Part 8 Bone
Case 77
Clinical History
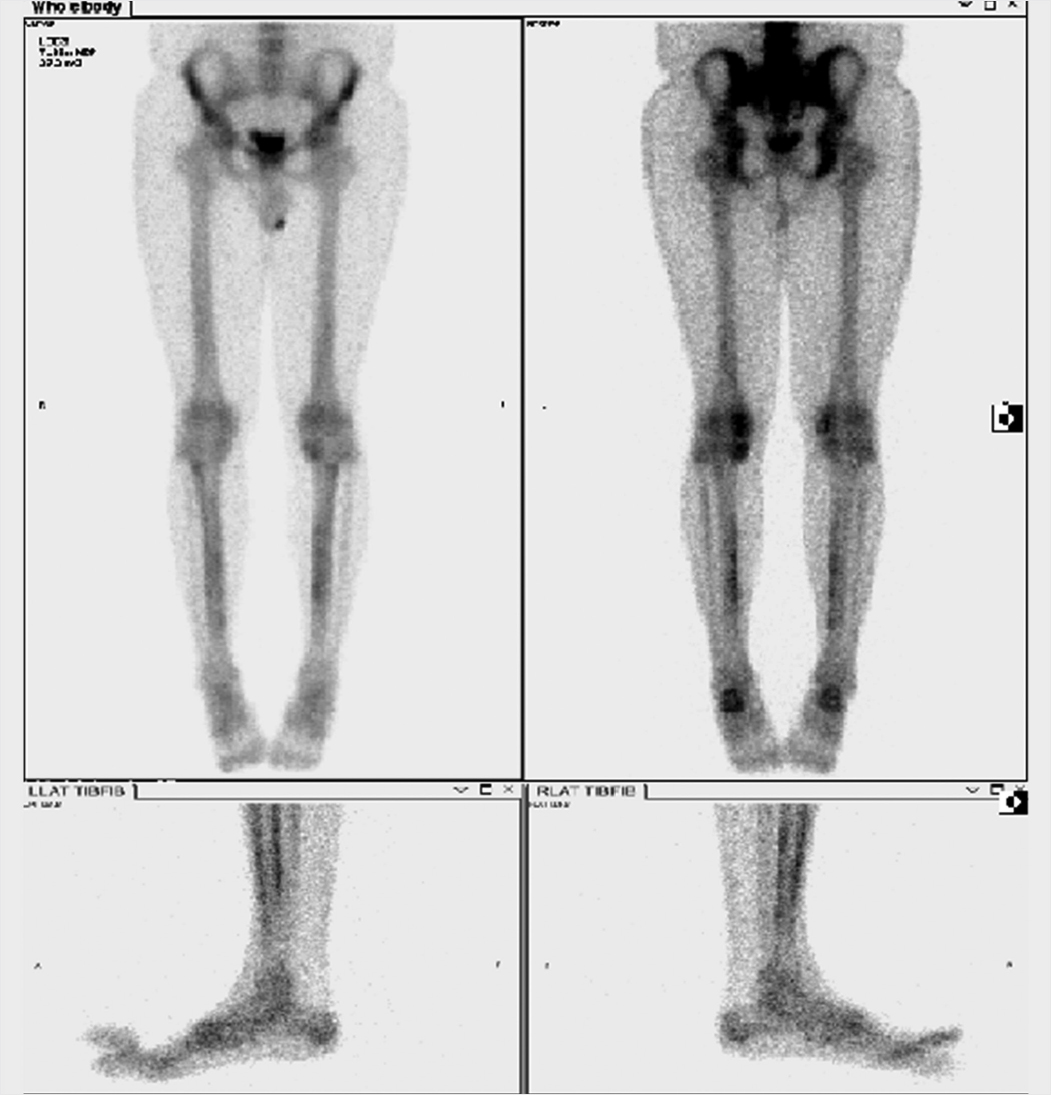
23-year-old male with bilateral shin pain for over a year, symptoms worsening to lower tibia (▶Fig. 77.1).
Key Finding
Symmetric “tram-track” cortical uptake of long bones
Top 3 Differential Diagnoses
Hypertrophic osteoarthropathy (HOA). Secondary HOA is a clinical syndrome of symptomatic periostitis of long bones due to various neoplastic and non-neoplastic pulmonary and extrapulmonary disorders. Common pulmonary causes include bronchogenic carcinoma, fibrous tumor of the pleura, mesothelioma, and chronic pulmonary infection/inflammation; as a result, a chest radiograph should be obtained in patients with scintigraphic evidence of HOA. Extrapulmonary etiologies include inflammatory bowel disease, cyanotic congenital heart disease, and thyroid acropachy. The exact pathophysiology of HOA remains unclear; however, vasoactive agents and hormones secreted by tumors and other inflammatory/infectious processes have been implicated. Scintigraphic findings of bilateral symmetric upper and lower extremity parallel cortical activity in a “tram-track” configuration often precede plain film evidence of undulating periosteal proliferation. There may be associated increased activity within the scapula, mandible/maxilla, and periarticular regions. Patients usually report painful swelling of the affected limb, stiff joints, and demonstrate digital clubbing on physical exam. The radiographic and scintigraphic findings usually resolve after treatment of the underlying disease.
Shin/quadriceps splints. Severe bilateral shin and quadriceps splints may produce increased parallel cortical activity within the lower extremities of physically active patients with lower leg pain related to exertion of overuse. Shin splints (medial tibial stress syndrome) result in unilateral or bilateral posteromedial tibial cortical periostitis. These patients present with dull aching leg pain. Unlike stress fractures that appear as focal regions of increased uptake on all three phases of a bone scan, splints are generalized linear or longitudinal activity along the diaphysis, usually the middle third, detected on delayed phase imaging. While stress fractures may coexist in a patient with shin or quadriceps splints, there has been no evidence to suggest a progression of splints to stress fracture.
Chronic venous stasis. Chronic venous insufficiency can lead to soft-tissue edema, associated skin changes (including stasis ulcers), and thick undulating or nodular periosteal proliferation of the affected extremity due to local hypoxia. Physical examination can help differentiate this entity from other causes of increased parallel long bone activity within an extremity by noting overlying skin changes. In the setting of cellulitis and chronic venous stasis, it may be difficult to exclude superimposed osteomyelitis.
Diagnosis
Bilateral shin splints.
✓ Pearls
Benign and malignant etiologies can lead to HOA; obtain a chest X-ray to evaluate for underlying tumor.
Shin and quadriceps splints are common in athletes and result in cortical periostitis with linear activity.
Chronic venous stasis may lead to undulating periosteal proliferation due to hypoxia.
Suggested Readings
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003; 23(2):341–358 Ali A, Tetalman MR, Fordham EW, et al. Distribution of hypertrophic pulmonary osteoarthropathy. AJR Am J Roentgenol. 1980; 134(4):771–780 Rana RS, Wu JS, Eisenberg RL. Periosteal reaction. AJR Am J Roentgenol. 2009; 193(4):W259–72Case 78

Key Finding
Superscan
Top 3 Differential Diagnoses
Metastatic disease. A superscan refers to increased skeletal uptake on bone scan with decreased or absent renal and soft-tissue activity. Diffuse osseous metastatic disease is the most common cause of a superscan, most commonly metastatic prostate cancer. With metastatic disease, the skeletal activity is typically inhomogeneous and centered primarily within the axial and proximal appendicular skeleton. Distinct metastatic foci may be discernible.
Metabolic bone disease. Although somewhat varied in scintigraphic appearance, metabolic diseases, such as renal osteodystrophy, hyperparathyroidism, and osteomalacia, may result in generalized increased activity in the skeleton relative to the kidneys and soft tissues. Features that suggest metabolic disease include uniform distribution of activity, involvement of the appendicular skeleton, and disproportionate increased calvarial uptake. The osseous manifestations of renal osteodystrophy result from altered vitamin D metabolism and secondary hyperparathyroidism. This diagnosis is suggested on bone scan by prominent activity along the costochondral junctions, involvement of distal long bones, “railroad tracking” and bowing of the femurs, and sternal activity. Pseudofractures may be seen in the setting of osteomalacia.
Paget’s disease. Intense activity and expansion of bones are characteristic of Paget’s disease, most commonly involving the pelvis, femora, spine, and skull. When multifocal or widespread, concentration of radiopharmaceutical in the skeletal lesions and increase in target-to-soft-tissue ratio may result in an apparent superscan.
Additional Diagnostic Consideration
Myeloproliferative/marrow infiltrative disorder: A superscan from myeloproliferative diseases, such as lymphoma, mastocytosis, and myelofibrosis, usually manifests as uniform and homogeneous radiotracer uptake within both the axial and appendicular skeleton, similar to a metabolic superscan. Appropriate history and laboratory values aid in distinguishing between myeloproliferative/marrow infiltrative disorders and metabolic disease.
Diagnosis
Diffuse osteoblastic metastatic disease.
✓ Pearls
Superscan refers to increased skeletal with decreased or absent renal and soft-tissue activity on bone scan.
Metastatic disease is the most common cause of a superscan and typically involves the axial skeleton.
Metabolic bone disease involves both the axial and appendicular skeleton and is usually homogeneous.
Paget’s disease may result in a superscan when widespread.
Suggested Readings
Buckley O, O’Keeffe S, Geoghegan T, et al. 99 mTc bone scintigraphy superscans: a review. Nucl Med Commun. 2007; 28(7):521–527 Cheng TH, Holman BL. Increased skeletal:renal uptake ratio: etiology and characteristics. Radiology. 1980; 136(2):455–459 Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003; 23(2):341–358Case 79

Clinical History
78-year-old male with metastatic prostate cancer prior to Xofigo therapy (▶Fig. 79.1).
Key Finding
Increased activity and osseous expansion in the pelvis
Top 2 Differential Diagnoses in an Adult
Paget’s disease. This condition most commonly occurs in middle-aged to older men. The cause is unknown. On bone scans, Paget’s disease exhibits increased activity, often with apparent expansion. Distribution is monostotic in 10 to 35% cases most commonly affecting the pelvis, spine, sacrum, femur, and cranium. Osteoporosis circumscripta, a classic lytic lesion of the skull, will have uptake at the margins. Paget’s disease progresses from one end of a long bone to the other with a sharp demarcation from the involved to the uninvolved portion, rendering the classic “blade of grass” appearance. Bone scan uptake is typically increased during all three phases of the disease (lytic, mixed, and sclerotic). Bone scan is more sensitive than radiography, and useful for identifying polyostotic disease. Sarcomatous degeneration may initially result in increasing focal activity, but may later appear photopenic due to lesional necrosis.
Metastases. Bone scan is the most useful imaging modality to search for osteoblastic metastatic disease. Although usually multifocal, metastases may occasionally be monostotic. The axial skeleton is most commonly involved. Sclerotic metastases are most likely due to prostate cancer in men and breast cancer in women. Metastatic disease typically presents as multifocal regions of increased activity on bone scan, with the activity often from the body’s reaction to the tumor. The involved bone may be enlarged secondary to tumor burden. Lesions may demonstrate increased activity within the first 6 months after chemotherapy, referred to as the “flare phenomenon,” as a result of a healing osteoblastic response. Increasing activity after 6 months should be considered progression of the disease.
Top 3 Differential Diagnoses in a Child
Ewing’s sarcoma. It is the second most common primary bone tumor in children (after osteosarcoma), usually involving the pelvis or femur. Patients typically present with progressive pain. Bone scans demonstrate increased activity and bone expansion may also be seen. Osseous metastases occur in approximately half of patients; therefore, follow-up imaging is warranted to evaluate for disease progression.
Lymphoma. Lymphoma can mimic Ewing’s sarcoma clinically and radiographically but has a more favorable prognosis. Increased activity and bony expansion may be seen on bone scan. The pelvis is commonly involved. Biopsy is warranted to confirm the diagnosis but should be coordinated with the pediatric surgeon as the tract used for biopsy may alter the surgical approach.
Fibrous dysplasia (FD). This condition may be monostotic or polyostotic (McCune–Albright syndrome). The lesions may be lucent having a ground glass matrix or may be sclerotic. Bony expansion is common. Increased uptake is noted in involved bones. Common locations include long bones, pelvis, craniofacial bones, spine, and ribs.
Diagnosis
Metastatic prostate cancer.
✓ Pearls
Paget’s disease most commonly affects the pelvis; bone scan may help identify sarcomatous degeneration.
Paget’s disease and FD can be monostotic or polyostotic.
Correlation with anatomic imaging can be paramount in distinguishing benign from malignant disease.
Suggested Readings
Abdelrazek S, Szumowski P, Rogowski F, Kociura-Sawicka A, Mojsak M, Szorc M. Bone scan in metabolic bone diseases. Review. Nucl Med Rev Cent East Eur. 2012; 15(2):124–131 Kumar AA, Kumar P, Prakash M, Tewari V, Sahni H, Dash A. Paget’s disease diagnosed on bone scintigraphy: Case report and literature review. Indian J Nucl Med. 2013; 28(2):121–123 Orzel JA, Sawaf NW, Richardson ML. Lymphoma of the skeleton: scintigraphic evaluation. AJR Am J Roentgenol. 1988; 150(5):1095–1099Case 80

Clinical History
67-year-old female with history of open reduction and internal fixation (ORIF) of the right ankle presenting with right lateral ankle cellulitis, refractory to outpatient treatment, swelling and tenderness to palpation, with healed scab over later malleolus (▶Fig. 80.1).
Key Finding
Three-phase positive bone scan
Top 3 Differential Diagnoses
Trauma. A TPBS involves dynamic flow imaging for the first minute after radiopharmaceutical injection, static blood pool imaging for next few minutes, and subsequent static delayed imaging at 2 to 4 hours. Although a TPBS is classically performed for determination of osseous infection, increased uptake on all three phases is a nonspecific finding and can be seen in setting of acute fracture or recent surgery. Approximately 80% of fractures demonstrate increased activity within 24 hours and over 95% of fractures demonstrate increased activity by 3 days. A healed extremity fracture may have persistent focal increased activity on the delayed phase of the bone scan for over a year.
Osteomyelitis. TPBS not only has a high sensitivity and negative predictive value for acute osteomyelitis, but it may also detect abnormalities 1 to 2 weeks earlier than radiographic manifestations. False-negative bone scans, however, are often seen in the setting of disrupted blood supply and abscess formation, especially in neonates and infants with hematogenously acquired osteomyelitis. Specificity is decreased in the setting of recent surgery, trauma, or orthopedic hardware. Dual-isotope imaging with indium-111-labeled white blood cells (In-111 WBC; for infection) and technetium-99m sulfur colloid (Tc-99m SC; for normal bone marrow mapping) can aide in assessment of osteomyelitis. Focal uptake on an In-111 WBC scan, which is spatially discordant from Tc-99m SC bone marrow scan, is suggestive of infection.
Bone tumor. Primary or secondary malignant bone tumors may demonstrate increased activity on all three phases. Although most benign osseous neoplasms will not demonstrate increased flow or blood pool activity, osteoid osteomas (OO) contain a three-phase positive nidus with a “target sign” on delayed imaging.
Additional Diagnostic Consideration
Complex regional pain syndrome: This condition typically occurs after trauma or surgery and is characterized by pain, swelling, and vasomotor instability out of proportion to the degree of injury. Periarticular swelling and osteopenia may be seen on plain radiographs. Early or acute complex regional pain syndrome (CRPS) classically demonstrates unilateral increased flow and blood pool activity with periarticular increased radiotracer activity on delayed images. This classic pattern is only seen in two-thirds of affected patients. The flow and blood pool activity may normalize in chronic or long-standing CRPS. Interestingly, CRPS in children commonly demonstrates normal or even decreased activity (so-called cold CRPS).
Diagnosis
Reactive bone marrow post ORIF.
✓ Pearls
Flow, blood pool, and delayed imaging at 2 to 4 hours make up a TPBS.
Three-phase positive scans may be seen with acute fractures, osteomyelitis, OOs, and CRPS.
In-111 WBC scan with Tc-99m SC scan is highly specific for hardware osteomyelitis.
CRPS presents with periarticular osteopenia and corresponding increased activity on TPBS.
Suggested Readings
Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003; 23(2):341–358 Kozin F, Soin JS, Ryan LM, Carrera GF, Wortmann RL. Bone scintigraphy in the reflex sympathetic dystrophy syndrome. Radiology. 1981; 138(2):437–443Case 81

Key Finding
Focal increased activity within an extremity on bone scan
Top 3 Differential Diagnoses
Stress fracture. Tc-99m hydroxy diphosphonate (HDP) or methylene diphosphonate (MDP) localizes to areas of increased osteoblastic activity. Over 80% of fractures are detected within the first 24 hours and nearly 95% by 72 hours. Stress fractures are classified as either fatigue fractures, which are fractures in normal bone exposed to abnormal stress, or insufficiency fractures, which are fractures in abnormal bone exposed to normal stress. Repetitive stress can lead to microfractures which may progress to overt fracture if unrecognized. Typical sites for fatigue-type stress fractures include the tibia, fibula, medial femoral neck, inferior pubic ramus, metatarsals, and calcaneus. Stress fractures are seen as intense focal, fusiform activity on bone scan, typically greater in intensity than the anterior superior iliac spine on the anterior image or sacroiliac joints on the posterior image. Stress fractures within long bones can be graded based on their extent of corticomedullary involvement. Single-photon emission computed tomography (SPECT) should be performed if concern is for femoral neck stress fracture as up to 50% can be missed on planar images. Treatment includes rest and modification of activity.
Osteomyelitis. This disease may occur due to extension from adjacent soft tissue cellulitis, direct inoculation from open wound, or by hematogenous spread. Three-phase bone scan (TPBS) has high negative predictive value for osteomyelitis. Cellulitis demonstrates hyperemia and soft-tissue uptake on early phases but no abnormal bone activity on delayed imaging. Osteomyelitis, in contrast, is positive on all three phases. Specificity for osteomyelitis is lower in the setting of recent trauma, surgery, or orthopedic hardware, necessitating correlation with indium-111-labeled white blood cells (In-111 WBC) and Tc-99m SC scans.
Neoplasm (benign and malignant). Primary bone malignancies (e.g., osteosarcoma and Ewing’s sarcoma) and osteoblastic metastases generally demonstrate avid uptake on bone scan. Sensitivity is lower for predominantly lytic lesions (multiple myeloma, renal cell carcinoma, and thyroid cancer). Benign bone tumors have a variable appearance on bone scan but generally do not demonstrate significant hyperemia with the exception of osteoid osteoma (OO). Osteoid osteoma has focal intense uptake within a central vascular nidus with comparatively less uptake in the surrounding reactive sclerosis, described as the “double-density” or “target” sign. Clinically, patients present with dull, achy night pain that is relieved by nonsteroidal anti-inflammatory drugs. Solitary bone cysts are generally photopenic, while bone islands and osseous hemangiomas rarely are detectable on bone scan. Benign, uncomplicated exostoses and enchondromas are usually warm on bone scan.
Additional Diagnostic Consideration
Fibrous dysplasia (FD): It is a congenital, nonhereditary skeletal dysplasia that generally demonstrates intense uptake on bone scan. Common areas of involvement include the ribs, tibia, femur, and craniofacial bones. The skeletal lesions demonstrate the classic expanded ground glass matrix on plain film. Bone scan is helpful in detecting polyostotic involvement.
Diagnosis
Completed stress fracture.
✓ Pearls
Stress fractures (fatigue or insufficiency) present as focal uptake in characteristic locations.
OO is positive on all three phases of bone scan with a characteristic “target” sign.
Multifocal uptake may be seen with metastases, osteomyelitis, insufficiency fractures, FD, or Paget’s disease.
Osseous metastases are generally seen within the axial rather than appendicular skeleton.
Suggested Readings
Bryant LR, Song WS, Banks KP, Bui-Mansfield LT, Bradley YC. Comparison of planar scintigraphy alone and with SPECT for the initial evaluation of femoral neck stress fracture. AJR Am J Roentgenol. 2008; 191(4):1010–1015 Love C, Din AS, Tomas MB, Kalapparambath TP, Palestro CJ. Radionuclide bone imaging: an illustrative review. Radiographics. 2003; 23(2):341–358Case 82

Clinical History
43-year-old male with unilateral café-au-lait spots and multiple lytic fractures (▶Fig. 82.1).
Key Finding
Regionally increased uptake on bone scintigraphy
Top 3 Differential Diagnoses
Fibrous dysplasia (FD). One-fourth of FDs are polyostotic. Three-fourths are monostotic and most commonly involve the rib, proximal femur, tibia, and skull. Coxa vara angulation (“shepherd’s crook”) can be seen in the proximal femur as well as anterior bowing of the tibia (“saber shin”). Tc-99m medronic acid (MDP) bone scintigraphy demonstrates increased radiotracer deposition where there is increased osseous metabolism, not always contiguous. Classic radiographic findings include a well-circumscribed lucent lesion within the metaphysis or diaphysis, often with a ground glass matrix and fusiform enlargement. Bowing deformities may require surgical correction.
Paget’s disease. This disease evolves through three phases: early lytic, mixed, and sclerotic. A sharply demarcated line of osteolysis advances from the epiphysis toward the diaphysis in a contiguous manner. Bone scan will show increased uptake in all three phases, particularly in active disease.
Osteosarcoma. This is a bone-forming malignant neoplasm that demonstrates increased radiotracer deposition on bone scintigraphy. Primary osteosarcoma usually presents in the metadiaphysis of long bones, secondary more frequently involving flat bones. Primary osteosarcoma is known to have “skip” lesions within the primary affected bone which can cause uptake similar to FD and Paget’s disease on scintigraphy.
Additional Diagnostic Consideration
Complex regional pain syndrome: CRPS most frequently presents as regional polyostotic periarticular increased radiotracer deposition on bone scintigraphy. It will involve most, if not all, of the osseous structures in the affected region. CRPS can be photopenic on bone scan, known as “cold CRPS,” more commonly seen in pediatric patients.
Diagnosis
Polyostotic FD.
✓ Pearls
FD rarely undergoes malignant change and often are not surgically corrected.
Bone scan is better for staging of Paget’s as radiography may underestimate disease.
Osteosarcoma can present with “skip” lesions resulting in regional uptake on bone scan.
Regional, polyostotic, and periarticular uptake is seen with CRPS which is hot on all three phases.
Suggested Readings
Kwon HW, Paeng JC, Nahm FS, et al. Diagnostic performance of three-phase bone scan for complex regional pain syndrome type 1 with optimally modified image criteria. Nucl Med Mol Imaging. 2011; 45(4):261–267 Rubin AN, Byrns K, Zhou D, Freedman L. Fibrous dysplasia of the rib: AIRP best cases in radiologic-pathologic correlation. Radiographics. 2015; 35(7):2049–2052 Theodorou DJ, Theodorou SJ, Kakitsubata Y. Imaging of Paget disease of bone and its musculoskeletal complications: review. AJR Am J Roentgenol. 2011; 196(6, Suppl):S64–S75Case 83

Key Finding
Focal soft-tissue uptake on bone scintigraphy
Top 3 Differential Diagnoses
Heterotopic ossification (myositis ossificans). Heterotopic ossification (HO), or bone formation where bone is not usually present, can be acquired or hereditary. Acquired HO is much more common and results from transformation of mesenchymal cells into osteogenic cells. It is usually seen after fracture, direct muscular trauma, surgery, closed head injury, or spinal cord injury. Clinical presentation is not specific and can include pain, fever, swelling, and erythema, with eventual loss of range of motion. If biopsied early, before the heterotopic bone has matured, pathology will show immature bone and fibrous proliferation and may be confused for osteosarcoma. Conventional radiography will initially show a nondescript calcific density that will evolve to mature bone on subsequent images. Three-phase bone scintigraphy is the most sensitive exam for early HO, with changes seen 4 to 6 weeks prior to the initial mineralization seen on radiographs. Initially, just the flow and blood pool images will be positive with delayed uptake seen around 1 week later. Bone scan will eventually show progressive decrease in deposition, with return to baseline after about 1 year.
Soft-tissue calcification. The uptake mechanism for the phosphate analogue bone tracers, Tc-99m medronic acid (MDP) and Tc-99m HDP, involves chemisorption primarily into the hydroxyapatite phase of bone formation. However, some of the radiotracer will be taken up by amorphous calcification. Focal/regional extraosseous uptake can be seen due to altered biodistribution from changed vascularity, extraosseous calcification (dystrophic, metastatic, or tumoral), neoplasms, or an inflammatory process. Correlation with anatomic imaging and clinical history will be helpful. Metabolic abnormalities will result in more diffuse uptake.
Nonvenous injection. Intra-arterial injection of radiotracer often produces a characteristic “glove” distribution pattern. Extravasation produces a focal area of radiotracer deposition at the injection site. With extravasation, there may also be focal radiotracer accumulation in the closest lymph node bed, often the axilla, mimicking focal soft-tissue uptake. Single-photon emission computed tomography (SPECT)/CT imaging can play an important role in establishing this as the etiology.
Additional Diagnostic Consideration
Breast tissue involvement: There can be focal radiotracer uptake within the postpubertal, lactating, or nonlactating breast tissue. It can be a finding in the setting of mastitis. It can also be from metastases and primary breast malignancies.
Diagnosis
Nonvenous injection.
✓ Pearls
Serial bone scans of HO demonstrate decreasing radiotracer deposition, paralleling injury resolution.
Tumoral calcinosis is often associated with articular bursa along extensor surfaces.
Nonvenous injection of radiotracer produces localized uptake often characteristic in nature.
Clinical history and anatomic imaging are helpful in the setting of extraosseous bone scan uptake.
Suggested Readings
Olsen KM, Chew FS. Tumoral calcinosis: pearls, polemics, and alternative possibilities. Radiographics. 2006; 26(3):871–885 Shehab D, Elgazzar AH, Collier BD. Heterotopic ossification. J Nucl Med. 2002; 43(3):346–353 Wale DJ, Wong KK, Savas H, Kandathil A, Piert M, Brown RK. Extraosseous findings on bone scintigraphy using fusion SPECT/CT and correlative imaging. AJR Am J Roentgenol. 2015; 205(1):160–172Case 84

Key Finding
Focal axial spine uptake on bone scintigraphy
Top 3 Differential Diagnoses
Degenerative joint disease. Axial spine degenerative joint disease is pervasive in older generations. However, it most often presents with metabolic activity juxtaposed with the vertebral body in a periarticular distribution. Anatomic imaging facilitates interpretation and differentiation of osteophytes.
Metastatic disease. Metastatic disease most often involves the vertebral body proper, the pedicle, and/or the posterior elements. It rarely involves the articular surfaces. While metastatic disease is most commonly multifocal, a single hot lesion in the spine on bone scan in a patient with a known malignancy is still likely to be a metastasis.
Spondylolysis. It is often associated with focal low back pain that worsens with activity. It is often seen in athletic adolescents. Spondylolysis is the result of an ongoing stress reaction. As such, there can be bone scintigraphy findings before anatomic changes are noticed. Bone scan uptake indicates symptomatic spondylolysis with active healing that may benefit from immobilization. Bone scan may also show uptake in the contralateral pars interarticularis raising concern for impending fracture.
Additional Diagnostic Considerations
Discitis: Bone scan can be used for initial nuclear medicine evaluation for discitis/osteomyelitis, and it should demonstrate uptake surrounding a disc space. Gallium-67 scintigraphy or flourine-18 FDG PET imaging is preferred over tagged WBC imaging for confirmation due to the high false-negative rate with WBC imaging in the spine.
Primary bone tumor: Several primary bone lesions can be located within the axial spine and demonstrate increased uptake on bone scan. These include OO, osteoblastoma, chondroblastoma (CB), malignant fibrous histiocytoma, Ewing’s sarcoma, lymphoma, chordoma, giant cell tumor (GCT), and hemangioma among others. Hemangiomas are commonly encountered, usually incidentally discovered on anatomic imaging and indistinguishable on bone scan, but may present as focally increased or focally decreased radiotracer deposition.
Diagnosis
Vertebral hemangioma.
✓ Pearls
Degenerative changes in the axial spine have periarticular hot spots.
Metastatic disease is most often located eccentrically in the vertebral body or pedicle.
Hemangiomas are usually “normal” on bone scintigraphy.
Metabolic scintigraphy findings can precede anatomic changes in spondylolysis.
Suggested Readings
Han BK, Ryu JS, Moon DH, Shin MJ, Kim YT, Lee HK. Bone SPECT imaging of vertebral hemangioma correlation with MR imaging and symptoms. Clin Nucl Med. 1995; 20(10):916–921 Park JS, Moon SK, Jin W, Ryu KN. Unilateral lumbar spondylolysis on radiography and MRI: emphasis on morphologic differences according to involved segment. AJR Am J Roentgenol. 2010; 194(1):207–215 Yang J, Servaes S, Edwards K, Zhuang H. Prevalence of stress reaction in the pars interarticularis in pediatric patients with new-onset lower back pain. Clin Nucl Med. 2013; 38(2):110–114Case 85

Clinical History
21-year-old male with five days of left hip pain after completing an obstacle course (▶Fig. 85.1).
Key Finding
Focally increased uptake in the hip on bone scintigraphy
Top 3 Differential Diagnoses
Stress fracture. Femoral neck stress fractures present with focal pain in the hip or groin, often in cases of athletes and runners. Plain film radiographs often fail to demonstrate significant changes, particularly early in the course. Untreated femoral neck stress fractures have complications including avascular necrosis (AVN), making diagnosis important. Single-photon emission computed tomography (SPECT) images are essential if bone scan is performed, as around half of femoral neck stress fractures will be missed on planar images. Magnetic resonance imaging is the gold standard in diagnosis showing edema and a fracture line. Stress fractures more commonly involve the compressive side of the femoral neck. Tension side femoral neck stress fractures must be made nonweight-bearing with immediate orthopedic referral.
Stress change without complete fracture. Fracture is the result of ongoing stress change. With abatement of the causative factor, edema, subtotal fracture, and repair may occur. Bone scintigraphy will still demonstrate increased metabolic activity before anatomic imaging is abnormal.
Synovial herniation pit. Also known as “Pitt’s pit,” it can present as a focal area of increased radiotracer distribution on bone scintigraphy. This is associated with a small round to oval lucency with surrounding thin sclerosis just distal to the femoral articular surface, in an anterior-superior location.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree