Part 5 Hepatobiliary
Case 48

Clinical History
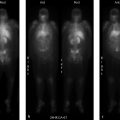
80-year-old male with methicillin-resistant Staphylococcus aureus bacteremia of unknown source, in septic shock, status post endoscopic retrograde cholangiopancreatography (ERCP) with biliary stent placement two days prior with increasing abdominal distention, transaminitis, and hyperbilirubinemia. Referred for hepatobiliary scintigraphy (HBS) to assess for obstruction (▶Fig. 48.1).
Key Finding
Delayed clearance of blood pool on HBS
Diagnosis
Hepatic dysfunction. HBS is performed utilizing iminodiacetic acid (IDA) derivatives tagged with Tc-99m. Currently bromotriethyl-IDA (mebrofenin) and diisopropyl-IDA (disofenin) are used in the United States. These agents remain tightly bound to protein in the blood which limits renal clearance. They dissociate from albumin in the liver and are extracted by hepatocytes, like bilirubin, then secreted unchanged into the biliary canaliculi. The modern IDA derivatives, created through alterations of the benzene ring, have better hepatic uptake allowing for clinical use in patients with higher bilirubin levels. Tc-99m mebrofenin has the highest liver extraction percentage and more rapid biliary clearance and it resists displacement by high bilirubin concentrations.
HBS, frequently called “HIDA” scan as homage to the first clinically useful IDA derivative, involves anterior dynamic imaging of the abdomen after radiopharmaceutical administration. The dynamic information allows for qualitative assessment of the imaged blood pool, hepatic parenchymal uptake, hepatic transit, biliary ductal system, gallbladder, and biliary-to-bowel transit.
Hepatic uptake should be diffuse and homogeneous with an abrupt increase in activity as the tracer makes it to the portovenous system, and it should result in rapid clearance of the blood pool. Normally, the blood pool should clear within 5 to 10 minutes. Delayed blood clearance is indicative of hepatocellular dysfunction which may be secondary to multiple causes including cirrhosis, fibrosis, and chronic biliary obstruction. With hepatic dysfunction, there may be vicarious radiopharmaceutical excretion through the kidneys. This is important to differentiate from biliary or bowel activity, particularly when evaluating neonatal jaundice.
Some quantitative methods have been derived for evaluation of hepatic function, but are not generally part of standard cholescintigraphy. These methods generally involve analysis of time–activity curves from regions of interest drawn around the liver and heart.
The presence of hepatocellular dysfunction affects the ability to evaluate for cholecystitis with cholescintigraphy. The predictive value of gallbladder visualization and biliary-to-bowel transit within 1 hour requires normal hepatic function. If dysfunction is present, delayed images may be necessary to truly evaluate for cystic duct obstruction or delayed biliary transit.
Diagnosis
Hepatocellular dysfunction.
✓ Pearls
Hepatic dysfunction results in delayed uptake of IDA derivatives, seen as prolonged blood pool activity.
Predictive measures of gallbladder visualization within 60 minutes requires normal hepatic function.
Vicarious renal excretion can simulate biliary or bowel activity when evaluating neonatal jaundice.
Modern IDA derivatives have better hepatic uptake allowing for usage with higher bilirubin levels.
Suggested readings
de Graaf W, Bennink RJ, Veteläinen R, van Gulik TM. Nuclear imaging techniques for the assessment of hepatic function in liver surgery and transplantation. J Nucl Med. 2010; 51(5):742–752 Tulchinsky M, Ciak BW, Delbeke D, et al. Society of Nuclear Medicine. SNM practice guideline for hepatobiliary scintigraphy 4.0. J Nucl Med Technol. 2010; 38(4):210–218 Ziessman HA. Hepatobiliary scintigraphy in 2014. J Nucl Med. 2014; 55(6):967–975Case 49

Clinical History
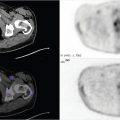
26-year-old female postoperative day 2 from laparoscopic cholecystectomy, febrile and tachycardic with increasing total bilirubin. Referred for evaluation for biliary leak versus obstruction (▶Fig. 49.1).
Key Finding
Delayed biliary clearance on Tc-99m mebrofenin hepatobiliary scintigraphy (HBS)
Top 3 Differential Diagnoses
Biliary obstruction (high grade or partial). Complete common bile duct obstruction can be missed with anatomic imaging in the acute stage as the gallbladder can collect the undrained bile preventing biliary duct dilation. HBS at this time may appear normal with the exception of absent bowel activity, even on delayed imaging. After about 24 hours, the gallbladder’s reservoir capacity will be overwhelmed which then results in increased pressure in, and eventually dilation of, the biliary tree. The increase in pressure impedes bile excretion into the bile canaliculi. At this stage, HBS will likely still show good hepatic extraction and clearance of the blood pool, but no activity will be seen entering the common bile duct, gallbladder, or bowel. If obstruction is not resolved, it will eventually lead to hepatocellular damage. Partial biliary obstruction can be more of a diagnostic challenge with HBS. Findings of partial duct obstruction, depending on chronicity, are in general very nonspecific and can include delayed blood pool clearance, delayed hepatic transit and biliary clearance, and delayed biliary-to-bowel transit. As absent biliary-to-bowel transit may be the only abnormality on HBS with acute complete common bile duct obstruction, some providers will not administer sincalide (cholecystokinin [CCK]-8) in this setting. It is not an absolute contraindication as there are many other causes of delayed biliary-to-bowel transit. CCK-8 should be used with caution if the clinical scenario matches acute biliary obstruction.
Hepatic dysfunction. Hepatocellular function is essential for HBS as the iminodiacetic acid (IDA) derivatives are handled like bile. Decreased hepatic function can affect all stages of HBS, leading to delays in blood pool clearance, biliary duct visualization, and biliary-to-bowel transit, and therefore, can mimic biliary obstruction.
Cholestatic jaundice. Nonobstructive cholestasis can result in a similar pattern of delayed biliary clearance. Patients who are receiving total parenteral nutrition are at risk for this condition, which can lead to acalculous cholecystitis. Cholestasis can also be associated with several medications, the postoperative state, congenital abnormalities, and pregnancy, among other things.
Diagnosis
Iatrogenic common bile duct obstruction.
✓ Pearls
HBS cannot always distinguish between obstruction, hepatocellular dysfunction, and cholestasis.
Absent biliary-to-bowel transit may be the only abnormality on HBS with acute biliary obstruction.
CCK-8 should be administered with caution if biliary-to-bowel transit is not seen within 60 minutes.
Hepatic function is essential for HBS, decreased function can affect all stages of the exam.
Suggested Readings
Low CS, Ahmed H, Notghi A. Pitfall and limitations of radionuclide hepatobiliary and gastrointestinal system imaging. Semin Nucl Med. 2015; 45(6):513–529 Roy-Chowdhury N, Roy-Chowdhury J. Diagnostic approach to the adult with jaundice or asymptomatic hyperbilirubinemia. In:UpToDate, Chopra S (Ed), UpToDate, Waltham, MA. (Accessed on November 17, 2016) Ziessman HA. Nuclear medicine hepatobiliary imaging. Clin Gastroenterol Hepatol. 2010; 8(2):111–116Case 50

Key Finding
Delayed biliary-to-bowel transit on HBS
Top 3 Differential Diagnoses
Normal variant. Normally, the hepatobiliary radiotracer is excreted through the bile ducts into the duodenum within 1 hour. However, around one-fifth of healthy patients with normal hepatobiliary function will demonstrate delayed biliary-to-bowel transit. This is likely secondary to physiologic factors relating to fasting state, including the amount of circulating endogenous CCK hormone and the native hypertonicity of the sphincter of Oddi (SO).
Biliary obstruction. There are numerous causes of both low-grade and high-grade biliary obstruction, including stones, benign or malignant strictures, inflammation from pancreatitis or cholangitis, and SO dysfunction (fixed or reversible). Low-grade or partial obstruction is suggested when bowel activity is identified greater than 1 hour, but less than 24 hours. High-grade biliary obstruction can result in a persistent hepatogram with absence of bowel activity at 24 hours. Longstanding obstruction can slowly cause hepatocellular dysfunction that decreases blood pool clearance of radiotracer.
Chronic cholecystitis. Intermittent cystic duct obstruction over a period of time can result in inflammation and fibrosis of the gallbladder wall, termed as chronic cholecystitis. Chronic cholecystitis primarily presents scintigraphically as filling of the gallbladder only on delayed images (2–4 hours) or after morphine augmentation; a less reliable and secondary sign of chronic cholecystitis is delayed biliary-to-bowel transit, possibly due to associated inflammation of the ampulla.
Additional Diagnostic Considerations
Sphincter of Oddi dysfunction: Abnormal contraction of the SO, which should normally relax with gallbladder contraction, can lead to delayed biliary-to-bowel transit.
Medication effect: Several medications can result in delayed visualization of small bowel activity on HBS. These include various medications that result in drug-induced cholestasis, as well as opiates due to SO contraction. Pretreatment with CCK can also cause a delay in biliary-to-bowel transit.
Hepatocellular dysfunction: This can result in delayed biliary-to-bowel transit due to associated cholestasis.
Diagnosis
Unknown.
✓ Pearls
Delayed biliary-to-bowel transit is a nonspecific finding that can be a normal variant.
Biliary obstruction and nonobstructive cholestasis can result in delayed biliary-to-bowel transit.
Delayed biliary-to-bowel transit can be an indicator of chronic cholecystitis.
Suggested Readings
Lambie H, Cook AM, Scarsbrook AF, Lodge JP, Robinson PJ, Chowdhury FU. Tc99 m-hepatobiliary iminodiacetic acid (HIDA) scintigraphy in clinical practice. Clin Radiol. 2011; 66(11):1094–1105 Tulchinsky M, Colletti PM, Allen TW. Hepatobiliary scintigraphy in acute cholecystitis. Semin Nucl Med. 2012; 42(2):84–100 Ziessman HA. Hepatobiliary scintigraphy in 2014. J Nucl Med. 2014; 55(6): 967–975Case 51

Clinical History
77-year-old male with known acute cholecystitis post ERCP with concern for bile leak (▶Fig. 51.1).
Key Finding
Nonvisualization of gallbladder on hepatobiliary imaging
Top 3 Differential Diagnoses
Acute cholecystitis. Acute cystic duct obstruction is the hallmark of acute cholecystitis. Hepatobiliary imaging has a high specificity (98%) and negative predictive value (99%) and is very useful in cases where ultrasound findings are equivocal. Under normal circumstances, the gallbladder is visualized within 1 hour of radiotracer administration. Nonvisualization of gallbladder activity within 4 hours of radiotracer injection in the setting of normal visualization of biliary and bowel activity is diagnostic of acute cholecystitis. Alternatively, morphine (0.04 mg/kg IV) may be administered after 1 hour of dynamic imaging. Nonvisualization of the gallbladder within 30 minutes of morphine administration is also diagnostic of acute cholecystitis. The “cystic duct” or “nubbin” sign may be seen as focal activity within the cystic duct up to the site of obstruction. Increased pericholecystic hepatic parenchymal activity (“rim sign”) can be an ominous sign of complicated/advanced (gangrenous, necrotic, or perforated) cholecystitis necessitating immediate surgical intervention.
Chronic cholecystitis. Delayed visualization of the gallbladder between 1 to 4 hours postinjection, or within 30 minutes after morphine augmentation, is suggestive of chronic cholecystitis. A second injection of radiopharmaceutical, or “booster dose,” may be necessary after the initial 60-minute image acquisition, if there is insufficient remaining hepatic or biliary tree activity to permit gallbladder filling.
Inadequate patient preparation. False-positives can occur with insufficient (< 4 hours) or prolonged (>24 hours) fasting, or prolonged hyperalimentation. Pretreatment with cholecystokinin (CCK), 30 minutes prior to injection, is usually recommended for prolonged fasting and hyperalimentation to allow the distended gallbladder to drain. Patients with a recent meal are imaged after fasting for a minimum of 4 hours.
Additional Diagnostic Considerations
Severe hepatocellular disease: Poor hepatocellular function can result in poor extraction and excretion of the radiotracer, resulting in delayed blood pool clearance (>10 min). False-positive studies occur due to delayed or nonvisualization of gallbladder. The key is to note the delayed blood pool clearance.
High-grade biliary obstruction: Prompt hepatic uptake without biliary excretion of radiotracer (“liver scan” sign) suggests biliary duct obstruction. Delayed 4- and 24-hour imaging is generally obtained to evaluate for bowel activity. The gallbladder may or may not fill depending upon the location and duration of obstruction. CT scan or magnetic resonance cholangiopancreatography (MRCP) may be helpful not only in establishing the diagnosis but also in determining a possible cause of obstruction.
Diagnosis
Acute cholecystitis.
✓ Pearls
Hepatobiliary scan is highly sensitive and specific for acute calculous cholecystitis.
False-positives may be seen with recent meal, extended fasting (> 24 hour), and hepatocellular dysfunction.
The “rim sign” can indicate complicated/advanced (gangrenous, necrotic, or perforated) cholecystitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree