Paget Disease
Pathophysiology
Paget disease, a relatively common bone disorder, is a chronic, progressive disturbance in bone metabolism that primarily affects older persons. It is slightly more common in men than in women (3:2), with an average age of onset between 45 and 55 years, although the disease has been known to occur in young adults. The prevalence of Paget disease varies considerably in different parts of the world, reaching its greatest incidence in Great Britain, Australia, and New Zealand.
The precise nature of Paget disease and its etiology are still debatable. Sir James Paget named the disease osteitis deformans in the belief that the basic process was infectious in origin. Other etiologies have also been proposed, such as neoplastic, vascular, endocrinologic, immunologic, traumatic, and hereditary. The hereditary etiology was supported by identification of mutations in the gene encoding sequestosome 1 (SQSTM1/p62) in patients with familial and sporadic Paget disease. Recent ultrastructural studies and the discovery of giant multinucleated osteoclasts containing microfilaments in the affected cytoplasm, as well as intranuclear inclusion bodies, suggest a viral etiology. Some investigators have obtained immunocytologic evidence identifying the particles as analogous to those from the measles group virus material. Other immunologic studies have demonstrated viral antigens in affected cells identical to those from the respiratory syncytial virus. The most recent research indicates a paramyxovirus as an etiologic factor.
Whatever the fundamental cause of Paget disease, its basic pathologic process has to do with the balance between bone resorption and appositional new bone formation. There is disordered and extremely active bone remodeling, secondary to both osteoclastic bone resorption and osteoblastic bone formation in a characteristic mosaic pattern, which is the histologic hallmark of this condition. Biochemically, the increase in osteoblastic activity is reflected in elevated levels of serum alkaline phosphatase, which can rise to extremely high values. Similarly, the increase in osteoclastic bone resorption is reflected in high urinary levels of hydroxyproline, which is formed as a result of collagen breakdown.
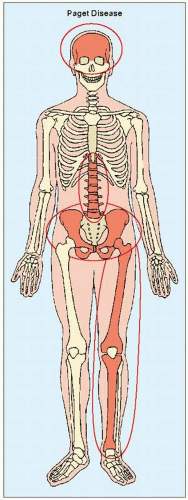
The skeletal abnormalities seen in Paget disease are frequently asymptomatic and may be an incidental finding on radiographic examination or at autopsy. When the changes are symptomatic, clinical manifestations are often related to complications of the disease, such as deformity of the long bones, warmth in the involved extremity, periosteal tenderness and bone pain, fractures, secondary osteoarthritis, neural compression, and sarcomatous degeneration. The distribution of a lesion varies from monostotic involvement to widespread disease. The following bones, in order of decreasing frequency, are most often affected: the pelvis, femur, skull, tibia, vertebrae, clavicle, humerus, and ribs (Fig. 29.1). The fibula is involved only in exceptional cases.
Radiologic Evaluation
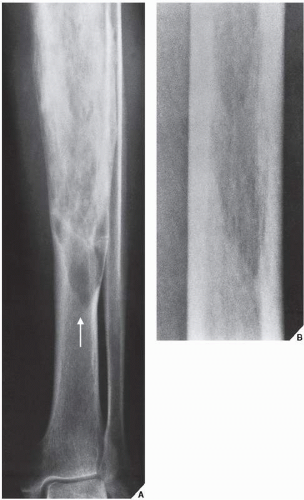
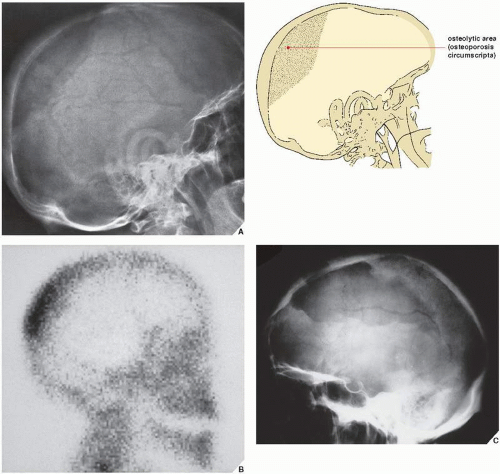
The radiographic features of Paget disease correspond to the pathologic processes in the bone and depend on the stage of the disorder. In the early phase, the osteolytic or hot phase, active bone resorption is evident as a radiolucent wedge or an elongated area with sharp borders that destroys both the cortex and cancellous bone as it advances along the shaft. The terms frequently used to describe this phenomenon are “advancing wedge,” “candle flame,” and “blade of grass” (Fig. 29.2). In flat bones such as the calvarium or the iliac bone, an area of active bone destruction known as osteoporosis circumscripta appears as a purely osteolytic lesion (Fig. 29.3). In the skull, most commonly affected sites are the frontal and occipital bones; both inner and outer calvarial tables are involved, but the former is usually more extensively affected.
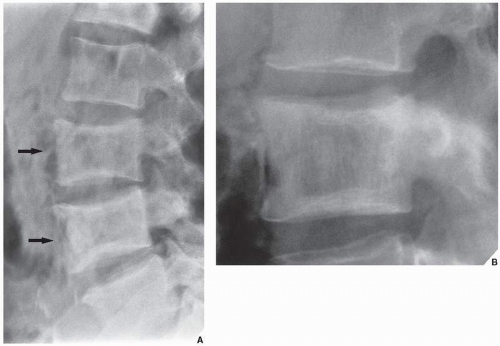
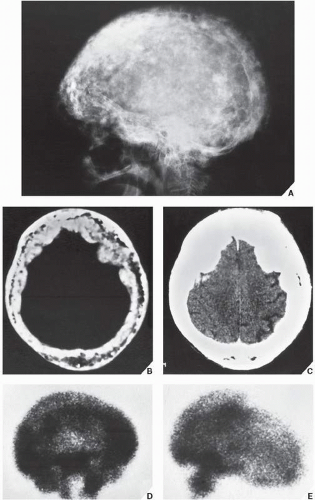
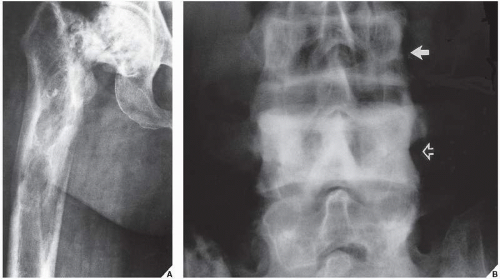
In the intermediate or mixed phase, bone destruction is accompanied by new bone formation, with the latter process tending to predominate. Bone remodeling appears radiographically as thickening of the cortex and coarse trabeculation of cancellous bone (Fig. 29.4). In the pelvis, cortical thickening and sclerosis of the iliopectineal and ischiopubic lines are present. Pubic rami and ischia may enlarge. In the spine, the thin cortex of the vertebral body, which disappears in the hot phase, is later replaced by broad, coarsely trabeculated bone, forming what appears to be a “picture frame” around the body (Fig. 29.5). In the skull, focal patchy densities with a “cotton-ball” appearance are characteristic (Fig. 29.6).
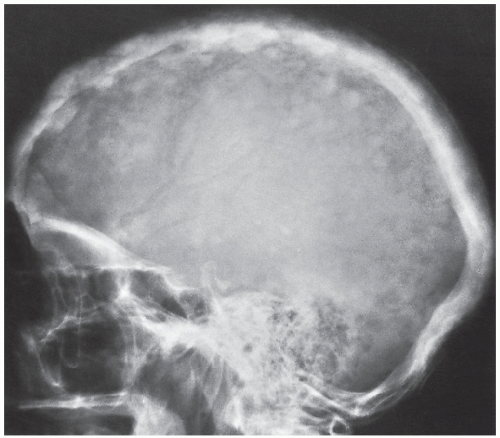
In the cool or sclerotic phase, a diffuse increase of bone density occurs together with enlargement and widening of the bone and marked cortical thickening, with blurring of the demarcation between cortex and spongiosa (Fig. 29.7). Bowing of long bones may become a striking feature (Fig. 29.8). Similar changes are observed in the skull, where obliteration of the diploic space is also a typical feature (Fig. 29.9).
It is important to remember that, since in the long bones Paget disease starts at one articular end and advances to the other, all three phases of the disorder may coexist in the same bone (Fig. 29.10A). Likewise, different phases may coexist in the flat bones or in the spine (Fig. 29.10B).
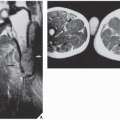
Computed tomography (CT) may demonstrate characteristic features of Paget disease (Fig. 29.11), although it is rarely required. Magnetic resonance imaging (MRI) is occasionally employed to demonstrate cortical and intramedullary involvement better, and to exclude (or confirm) extension of the process into the soft tissues. In general, the pagetic bone exhibits heterogeneous signal intensity. On T1-weighted sequences, intermediate-to-low signal intensity is usually noted. On T2 weighting, the signal may be high, intermediate, or low, depending on the stage of the disease and degree of fibrosis and sclerosis (Figs. 29.12 and 29.13).
Differential Diagnosis
Several conditions may mimic Paget disease, while the disease itself may be mistaken for other pathologic processes; for example, involvement of a single bone can be mistaken for monostotic fibrous dysplasia, and a uniform increase in osseous density may mimic lymphoma or metastatic cancer. The rugger-jersey appearance of the spine in secondary hyperparathyroidism may resemble Paget vertebra (see Fig. 28.8). Vertebral hemangioma also looks very much like Paget vertebra on a radiograph, except that the vertebral body is not enlarged and the vertebral end plates are well outlined (see Fig. 20.46). However, the condition that bears the most striking resembalance to Paget disease is familial idiopathic hyperphosphatasia, also called “juvenile Paget disease” (see Figs. 30.1 and 30.2). In this condition, unlike Paget disease, the articular ends of the bone may not be affected.
Complications
Pathologic Fractures
Of the numerous complications observed in patients with Paget disease, the most common are pathologic fractures in the long bones. They may resemble partial or incomplete stress fractures, appearing radiographically as multiple short horizontal radiolucent lines on the convex aspect of the cortex (Fig. 29.14). True complete fractures are referred to as “banana-type” because of the horizontal direction of the fracture line as it traverses the affected bone (Fig. 29.15), and they have also been compared with crushed rotten wood or chalk. Fractures are more likely to occur during the osteolytic or hot phase, and they are frequently the main presenting manifestation of Paget disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree