Opening Round
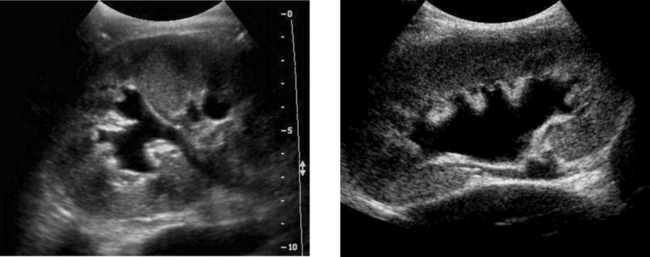
ANSWERS – CASE 1
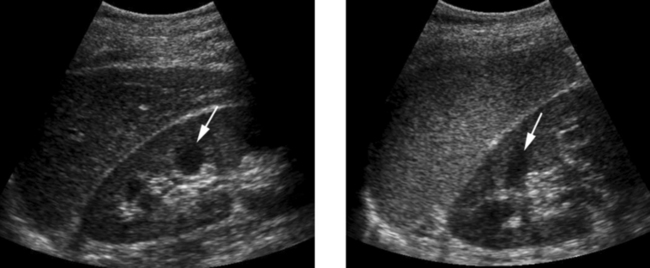
Normal Kidneys
2. The first image is the right kidney and the second image is the left kidney. The only way to tell the difference is to compare the echogenicity of the adjacent liver and spleen. The normal liver is usually similar or slightly more echogenic than the right kidney. The spleen is considerably more echogenic than the left kidney.
ANSWERS – CASE 2
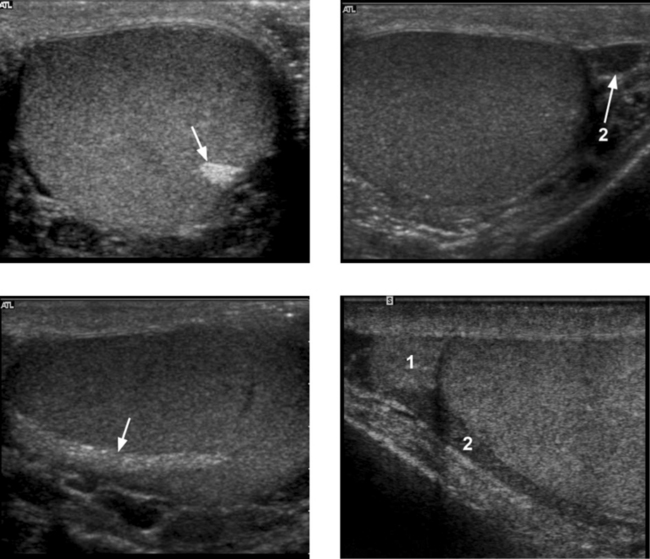
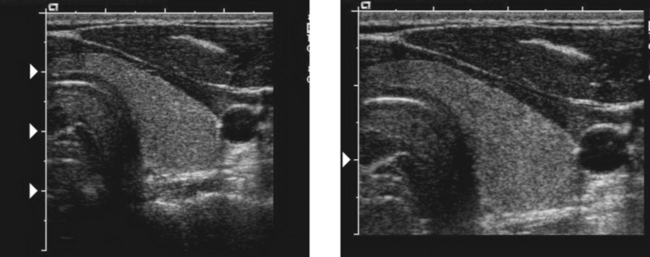
ANSWERS – CASE 3
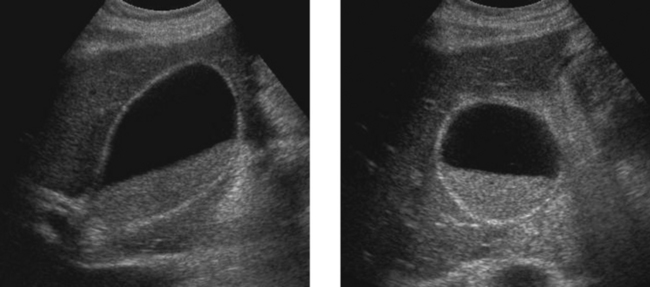
Angiomyolipoma
1. Both images show a hyperechoic mass. The second image shows slight posterior shadowing. These findings are typical of an angiomyolipoma (AML).
3. This is controversial. Since renal cell carcinoma is occasionally similarly hyperechoic, it is not unreasonable to recommend either a noncontrast CT or MRI to prove that the lesion contains fat or follow-up sonography to prove stability.
ANSWERS – CASE 4
CASE 6
Longitudinal view of the right posterior hemithorax and transverse view of the right upper quadrant obtained in different patients.
ANSWERS – CASE 5
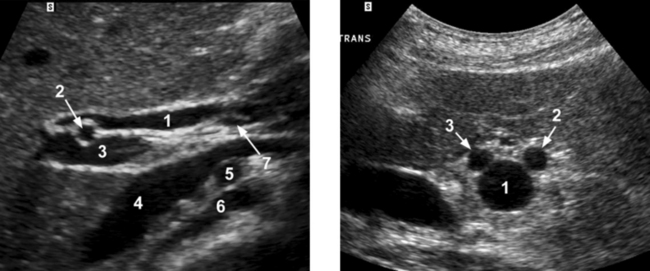
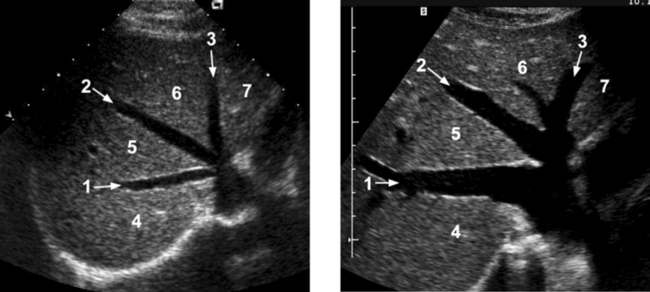
Normal Anatomy of the Common Bile Duct
1. 1 = Common hepatic duct, 2 = Right hepatic artery, 3 = Portal vein, 4 = Inferior vena cava, 5 = Right renal artery, 6 = Crus of the right diaphragm, 7 = Cystic duct insertion.
3. Bile duct diameter is measured from inner wall to inner wall. This is done to allow for better correlation with measurements taken during cholangiography.
4. The bile duct diameter is usually greatest in its mid segment (i.e., between the porta hepatis and the pancreatic head).
ANSWERS – CASE 6
CASE 7
1. What is the normal echogenic structure (arrow) shown on the first transverse view and the first longitudinal view?
2. What are the normal peritesticular structures labeled 1 and 2 on the second transverse view and the second longitudinal view?
ANSWERS – CASE 8
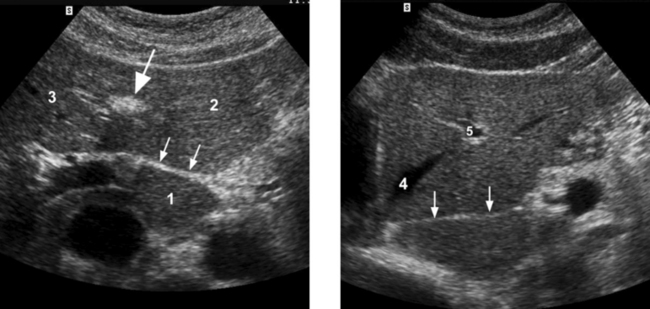
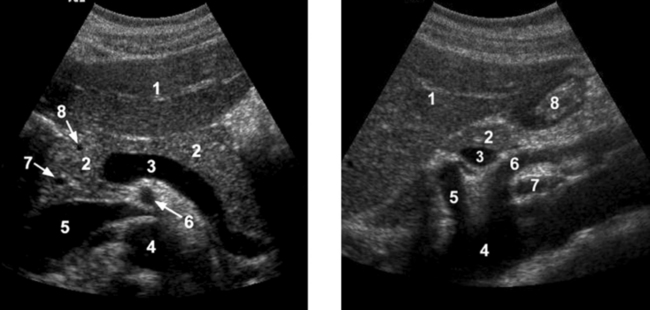
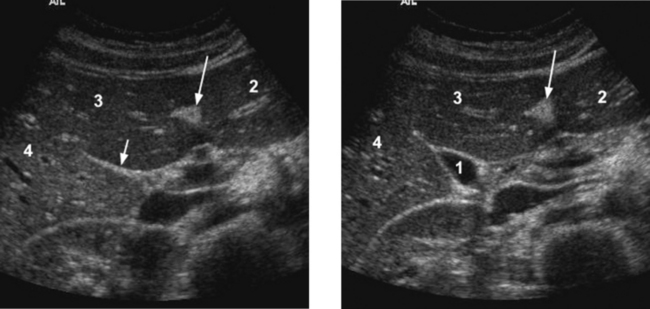
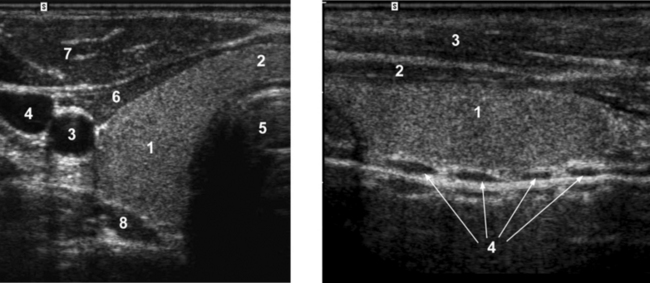
Normal Peripancreatic Anatomy
1. 1 = Left lobe liver, 2 = Pancreas, 3 = Portosplenic confluence, 4 = Aorta, 5 = Inferior vena cava (IVC), 6 = Superior mesenteric artery (SMA), 7 = Common bile duct (CBD), 8 = Gastroduodenal artery.
2. 1 = Left lobe liver, 2 = Pancreas, 3 = Splenic vein, 4 = Aorta, 5 = Celiac axis, 6 = SMA, 7 = Left renal vein, 8 = Gastric antrum.
4. The superior mesenteric vein is immediately adjacent to the head and uncinate process of the pancreas. The SMA is separated from the pancreas by a ring of echogenic fibrofatty tissue.
ANSWERS – CASE 10
ANSWERS – CASE 11
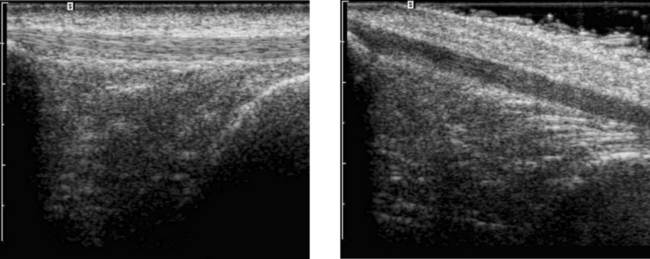
Normal Tendon Anisotropy
1. The patellar tendon is normal in both views. In fact, it is the same tendon imaged once with the long axis parallel to the transducer and again with the long axis at an angle to the transducer.
2. Decreased echogenicity in a tendon may indicate tendinitis or a partial tear, or it may be due to anisotropy.
ANSWERS – CASE 12
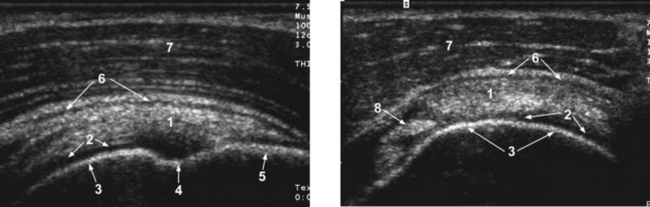
Normal Anatomy of the Shoulder
1. 1 = Rotator cuff (RC), 2 = Cartilage, 3 = Humeral head, 4 = Anatomic neck, 5 = Greater tuberosity, 6 = Subdeltoid bursa, 7 = Deltoid, 8 = Biceps tendon.
2. The rotator cuff is composed of four tendons and muscles—the subscapularis, the supraspinatus, the infraspinatus, and the teres minor.
3. The intra-articular portion of the biceps tendon separates the subscapularis and the supraspinatus.
ANSWERS – CASE 13
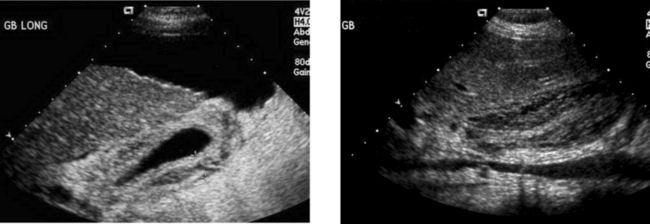
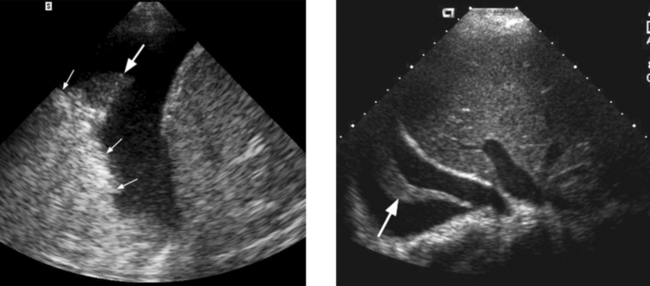
Gallbladder Wall Thickening
1. Both patients have thick gallbladder (GB) walls. The first image also shows ascites and a nodular liver consistent with cirrhosis. The second image also shows a completely contracted GB lumen.
2. The causes of a thick GB wall include heart failure, hypoproteinemia, edema-forming states, hepatitis, cirrhosis, portal hypertension, lymphatic obstruction, GB cancer, adenomyomatosis, and cholecystitis.
3. The nodularity of the liver surface in the first image is consistent with cirrhosis, and this is the cause of the GB wall thickening. The lumen of the GB is completely contracted in the second image, and this finding should raise the possibility of hepatitis.
CASE 14
3. How can you distinguish the hepatic veins and portal veins on a static gray-scale view of the liver?
ANSWERS – CASE 14
Normal Hepatic Venous Anatomy
2. The right hepatic vein separates the anterior (5) and posterior (4) segments of the right lobe. The middle hepatic vein separates the anterior segment of the right and the medial segment (6) of the left lobe. The left hepatic vein separates the left lateral (7) and the left medial segments.
3. Unlike the portal veins, the hepatic veins are not surrounded by fibrofatty tissues and therefore have much less echogenic walls. In fact, in most circumstances, the wall of the hepatic vein is not visible sonographically. The exception is when the hepatic vein is viewed with the walls perpendicular to the direction of the sound. In this situation, the wall produces a specular reflection and appears as a thin, echogenic line. This is well demonstrated in the right hepatic vein on the first image.
4. The caudate lobe drains into the vena cava via small veins that are separate from the three main hepatic veins. The caudate veins can function as collaterals in patients with Budd–Chiari syndrome.
ANSWERS – CASE 15
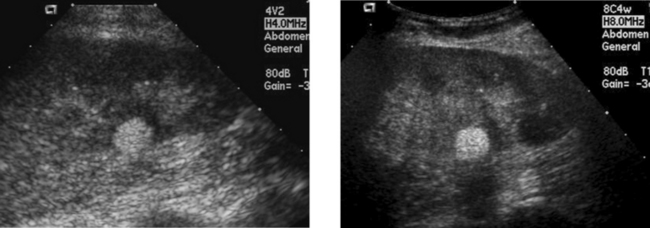
Frame Rate and Resolution
3. Frame rate can be improved by decreasing the number of focal zones, decreasing the image depth, decreasing sector width, decreasing line density, and turning off Doppler modes.
4. Resolution can be improved by using a higher frequency transducer, increasing the number of focal zones, and increasing line density.
CASE 16
3. How can the carotid artery be distinguished from the jugular vein on gray-scale scans of the neck?
CASE 17
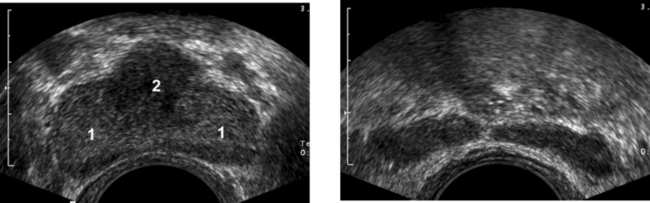
Transverse views of the prostate from a transrectal approach. The second image was obtained slightly superior to the first.
ANSWERS – CASE 16
Normal Anatomy of the Thyroid
1. 1 = Right thyroid lobe, 2 = Thyroid isthmus, 3 = Carotid, 4 = Jugular, 5 = Trachea shadow, 6 = Strap muscles, 7 = Sternocleidomastoid muscle, 8 = Longus coli muscle.
3. The carotid artery is circular, the jugular vein is oval. The carotid is more medial and deep, the jugular is more lateral and superficial. The carotid is noncompressible, the jugular is easily compressible. The diameter of the carotid is constant, the diameter of the jugular varies.
ANSWERS – CASE 17
Normal Prostate
1. Number 1 indicates the peripheral zone. Number 2 indicates the central gland, which includes the central zone and the transitional zone.
3. In young men the peripheral zone is the largest. Because of the effects of benign prostatic hypertrophy, the central gland is the largest in older men.