Parathyroid Scintigraphy
Patrick M. Colletti
LEARNING OBJECTIVES
1. Explain the basic principles of hyperparathyroidism.
2. Describe the methods of parathyroid scintigraphy.
3. Compare the results of five different parathyroid scintigraphy techniques.
BACKGROUND
Primary hyperparathyroidism (pHPT) is associated with one or more abnormally active parathyroid gland. Secondary hyperparathyroidism (sHPT) is associated with chronic hypocalcemia results in reactive overproduction of parathyroid hormone (PTH). sHPT is often directly related to chronic renal failure. Tertiary hyperparathyroidism (tHPT) is the result of untreated sHPT, with continuously elevated PTH levels.
Parathyroidectomy for hyperparathyroidism is typically planned on the basis of medical imaging and performed via a scope or small incision with intraoperative PTH (IOPTH) monitoring. Given the biological half-life of PTH of 5 min, successful excision of target parathyroid lesions should result in a 50% or greater reduction in IOPTH compared with preoperative baseline levels at 5 min and a normal or near-normal IOPTH level at 10 min post-excision (1,2,3).
There are several effective methods for locating parathyroid adenoma and parathyroid hyperplastic glands, including ultrasound, 4D contrast-enhanced computed tomography (CT), selective angiography with venous sampling, and radionuclide parathyroid imaging. This chapter presents the methods and results of parathyroid scintigraphy.
Parathyroid scintigraphy
While there are alternative radiopharmaceuticals that may be used for parathyroid localization, including 11C-choline positron emission tomography (PET)/CT (4), 99mTc sestamibi is reliable and effective as applied in a variety of techniques (5,6,7,8,9,10):
99mTc sestamibi alone with delayed views, with or without pinhole imaging, single photon emission computed tomography (SPECT), or SPECT/CT.
99mTc sestamibi with subtraction of the 99mTc-pertechnetate or 123I-labeled thyroid with or without pinhole imaging, SPECT, or SPECT/CT.
Table 5.1 compares the clinical performance of these techniques [11]. Parathyroid scintigraphy detects 50% to 75% of parathyroid adenomas.
Interpretation may be as simple as visually comparing pertechnetate images with sestamibi images, looking for differences on the sestamibi images not seen on the pertechnetate images. In general, delayed 99mTc sestamibi images will increase the contrast between parathyroid adenomas and thyroid tissue, as the thyroid activity washes out faster than parathyroid adenomas.
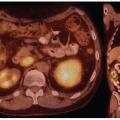
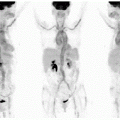
Figure 5.1 demonstrates differences in activity seen on 99mTc sestamibi as compared with 99mTc-pertechnetate images along with differential thyroid washout.
Figure 5.2 demonstrates the advantage of SPECT/CT for the 3D location of mediastinal parathyroid adenoma.
Figure 5.3 shows how sestamibi and pertechnetate comparison with differential washout demonstrates all four hyperplastic parathyroid glands in a patient with renal failure.
Figure 5.4 presents examples from patients with secondary and tertiary hyperparathyroidism.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree