7 Pathology of the Nasal Cavity and Paranasal Sinuses
Nonmalignant Pathology of the (Para)nasal Sinuses
Maxillary Sinusitis
Differential Diagnosis
• All causes of obstruction of the maxillary sinus that might induce fluid levels or persistent sinusitis.
• Periapical pathology with inflammation and osteolysis.
• Solitary (fungal) infection.
• Trauma leading to bony dislocation and obstruction of drainage from the sinus.
• Benign and malignant lesions.
Points of Evaluation
• The Waters and Caldwell views are complementary and must always be available for comprehensive evaluation and avoiding misinterpretation due to superimposition of bony structures.
• The area of the natural ostium of the sinus might be obstructed. Computed tomography (CT) can show this obstruction in more detail.
• Pay close attention to unilateral opacities, which are suggestive of tumor or odontogenic infection.
• Complete opacification may be demonstrated after previous endonasal sinus surgery, Caldwell–Luc procedures, or after orbital decompressions in Graves disease. In these patients, conventional radiography is not very useful and CT should be used for a comprehensive detailed examination.

Fig. 7.1 a,b Conventional radiographic views for sinus evaluation.
a Caldwell view. This 26-year-old patient had pain in the right maxillary region. The right maxillary sinus seems to be opacified in the lower part (1). The left frontal sinus is absent and the right frontal sinus is hypoplastic (2).
b Waters view. This view shows clear air–fluid level (1) in the right maxillary sinus seen in Fig 7.1a. The aeration of the maxillary sinus on the left side is confirmed. The sphenoid sinus is visible, showing normal pneumatization and aeration (2). In addition, a bony septal deviation to the right (3) is observed and there is opacification of the mastoid cells on the right side (4).
Adenoid Hypertrophy
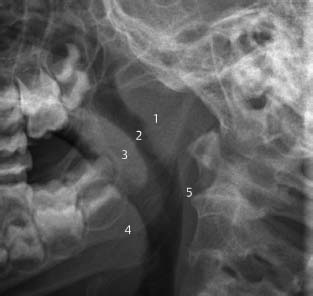
Fig. 7.2 Plain radiograph for adenoid evaluation.
Lateral skull view. Previously, in the absence of flexible endoscopes or in cases of doubt in younger children, the presence and size of the adenoid was evaluated on conventional plain films. In this lateral view of the skull, the adenoid (1) is enlarged quite extensively and almost completely obstructs the nasopharyngeal airway (2). Also seen are the velum and uvula (3), base of tongue (4), and posterior pharyngeal wall (5).
Fracture of the Nasal Bone and Retention Cysts
Differential Diagnosis
The radiologic features as seen in Fig. 7.3 are typically pathognomic of retention cysts. In general, these retention cysts must be considered nonpathologic findings. Clinically, they are often asymptomatic or found in patients with minor complaints. In conventional radiographic views, and also on CT, these cysts may be confused with mucosal thickening of the maxillary sinus wall.
Points of Evaluation
In cases of large cysts resulting in obstruction of the maxillary sinus and those accompanied by signs of sinusitis, surgical removal (marsupialization) might be considered to improve drainage.
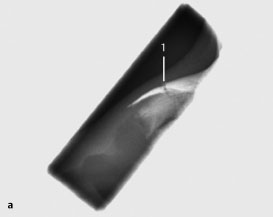
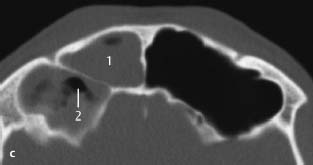
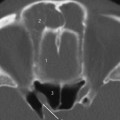
Fig. 7.3 a–c Mild trauma to the nose. Hematoma made palpation difficult to exclude a fracture.
a Plain radiograph, lateral view. This view of the nasal bone in a patient with facial trauma demonstrates a fracture of the nasal bone (1), with slight depression and dislocation of the anterior part. Although the field of radiation has been restricted as much as possible, these views are not regularly taken, since palpation in most cases is sufficient to diagnose a fracture. Such radiographs may be considered in cases of severe swelling, which prevents adequate evaluation by palpation, and in cases of violence, for medicolegal reasons. CT is superior for accurate evaluation in cases of extensive facial trauma.
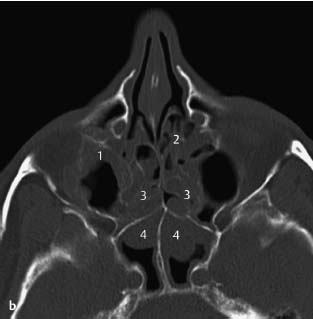
Fig. 7.3b patient after facial trauma.
b CT, axial. Patient with facial trauma showing multiple fracture lines in the nasal bone (1). No other fractures were noted. A coincidence finding was a rounded lesion with smooth borders in the posterior wall of the right maxillary sinus (2). No other (mucosal) pathology of the maxillary sinus was noted. The lesion is a retention cyst. On coronal views (not shown), these cysts are most frequently found on the floor of the maxillary sinus.
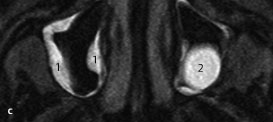
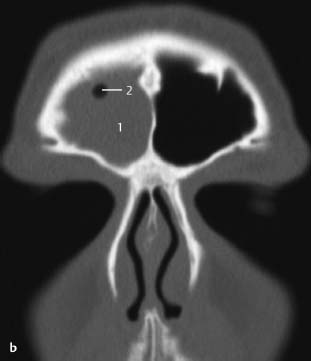
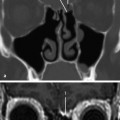
Fig. 7.3 c Retention cysts.
c MRI, T2-weighted, axial. This patient was seen by a neurologist and complained of pressure in the region of the maxillary sinus. On the right side, the hyperintense signal (1) is indicative of mucosal thickenings adhering to the wall of the maxillary sinus. There are no signs of extensive sinusitis with no evidence of fluid levels in the sinus. On the left side, a solitary retention cyst (2) is seen; it is filled with hyperintense fluid and is not obviously adherent to the wall of the sinus. There is slight mucosal thickening seen in the region of the cyst.
Differential Diagnosis
• All etiologies causing mucosal swelling and polyps.
• Chronic rhinosinusitis with or without polyps, associated with hyperreactivity, allergy, smoking.
• Less frequently: Wegener granulomatosis, which typically is associated with destruction of the nasal septum; sinonasal malignancies, which usually show infiltration of surrounding structures and/or bone destruction; and allergic fungal sinusitis.
Points of Evaluation
• Bilateral soft-tissue disease is a reassuring finding, as it usually indicates benign disease such as chronic sinusitis or polyposis.
• Anatomic structures obstructing the sinuses, due to a growth spurt in adolescence, may play a role.
• In cases with symptoms that arise later in life, concomitant secondary pathology is responsible.
• Bone destruction is the hallmark of infiltrating processes and malignant behavior.
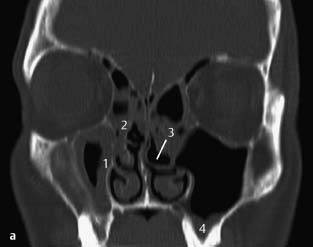
Fig. 7.4 a, b Patient with nasal obstruction, smell disorder, and rhinorrhea.
a CT, coronal. The scan shows mucosal thickening in the right maxillary sinus (1), partial opacification of the ethmoid cells (2) on both sides, pneumatization of the left middle turbinate (3), and thickened mucosa on the floor of the left maxillary sinus (4). The maxillary tooth roots are in close proximity to the floor of the sinus, which is extending down between the roots (i.e., normal finding).
b CT, axial. Mucosal thickening of the walls of maxillary sinus (1). The concha bullosa on the left side (2) is less visible on this slice. Note the opacification of the ethmoid (3) and mucosal thickening of the anterior walls of the sphenoid sinus (4) with a smooth-bordered, rounded, expansile appearance suggestive of polyps. Bone destruction is not present.
Differential Diagnosis
Nasal polyps, antrochoanal polyps, inverted papilloma, unilateral chronic odontogenic sinusitis with secondary polyps due to chronic infection, unilateral fungal sinusitis, mucoceles, malignancy and cystic fibrosis (similar appearance but commonly bilateral).
Points of Evaluation
• Destruction of bony outlines (with infiltrative characteristics) is suggestive of inverted papilloma, malignancies, or fungal infection.
• Calcifications in the opacified area are suggestive of fungal infection. Resorption of bone around tooth roots suggests odontogenic infection.
• Beware of pathology in the sphenoethmoidal fossa (i.e., juvenile angiofibroma).
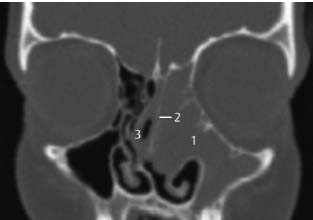
Fig. 7.5 Patient with blocked left nose.
CT, coronal. Complete opacification of the left maxillary sinus and ethmoid (1) is seen. Medial displacement of the middle turbinate (2) and nasal septum (3), indicates chronic compression of these structures. There are no signs of bony destruction of the orbital rim or the maxillary sinus or any calcifications in the opacified area.
Differential Diagnosis
• Conditions causing mucosal swelling and polyps, obstructing the frontal recess.
• Unilateral processes such as inverted papilloma or malignancies.
• Fungal infections.
Points of Evaluation
• The anatomy and pathology of the frontal recess required special attention.
• In cases of persisting drainage problems in the region of the frontal recess, the septum between the frontal sinuses may be removed for establishing drainage by way of the left frontal recess.
• Bony destruction with infiltrative characteristics is suggestive of malignancy.
• Calcifications in the opacified area are suggestive of fungal infections.
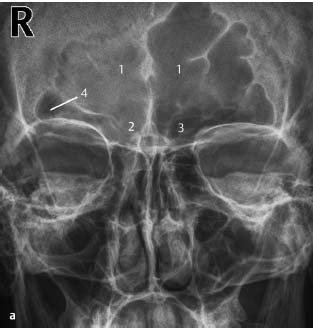
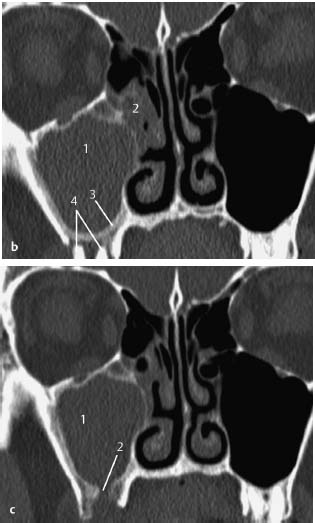
Fig. 7.6 a–c Patient with frontal headaches in the region of the right frontal sinus, with extensive pneumatization of both frontal sinuses.
a Plain radiograph, Caldwell. It is difficult to evaluate the superior aspect of the frontal sinuses (1) to determine whether these are opacified or are limited in depth. A Waters view was not helpful in discriminating depth or opacification. The frontal recess on the right side (2) seems opacified compared with the left side (3). In the most lateral part of the right frontal sinus, some aeration still seems to be present (4).
b CT, coronal. Opacification of the right frontal sinus (1) is confirmed, with minimal central aeration (2). This case illustrates the point that opacification in areas of limited depth is difficult to evaluate on conventional radiography.
c CT, axial. Opacification (1) and partial aeration (2) of the right frontal sinus is seen. The anterior and posterior walls of the frontal sinus are intact. No calcifications are visible. An obstruction of the frontal recess may be present. In cases of failed endonasal approach, the frontal sinus and recess are easily accessible by an external approach because of sufficient length and depth of the sinus. Note: the right frontal sinus is compartmentalized by a bony septum, which may be removed for optimal drainage.
Differential Diagnosis
Nasal polyps, inverted papilloma, unilateral chronic odontogenic sinusitis with secondary polyps, unilateral fungal sinusitis, malignancy cystic fibrosis (commonly bilateral), foreign bodies (e.g. dental filling).
Points of Evaluation
• Destruction of bony outlines with infiltrative characteristics is suggestive of inverted papilloma, malignancies, or fungal infections.
• Calcifications in the opacified area are suggestive of fungal infections.
• History of frequent dental consultations and resorption of bone around tooth roots may indicate odontogenic infections.
• Long-term antibiotics are an essential part of postoperative treatment.

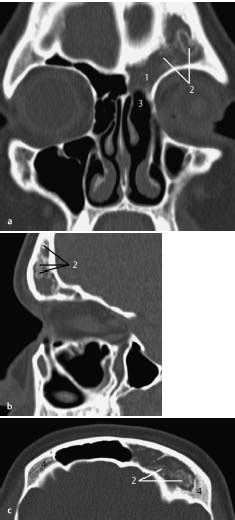
Fig. 7.7 a–c Patient with unilateral pain and pressure in the right maxillary region.
a Plain radiograph, Waters view. There is opacification of the right maxillary sinus (1) as well as in the region of the right ethmoid (2). The right frontal recess seems slightly opacified compared with the contralateral side (3). The left side demonstrates no opacification.
b CT, coronal. Opacification seen on CT confirms the findings in the maxillary sinus (1) and infundibulum (2). In addition, a thickened periosteal lining is observed, especially on the floor of the maxillary sinus (3). Just below this, the roots of a maxillary molar are visible (4) with signs of bone resorption, indicative of periapical infection. This is the most likely cause of the unilateral sinusitis.
c CT, coronal. After extraction of the offending tooth, opacification of the sinus (1) and symptoms persisted due to an oroantral fistula in the maxillary bone (2). Eventually, surgical closure of this fistula cured the problem. In such cases, endoscopic sinonasal surgery may facilitate recovery.
Differential Diagnosis
• All other causes of mucosal swelling and polyps, such as allergy.
• Less frequently: Wegener granulomatosis, which usually shows destruction of the nasal septum; and inverted papilloma or malignancy, often with infiltration of the surrounding bone and/or soft tissues, but rarely bilateral.
Points of Evaluation
• Destruction of bony outlines with infiltrative signs is more characteristic of malignancy.
• Expansion is more likely to be due to benign processes, such as polyposis or mucocele.
• Calcifications in the opacified area are suggestive of fungal infections.
• Resorption of bone around tooth roots indicates dental pulp infections.
• In children, expansion due to polyps can result in cosmetic problems of the exterior aspect of the nose.

Fig. 7.8 a–c Adult patient with known cystic fibrosis and frontal pressure feeling.
a CT, coronal. There is opacification of the right frontal sinus (1) with surrounding osteitic changes (2) such as increased thickness and sclerosis of the sinus walls. These signs are often seen in chronic infections, in particular with cystic fibrosis. In these patients, pneumatization of the frontal sinuses may be absent or limited, especially due to inflammation at an early stage during the development of the sinuses. Note the septal deviation.
Fig. 7.8b Patient with cystic fibrosis history of multiple endonasal surgical procedures.
b CT, coronal. There is complete opacification of the right maxillary sinus because of re-closure of the antrostomy to the middle meatus (1), probably by polyps. The opacified left maxillary sinus (2), although a wide open antrostomy to the middle meatus is observed, is suggestive of polyps and mucosal thickening as a result of chronic inflammation. This chronic inflammation is also evidenced by the osteitic changes in the walls of the maxillary sinus (3) and ethmoid (4).
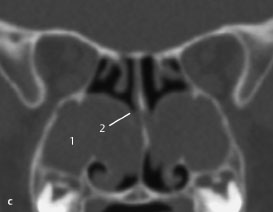
Fig. 7.8 c CT of a 12-year-old child with cystic fibrosis.
c CT, coronal. Complete opacification of both maxillary sinuses (1), probably due to polyps and stasis of mucoid secretions. Its chronicity is demonstrated by the pressure erosion of the medial wall (2). Endoscopy of the middle meatus should reveal these polyps.
Differential Diagnosis
All underlying causes of mucosal swelling and polyps, such as hyperreactivity, allergy, smoking. Rule out iatrogenic disorders due to extensive previous surgery. Post-traumatic lesions. Pott puffy tumor. Fistulization to the dura (cerebrospinal fluid leakage).
Points of Evaluation
• Sinusitis of the maxillary sinus, which is unresponsive to antibiotics or persists after long-term antibiotics, may be due to fungal infection. Usually, fungal infections affect the maxillary sinus. Less frequently, the frontal sinus is affected.
• Immunosuppressed patients (those with diabetes, human immunodeficiency virus [HIV] infection, or leukemia, and those taking immunosuppressive medication) are at increased risk of fungal infections.
• Opacification with general or focally increased density is suggestive of fungal infection.
• Diffuse infiltration of surrounding structures is seen in some invasive fungal infections (see also “Invasive Fungal Sinusitis,” p.240).
Fig. 7.9 a–c Patient with constant left frontal sinus pressure. CT, coronal (a), sagittal (b), and axial (c).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree