1 Optimizing the diagnostic information
Introduction
Image Optimization
BOX 1.1 Making the most of your equipment
The diagnostic quality of the image can be improved by:
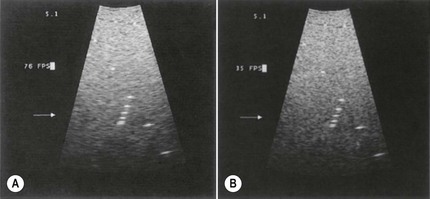
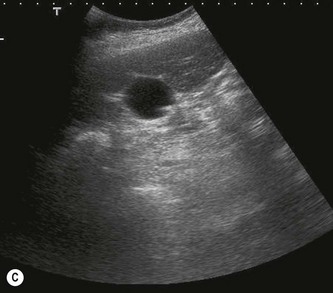

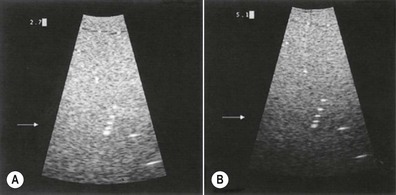
Fig. 1.2 • The effect of line density.
(A) 76 frames per second (FPS).
(B) 36 FPS – the resulting higher line density improves the image, making it sharper.
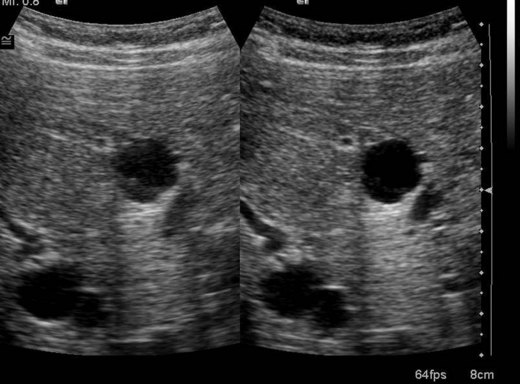
(C) The gallbladder is displayed with a low line density, as the scanning area is large.
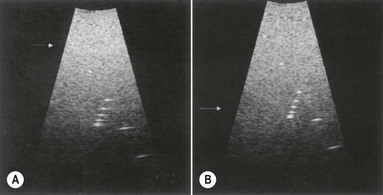


Fig. 1.3 • The effect of focal zone placement.
(A) With the focal zone in the near field, structures in the far field are poorly resolved.
(B) Correct focal zone placement improves both axial and lateral resolution of the wires.
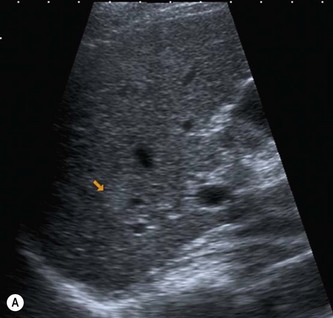

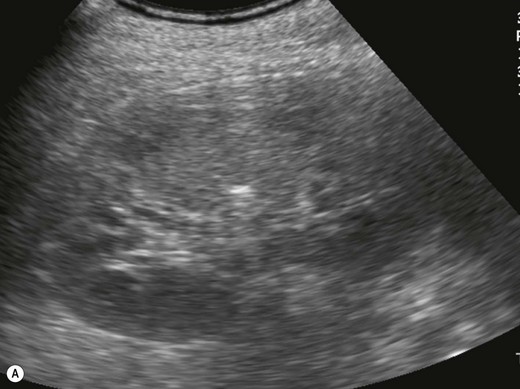
Fig. 1.4 • The effect of using post-processing options.
(A) A small nodule in a cirrhotic liver merges into the background and is difficult to detect.
The bottom line is, it is far better to have a scan performed properly on a low-tech piece of equipment by a knowledgeable and well-trained operator than to have a poorly performed scan on the latest high-tech machine (Fig. 1.6). A good operator will get the best out of even the lowliest scanning device and produce a result that will promote the correct patient management. A misleading result from a top-of-the-range scanner can be highly damaging and at best, delay the correct treatment or at worst promote incorrect management.
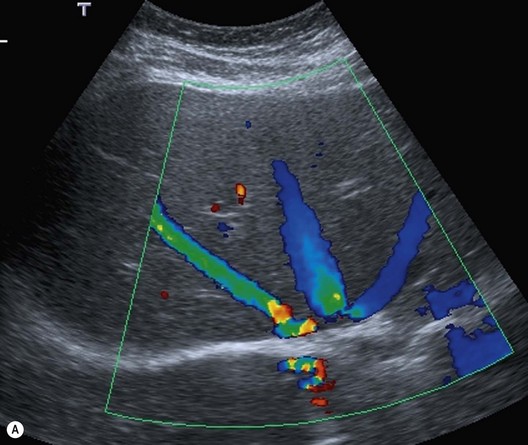
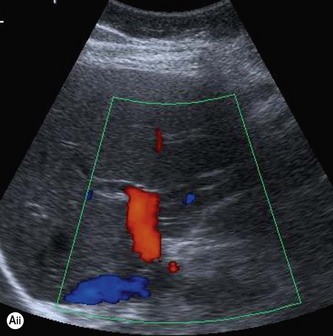
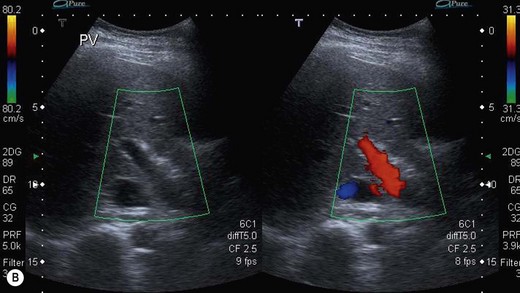
The use of doppler
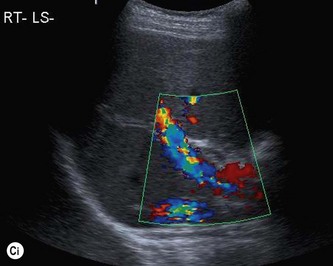
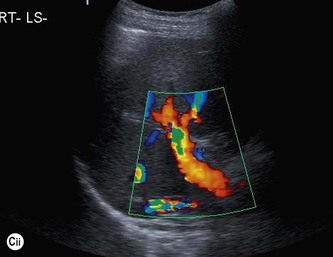
Colour Doppler is used to assess the patency and direction of flow of vessels in the abdomen, to establish the vascularity of masses or lesions and to identify vascular disturbances such as stenoses. Flow information is colour coded (usually red towards and blue away from the transducer) and superimposed on the image. This gives the operator an immediate impression of a vascular ‘map’ of the area (Fig. 1.7). This Doppler information is obtained simultaneously, often from a relatively large area of the image, at the expense of the grey-scale image quality. The extra time taken to obtain the Doppler information for each line results in a reduction in frame rate and line density, which worsens as the colour Doppler area is enlarged. It is advisable, therefore, to use a compact colour ‘box’ to maintain image quality.
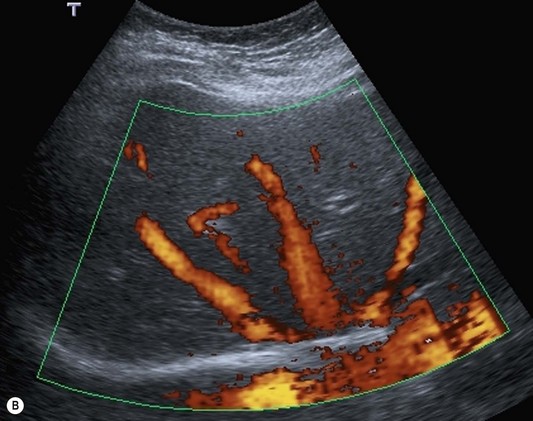
Power Doppler also superimposes Doppler information on the grey-scale image, but without any directional information. It displays only the amount of energy (Fig. 1.8). It has the advantage of a stronger signal, allowing identification of smaller vessels with lower velocity flow than colour Doppler. As it is less angle-dependent than colour Doppler it is particularly useful for vessels which run perpendicular to the beam – such as the inferior vena cava (IVC).
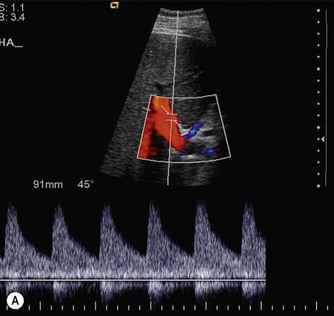
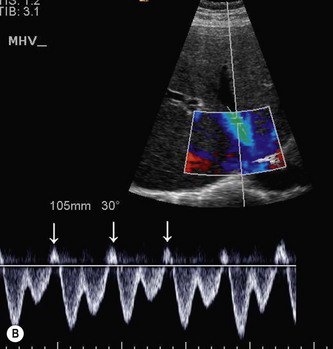
Pulsed Doppler uses pulses of Doppler from individual elements or small groups of elements within the array. This allows the operator to select a specific vessel, which has been identified on the grey-scale or colour Doppler image, from which to obtain a spectrum. This gives further information regarding the flow envelope, variance, velocity and downstream resistance of the blood flow (Fig. 1.9).
Getting the best out of doppler
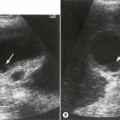
Doppler is known to produce false positive results for vessel occlusion (Fig. 1.10) and the operator must avoid the pitfalls. It is essential that the Doppler settings are sensitive enough to detect the velocity of flow in the vessel (Box 1.2). This means that the angle of insonation to the direction of flow must be as close to 0° as possible (i.e. the vessel must be flowing towards or away from the beam, not perpendicular to it), the pulse repetition frequency (PRF) must be set to detect slow flow and the Doppler gain must be turned up sufficiently.