to imperfect graft function (Franco et al. 2003). Longitudinal stress fractures of the tibia can also occur in patients with healed chronic osteomyelitis (Feydy et al. 2000). Even postpartum osteoporosis was found to be a cause of insufficiency fractures around the knee (Clemetson et al. 2004).
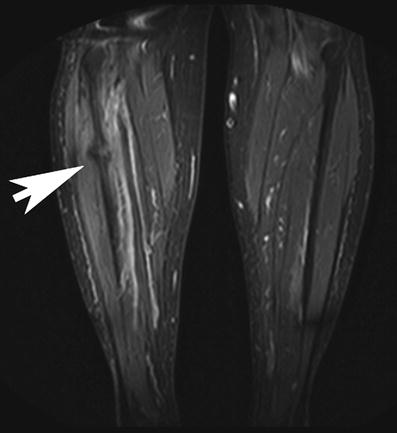



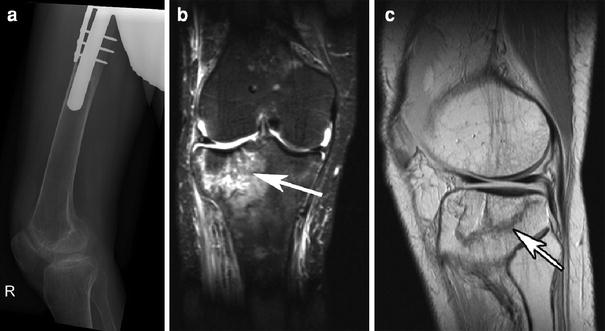
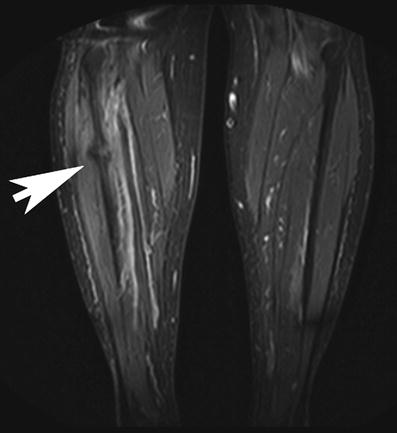
Fig. 8
Coronal STIR MR sequence of both lower extremities demonstrating marrow edema and subtle fracture line due to insufficiency fracture at the right fibula

Fig. 9
AP radiograph of the left knee demonstrating an old insufficiency fracture of the right fibula with callus formation after total knee replacement

Fig. 10
Dorso-plantar radiograph of the right foot demonstrates insufficiency fracture of the second and third with massive callus formation in this 85-year-old female patient

Fig. 11
AP radiograph of the right proximal femur with sclerosis and subtle fracture line at the medial aspect of the femur shaft below the lesser trochanter (arrow) indicating an old insufficiency fracture; note generalized osteopenia; and internal fixation hardware at the distal femur
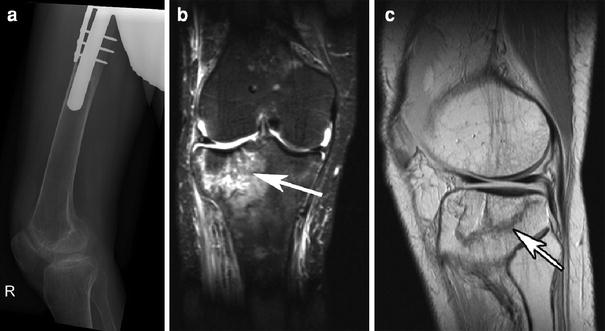
Fig. 12
Patient with history of tumor endoprosthesis at the proximal femur and insufficiency fracture at the proximal tibia. Lateral radiograph of the distal femur and knee shows severe osteopenia but no fracture a. The coronal STIR sequence shows significant bone marrow edema pattern and subtle fracture line at the lateral tibia b. The sagittal T1-w image better demonstrates the fracture line in the same patient c
One of the important differential diagnoses of subchondral insufficiency fractures of the femoral head may include osteonecrosis. Typical MRI findings in insufficiency fractures include a pattern of bone marrow edema with a low-signal-intensity line (resp. fracture) on the T1-weighted images parallel to the subchondral bone. In general, the circumscribed lesions on MRI, which are commonly observed in osteonecrosis, are not found (Yamamoto et al. 2007). Histopathologically fracture callus, reactive cartilage, and granulation tissue is seen without any evidence of antecedent osteonecrosis. The subchondral insufficiency fracture of the femoral head (SIF) is a recently recognized cause of acute onset arthritis mostly in elderly women, which previously had been commonly considered either as osteonecrosis or osteoarthritis.
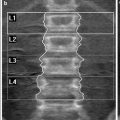
1.5.3 Spine
Insufficiency fractures at the spine are a leading cause for acute low back pain without an acute traumatic event. Usually a concave or wedge-shaped deformity of the affected vertebra is found and a wide range of the vertebral height ratios and fracture distribution were reported (Kawaguchi et al. 2001). Once an initial vertebral fracture is sustained, the risk of subsequent vertebral fracture increases significantly. However, this effect cannot be explained by low bone mass alone, suggesting that factors independent of this parameter contribute to this occurrence (Briggs et al. 2007). The assessment of vertebral fractures using a semiquantitative approach has been described, grading osteoporotic fractures into type 1 (20–25 % deformity), type 2 (25–40 %), and type 3 (>40 %) (Genant et al. 1993). Accurate radiographic diagnosis of osteoporotic vertebral fractures is important. Several studies indicated a false-negative rate of up to 34 % in reports of lateral radiographs of the thoracolumbar spine (Delmas et al. 2005). Radiologists should be aware of the importance of vertebral fracture diagnosis in assessing future osteoporotic fracture risk. Vertebral fractures incidental to radiologic examinations done for other reasons should be identified and reported, in particular vertebral fractures should be assessed in lateral chest radiographs. Proper training of radiologists is necessary to improve detection of vertebral fractures (Lentle et al. 2007). In oncologic patients differentiation from benign and malignant vertebral fractures is important and can be achieved by MRI or PET-CT (Figs. 13, 14).
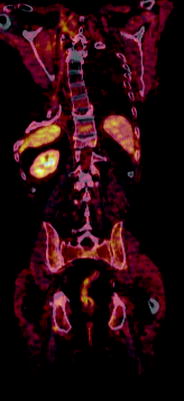
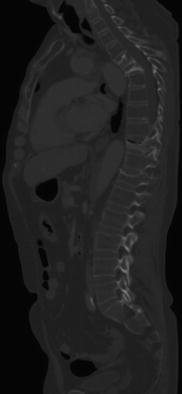
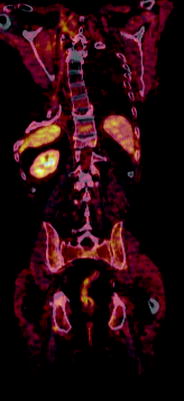
Fig. 13
61-year-old female patient with a history of bronchial carcinoma, FDG-PET-CT showing only moderate metabolic activity in the thoracic spine with several compression fractures. PET-CT excludes malignant fractures due to underlying disease
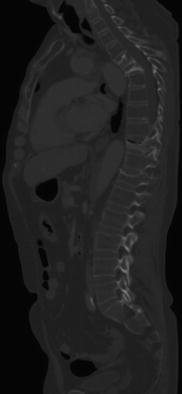
Fig. 14
Same patient as in Fig. 13 demonstrating multiple vertebral fractures with gibbus at the thoracic spine
1.5.4 Upper Extremity
A common site of fragility fractures is the distal forearm. In addition, fractures involving the wrist are known to be strongly associated with osteoporosis. It is well-known that patients with distal radius fracture who are otherwise healthy have a preferential bone loss at the distal forearm. Distal radius fractures are also associated with generally low bone mass and elevated fracture risk at other skeletal sites. In these subjects pharmacotherapy for osteoporosis is warranted (Mallmin and Ljunghall 1994). Interestingly in osteoporosis the proximal humerus may also be a fracture site at risk (Guggenbuhl et al. 2005).
1.6 Differential Diagnosis
An important differential diagnosis of a stress/insufficiency fracture is a fracture due to malignant disease. MRI features of a malignant fracture are diffusely or focally abnormal bone marrow signal which may be either well-defined or ill-defined and does not follow fracture lines. In addition abnormal intracortical, periosteal, or muscle signal intensity are found as well as endosteal scalloping and soft-tissue masses. The features seen on CT are bone marrow abnormality which may be well-defined, ill-defined, permeative or moth-eaten, endosteal scalloping, periosteal reaction, and a soft-tissue mass. Accuracy for differentiating malignant fractures from stress fractures was reported to be highest with MRI (93–98 %) followed by CT (82–88 %) and radiographs (88–94 %) (Fayad et al. 2005).
1.7 Imaging Methods and Limitations
Radiographs are the initial imaging test in patients with pain localized to the skeleton. If the radiographs are inconclusive and pain persists, either MRI or CT will be performed. Multidetector computed tomography (MDCT) is currently standard and allows multiplanar reconstruction, near isotropic 3D reconstructions of anatomical structures, reduction of artefacts as well as thin-section high-resolution imaging which is beneficial to visualizing also subtle fracture lines. It should be considered, however, that MRI is more sensitive and the imaging modality of choice if the patient history suggests malignant disease and metastasis may be responsible for fracture. Though MRI is very sensitive for detection of fractures, bone marrow changes, and related soft-tissue edema, it should be considered that in the absence of fractures lines or a typical history MRI may also be misleading and suggest other bone marrow pathology such as malignant infiltration. While MRI is the most sensitive technique in the visualization of insufficiency fractures, CT sometimes tends to depict the extent and stability of these fractures better. Bone scintigraphy is highly sensitive, but not specific. Atypical uptake patterns may be difficult to interpret and abnormal uptake may persist for several months.
1.7.1 Radiographs
Radiographic findings depend on the site of the fracture. Parasymphyseal and pubic ramus fractures may have an aggressive appearance that depends on the stage of fracture maturity. Findings include sclerosis, lytic fracture line, bone expansion, exuberant callus, and osteolysis. The most common finding is a sclerotic band or line. A lytic fracture line or cortical break rarely is observed. The degree of confidence is low in sacral fractures because of osteoporosis, overlying bowel gas, and calcified vessels and is better at peripheral sites like in long bones and the metatarsal bones. Parasymphyseal and pubic ramus fractures often are misinterpreted as malignant lesions. Sacral, iliac, and supra-acetabular fractures often are difficult to detect.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree