Chapter 21 Pathology
 The purpose of medical imaging is to demonstrate the presence or absence of disease, so it is important for imaging practitioners to have some understanding of the types they might encounter.
The purpose of medical imaging is to demonstrate the presence or absence of disease, so it is important for imaging practitioners to have some understanding of the types they might encounter. Many diseases share common pathological processes relating to the causation and progression of the illness.
Many diseases share common pathological processes relating to the causation and progression of the illness. Understanding these general concepts in pathology can aid in the understanding of diseases specific to particular regions of the body.
Understanding these general concepts in pathology can aid in the understanding of diseases specific to particular regions of the body.INFECTION
Infection occurs when microorganisms multiply in tissues where they are normally absent or present in only small numbers. Those that cause disease are described as pathogenic (Table 21.1). The types of microorganism involved in infection include bacteria, viruses, yeast, fungi and protozoa.
Table 21.1 Examples of pathogenic microorganism
| Disease | Organism and type | Effect |
|---|---|---|
| Tuberculosis (TB) | Mycobacterium tuberculosis (bacterial) | Pulmonary or other organ infection resulting in chronic inflammation and tissue destruction |
| Cholera | Vibrio cholera (bacterial) | Severe diarrhoea |
| Pneumonia | Streptococcus pneumoniae and others (bacterial) | Pulmonary inflammation with fever |
| Osteomyelitis | Staphylococcus aureus and others (bacterial) | Often chronic bone infection resulting in pain and swelling |
| Gangrene | Clostridium perfringens (bacterial) | Severe tissue destruction resulting in tissue death and putrefaction |
| Acquired immune deficiency syndrome (AIDS) | Human immunodeficiency virus (HIV) | Destruction of T lymphocytes resulting in increased susceptibility to infection and development of rare tumours; e.g. Kaposi’s sarcoma |
| Influenza | Influenza virus | Severe respiratory tract infection. Potentially fatal depending on the strain |
| Squamous epithelial tumours | Human papilloma virus | Malignant transformation of infected squamous epithelium, especially in the cervix |
| Viral hepatitis | Hepatitis B virus and others | Liver inflammation and potentially fatal |
| Pneumonia | Pneumocystis carinii (fungus) | Another cause of pneumonia, particularly in the immunocompromised; e.g. AIDS |
| Aspergillosis | Aspergillus fumigatus (fungus) | Chronic lung infection |
| Thrush | Candida albicans (yeast) | Mucous membrane lesions |
| Malaria | Plasmodium (protozoa) | Fever, anaemia, liver, spleen and lymph node enlargement. Potentially fatal |
INFLAMMATION
Inflammation may be of rapid (acute) or slow (chronic) onset.
ACUTE INFLAMMATION
Acute inflammation displays typical features:
Causes of acute inflammation include:
CHRONIC INFLAMMATION
Causes of chronic inflammation include:
CARCINOGENESIS
Tissues that are growing or that have to replace cells lost or damaged as part of their normal function will show rapid cell division; in other tissues cell division will be very slow. In both cases the process is highly coordinated to ensure that the tissue is renewed in a way appropriate to itsfunction. Sometimes this careful coordination is lost and a cell may begin to divide more frequently than normal. As a result a mass of abnormal tissue may form which may be referred to as a neoplasm or tumour. The transformation of normal tissues or benign tumours into cancer is called carcinogenesis. Box 21.1 explains some of the terminology relating to tumours.
CANCER INCIDENCE
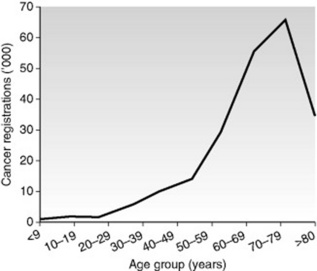
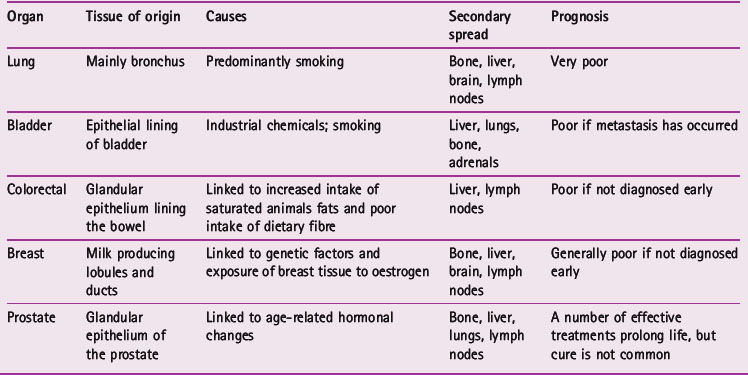
Cancer incidence increases with age (Fig. 21.1). The transformation of a normal cell into a cell that will form a tumour is primarily a genetic event, but this may be triggered by environmental factors. Cells from older people have had more time to experience the environmental factors that can lead to carcinogenesis and this may explain the increasing incidence with age. Table 21.2 gives details of some commonly seen cancers.
TUMOUR BEHAVIOUR
Malignant tumours
The grading and staging of malignant tumours
The prognosis of a person’s cancer is determined by both its grade and its stage. Grade refers to how well differentiated the tumour cells are; that is, how much like the tissue of origin they are. Poorly differentiated cells that have lost the particular characteristics of the organ from which they arise tend to form more aggressive tumours. Stage is determined by the size of the primary tumour and the degree of spread to local or remote organs and lymph nodes. Table 21.3 explains the staging scheme used for breast cancer.
Table 21.3 The main staging systems used to assess the extent of spread of breast carcinomas
| Stage | Extent of spread |
|---|---|
| International classification | |
| I | Lump with slight tethering to skin, but node negative |
| II | Lump with lymph node metastasis or skin tethering |
| III | Tumour which is extensively adherent to skin and/or underlying muscles, or ulcerating or lymph nodes are fixed |
| IV | Distant metastases |
| TNM | |
| T1 | Tumour 20 mm or less; no fixation or nipple retraction. Includes Paget’s disease |
| T2 | Tumour 20–50 mm, or less than 20 mm but with tethering |
| T3 | Tumour greater than 50 mm but less than 100 mm; or less than 50 mm but with infiltration, ulceration or fixation |
| T4 | Any tumour with ulceration or infiltration wide of it, or chest wall fixation, or greater than 100 mm in diameter |
| N0 | Node-negative |
| N1 | Axillary nodes mobile |
| N2 | Axillary nodes fixed |
| N3 | Supraclavicular nodes or oedema of arm |
| M0 | No distant metastases |
| M1 | Distant metastases |
SKELETAL SYSTEM
ARTHRITIS
As a result of these changes, those with osteoarthritis may experience pain on movement, stiffness and joint instability. If this becomes severe it may be necessary to perform a total joint replacement (Fig. 21.2).
PAGET’S DISEASE
Paget’s is a fairly common disease affecting the elderly, arising from a disordering of normal bone turnover. Affected bones are characterised by an increase in bone synthesis, resulting in a thickened and sclerotic ‘cotton wool’ appearance radiographically. Paget’s usually affects the pelvis, skull and long bones, often progressing from one end towards the centre. Weight-bearing bones affected by Paget’s, such as the femur and tibia, can become bowed (Fig. 21.4). When the skull is affected there may be encroachment on the cranial nerve foramina, causing various neurological symptoms including vertigo, blindness and deafness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree