Fig. 9.1
(a–c) PA, lateral, and merchant views of the left knee, demonstrating excessive patellar tilt and subluxation, with moderate degenerative changes of the lateral patellar facet
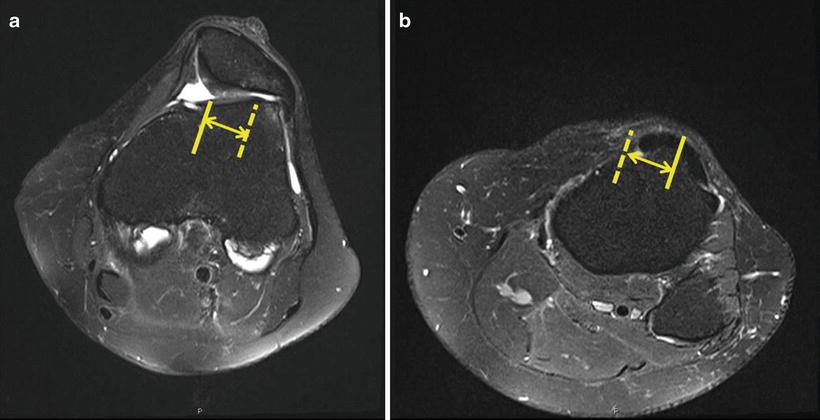
Fig. 9.2
(a, b) MRI demonstrating increased TT-TG distance and patellar malalignment. Solid line demonstrates trochlear groove in a and tibial tubercle in b. Dashed lines indicate the superimposed line of the opposing structure. The arrow represents the TT-TG distance
Given the patients’ findings of increased TT-TG distance, excessive patellar tilt and subluxation, and chondral wear of the lateral patellar facet, she was indicated for surgery consisting of anteromedialization osteotomy of the tibial tubercle, lateral retinacular release, MPFL reconstruction with hamstring autograft, and shaving chondroplasty of the patella.
Surgery
At the time of surgery, a diagnostic arthroscopy was performed, with confirmation of full-thickness cartilage loss on the lateral patellar facet and lateral trochlea. A shaving chondroplasty was performed, debriding the chondromalacia back to a stable rim (Fig. 9.3a, b). Next, the open portion of the procedure was initiated. An 8 cm incision along the medial patellar edge extending to the level of the tibial tubercle was placed. An open lateral retinacular release was performed, with care taken to protect the superior lateral geniculate artery. This was able to correct the excessive lateral patellar tilt. Next, attention was turned to the tibial tubercle osteotomy. A 45° angle of osteotomy was chosen, and the distal periosteum of the osteotomy was left intact to serve as a hinge point. A correction of 1 cm of medialization and 7 mm of anteriorization was achieved to reduce the TT-TG to a desired 10 mm. Provisional clamps were placed, and tracking was checked prior to placement of two 4.5 mm bicortical screws (Fig. 9.4). The final step involved MPFL reconstruction to address the patella subluxation. Gracilis autograft was harvested in the standard fashion and prepared on the back table. The proximal medial border of the patella was dissected, and two parallel 3.2 mm tunnels were drilled from the medial border to the anterior mid-patella to allow a looped passage of the gracilis graft, leaving the free ends for attachment in the femur. Schottle’s point was identified at the junction between Blumenstadt’s line and the posterior femoral condyles, along the posterior cortical line of the femur [16] (Fig. 9.5). A guide pin was placed at the MPFL origin. Isometry was then checked with the graft around the guide pin by taking the knee through a full range of motion. After verification, final graft passage and interference screw femoral fixation was completed with the knee at 45° of flexion so that the patella was fully seated within the trochlear groove during tensioning.
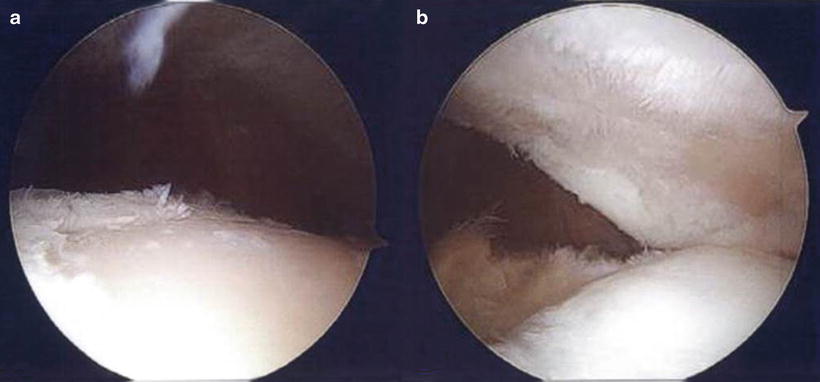


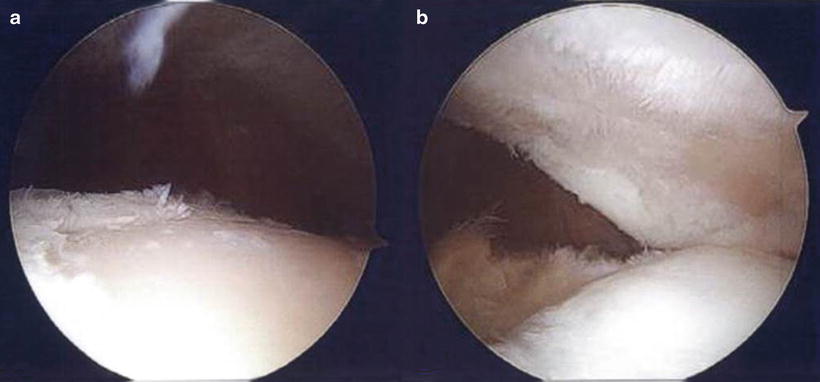
Fig. 9.3
Arthroscopic images showing full-thickness cartilage loss on both the lateral trochlea (a) and lateral patellar facet (b)

Fig. 9.4
Intraoperative fluoroscopy showing bicortical screw fixation of tibial tubercle osteotomy

Fig. 9.5
Lateral intraoperative radiograph showing Schottle’s point, the junction between Blumenstadt’s line and the posterior femoral condyles, along the posterior cortical line of the femur
Postoperatively, the patient was initially restricted to 50 % weight bearing until the osteotomy was healed (Fig. 9.6a–c). Flexion began at 0–60° and increased by 30° every 2 weeks in a hinged brace. She ultimately went on to heal uneventfully, although she continued to report occasional anterior knee pain and slight irritation related to the tibial tubercle screws, which required hardware removal at 15 months postoperative. Final radiographs prior to hardware removal are shown in Fig. 9.7a, b.



Fig. 9.6
Initial postoperative radiographs, showing fixation of the tibial tubercle (a, b) osteotomy and correction of excessive patellar tilt (c)

Fig. 9.7
(a, b) Final PA and lateral radiographs demonstrating a healed tibial tubercle osteotomy
Discussion
General indications for combined proximal and distal procedures in patellar maltracking
Essential steps for proper execution of tibial tubercle osteotomy, MPFL reconstruction
Case 2
History/Exam
A 13-year-old female presented to clinic with bilateral knee pain, left greater than right, since early childhood. There was no history of specific injury; however, the patient reportedly had subluxation of both kneecaps with every step, and pain was worsened by any prolonged activities. Prior to her presentation, she had received no operative treatment, but had failed a trial of physical therapy and activity modification. On initial examination, the patient was noted to have external rotation and valgus alignment of both her lower extremities. There was an effusion at the knees bilaterally, with patellar crepitus, tenderness, and apprehension. There was a markedly positive J sign with gross subluxation of the patella requiring manual reduction for the knee to flex. Essentially, her patellas dislocated constantly. The remaining examination findings were unremarkable.
Imaging
On initial imaging, the patient was noted to have a Caton–Deschamps ratio of 1.14 bilaterally, with severe trochlear dysplasia (Dejour type D) with a supratrochlear spur on the left and less severe on the right (Fig. 9.8a–d). There was evidence of MPFL insufficiency bilaterally, with patellar subluxation and excessive lateral tilt. The femoral tibial anatomic axis was 7°, and there was bowing of the femur and tibia resulting in mechanical axis displacement lateral to the joint center. A bilateral lower extremity computed tomography scan was ordered for surgical planning (Fig. 9.9a, b). On the left lower extremity, the femoral neck was retroverted 12° relative to the femoral condylar axis. There was marked trochlear dysplasia, with lateral subluxation and tilt. There was a chronic ossicle of the medial patella, suggestive of chronic avulsion injury from the patella. The TT-TG distance was 23 mm. On the right lower extremity, the femoral neck was retroverted 5°, with trochlear dysplasia and less severe lateral patellar subluxation and tilt. The TT-TG distance was measured at 28 mm. If desired, a 3D reconstruction CT scan can also be obtained for preoperative planning (Fig. 9.9c).
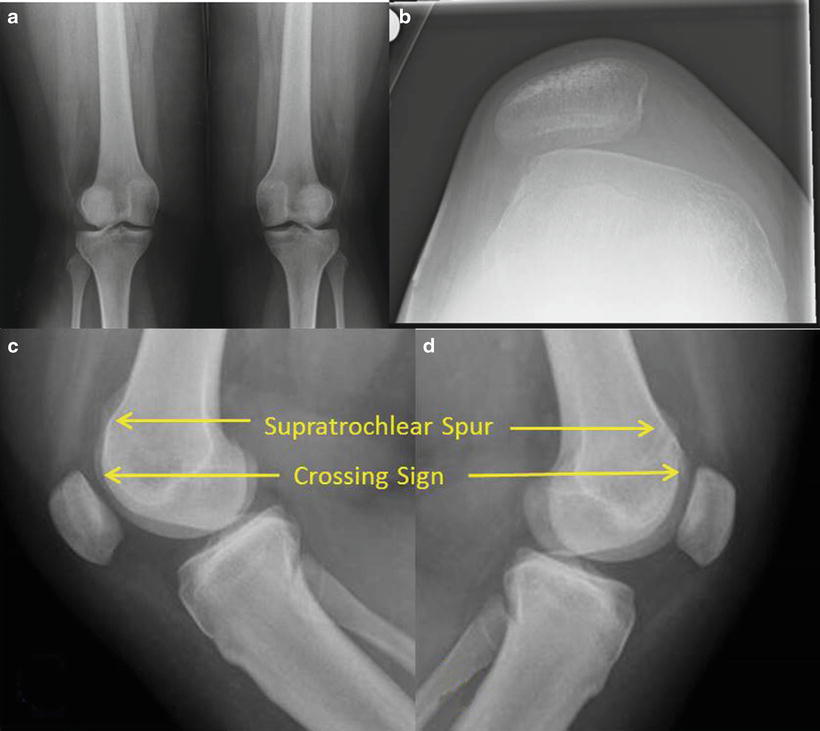
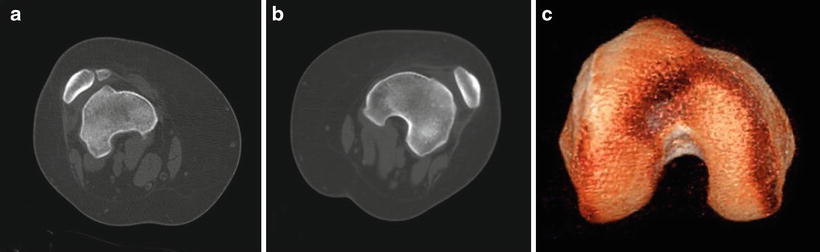
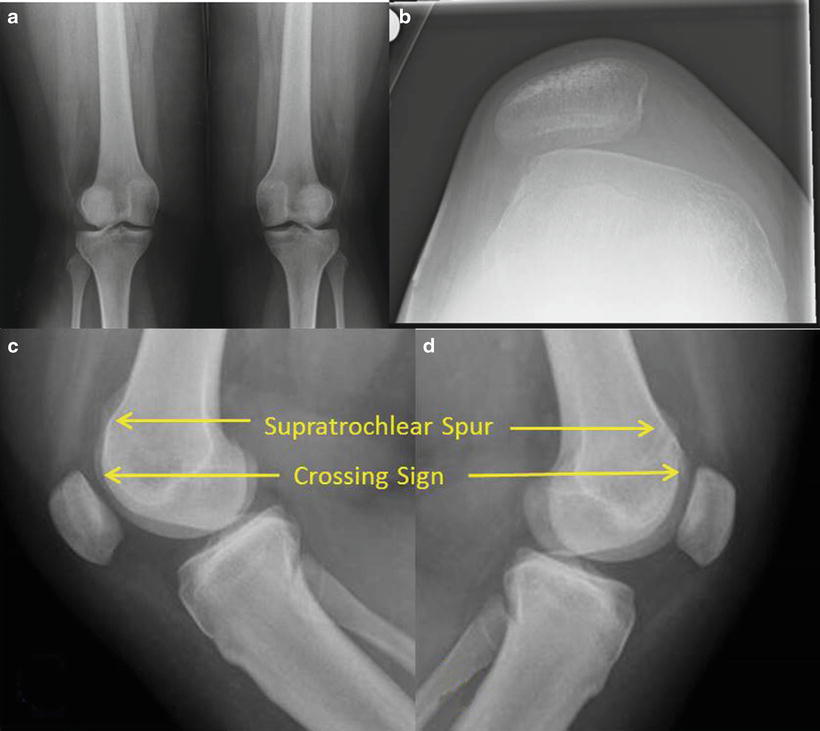
Fig. 9.8
(a–d) PA, merchant (R knee), and lateral radiographs, demonstrating Dejour type D trochlear dysplasia bilaterally (arrows), more severe on the left. The crossing sign represents the point at which the trochlea is flattened
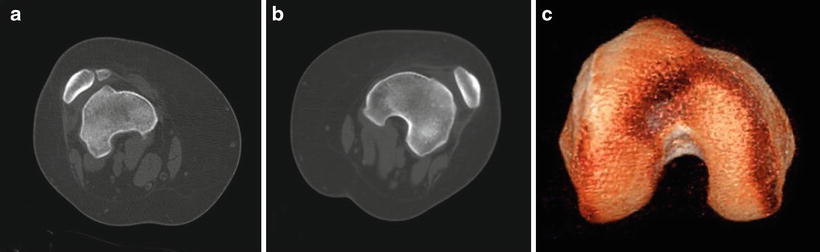
Fig. 9.9
(a) Right lower extremity CT showing a supratrochlear spur, patellar ossicle, and abnormal femoral rotation. (b) Left lower extremity CT showing a more severe rotational abnormality of the femur, with chronic patellar subluxation and trochlear dysplasia. (c) 3D reconstruction of CT scan for visualization of trochlear dysplasia
Based on the patients’ findings of increased TT-TG distance, excessive patellar tilt, and severe trochlear dysplasia, she was indicated for surgery consisting of anteromedialization osteotomy of the tibial tubercle, lateral retinacular release, MPFL reconstruction with hamstring autograft, and sulcus deepening trochleaplasty. Since the left knee showed more severe symptoms at the time of her presentation, the decision was made for staged reconstruction starting with the left lower extremity. The patient did well clinically following her initial procedure and was indicated for her contralateral knee at 6 months postoperatively. The surgical sequence was similar, and to avoid redundancy, presented findings are based on the patient’s second procedure only.
Surgery
On the patient’s second procedure date, an examination under anesthesia was performed, confirming gross instability and maltracking of the right patella. Next, a standard medial parapatellar arthrotomy was placed. First, the tibial tubercle osteotomy was prepared, and a cut was made at 45°, leaving a distal periosteal hinge intact. Translation of 13 mm was achieved, based on the preoperative TT-TG distance of 28 mm to achieve a final distance of 15 mm, and the fragment was provisionally fixed with a clamp. Two bicortical 4.5 mm screws were placed after verifying correction of patellar tracking through a full range of motion.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








