5 Pathology of the Skull Base
Pathology of the Middle Skull Base
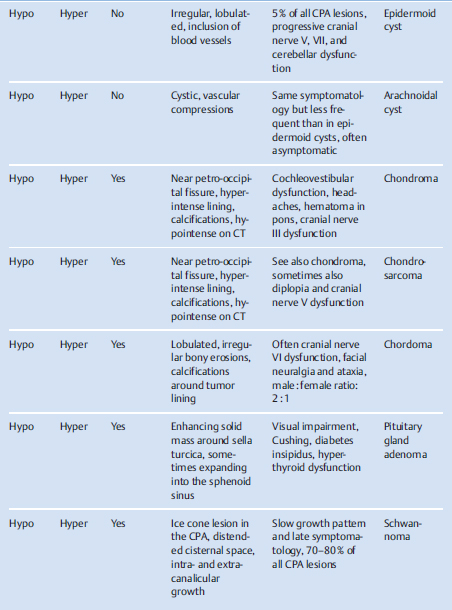
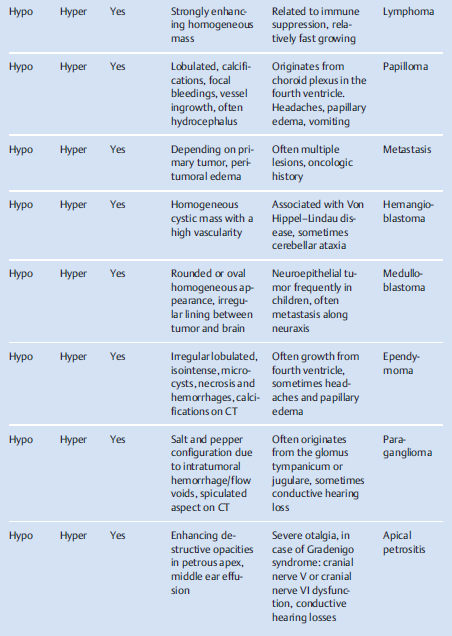
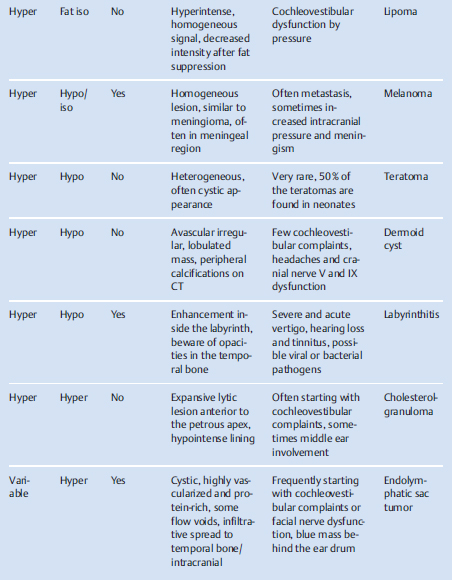
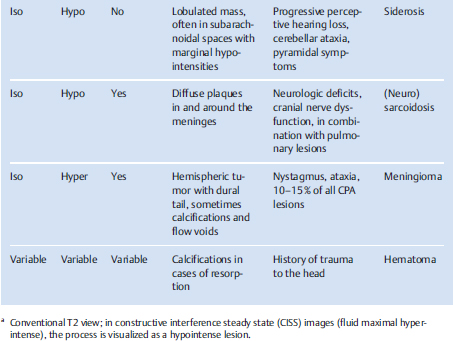
Lesions in the cerebellopontine angle (CPA) may be evaluated as shown in Table 5.1, according to intensity (T1/T2-weighted), contrast enhancement, and commonly occurring or characteristic radiologic features. Then, in combination with the clinical symptoms, the most likely diagnosis can be made. Note that Table 5.1 is not comprehensive and variations in presentation maybe seen. A variety of CPA pathologies will be discussed in this chapter.

Pseudotumors in the Apex of the Petrous Bone
Differential Diagnosis
Hemangioma, cholesterol cyst (granuloma), cholesteatoma, epidermoid, and lymphangioma.
Points of Evaluation
• Pseudotumors of the petrous apex are often found incidentally owing to normal variations in anatomy. It is important to be aware of their harmless nature and to reassure the patient.
• Hemangiomas demonstrate a salt and pepper configuration, although they are rare in the petrous apex.
• A cholesterol cyst (granuloma) is hyperintense on T2-weighted images due to mucus stasis, and hyperintense on T1-weighted images due to hemorrhagic changes with possible contrast enhancement of the capsule and expansive characteristics.
• Cholesteatoma appears less bright on T1-weighted images.
• Epidermoids demonstrate hypointense T1- and hyperintense T2-weighted signal intensity.
• For lymphangioma, see separate section.
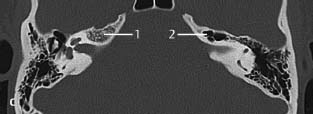
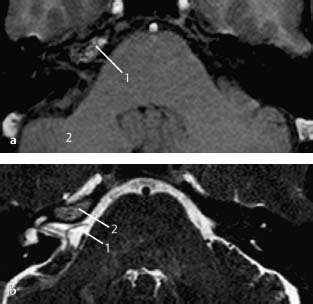
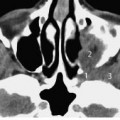
Fig.5.1 a–c Patient with tinnitus, who was referred from another hospital with a mass in the region of the right petrous apex.
a MRI, T1-weighted, axial. T1-weighted image shows that the lesion (1) has high signal intensity compared with brain tissue (2). The contralateral petrous apex has low signal intensity. With gadolinium administration (not shown) no enhancement was seen.
b MRI, T2-weighted, axial. On this heavily T2-weighted image, fluid (for example the cerebrospinal fluid [1] in the cerebellopontine cistern) has high signal intensity. The lesion (2) has slightly higher signal intensity than the brain tissue but not as high as fluid. Combined with the information from the T1-weighted image, this is a classic case of a pseudotumor due to asymmetric pneumatization of the petrous apex. The right petrous apex contains fatty marrow (high signal intensity on T1-weighted images), whereas the pneumatized contralateral apex only contains air with low signal intensity on both T1- and T2-weighted images.
c CT, axial. CT of the same patient confirms the difference in pneumatization and, in particular the aeration, of the petrous apex. Note: Normal bone marrow is present in the right petrous apex (1). Pneumatized petrous apex on the left side (2).
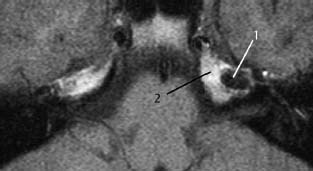
Fig. 5.2 Patient with perceptive hearing loss on the left side. Evaluation was done to exclude retrocochlear pathology.
MRI, T1-weighted, axial. A lesion (1) in the petrous apex on the left side. This type of lesions that appear black on T1-weighted sequences with or without contrast, as well as on T2-weighted sequences are indicative of bone or aerated petrous cells. On this image, the (remaining) petrous apex is filled with fatty marrow (2).
Schwannoma of the Internal Auditory Canal
Differential Diagnosis
Vestibular schwannoma, facial schwannoma, vascular tumors, inflammatory processes such as meningitis, neuritis, and gummas. Rare: meningioma, lipoma, metastases, lymphoma.
Points of Evaluation
• Vestibular schwannoma is the most frequent pathology (90%) found in this area. The clinical presentation facilitates the diagnosis because of hearing problems (vestibulocochlear).
• Multiple cranial nerve deficits are suggestive of inflammatory processes.
• A meningioma with the internal auditory canal as its only location and site of origin is possible but extremely rare; these tumors are usually CPA lesions protruding into the canal. In cases of a suspicious lesion in the CPA, MRI with contrast enhancement is recommended.
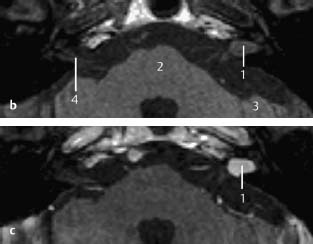
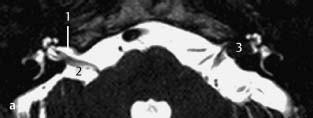
Fig. 5.3 a–c Patient with slowly progressive left-sided sensorineural hearing loss.
a MRI, T2-weighted, axial. On this T2-weighted image, the cerebrospinal fluid has very high signal intensity. Normally, the internal auditory canal (1) and cerebellopontine angle/cistern (2) are filled with cerebrospinal fluid, whereas neural structures (i.e., vestibulocochlear and facial nerves) are seen as hypointense structures. The inner ear also displays high signal intensity due to the presence of fluid in the inner ear. However, in this patient a mass is present on the left side (3) in the internal auditory canal, which is partially obscuring the normal fluid contents, with some remaining fluid in the fundus of the inner ear. The contours are smooth, suggestive of a benign space-occupying lesion.
b MRI, T1-weighted, axial. This T1-weighted image shows the lesion located in the left internal auditory canal, which is isointense to the brainstem (2) and cerebellum (3). Normal contents of the internal auditory canal (4) are less well visualized compared with the T2-weighted sequence. Compare with Fig. 5.3 a.
c MRI, T1-weighted with gadolinium enhancement, axial. Although the presence of a schwannoma in this region is highly likely, the use of gadolinium helps to confirm the diagnosis because schwannomas typically show strong homogeneous enhancement (1).
(For differential diagnosis and points of evaluation, see Cochlear Schwannoma.)
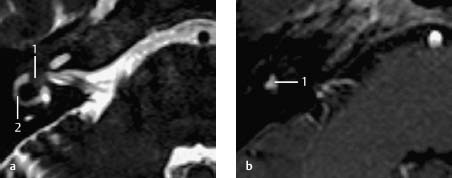
Fig. 5.4 a,b Patient with hearing deficits on the right side and nonspecific vertigo.
a MRI, T2-weighted, axial. A partial lack of fluid in the vestibule and horizontal semicircular canals is evident (1). A mass lesion is present in the vestibule. The status of the horizontal semicircular canal is unclear since it there is only reduced fluid content, as shown by its lowered signal intensity (2) and no definite mass.
b MRI, T1-weighted with gadolinium enhancement, axial. There is strong enhancement of the vestibule (1), which is highly suggestive of a vestibular schwannoma. The horizontal canal does not show any enhancement. A clear explanation of the hearing deficits could not be provided in this patient, since there was no involvement of the fundus.
Differential Diagnosis
Besides a high chance of schwannomas: inflammatory or immunological processes, secondary calcifications, congenital deformities of the inner ear.
Points of Evaluation
• Subtle and diffuse enhancements are also suggestive of active immunologic pathologies or intralabyrinthine infections.
• Fibrosis or ossification may occur over a period of months, excluding the possibility of cochlear implantation in bilateral deafness.
• CT may be able to differentiate between intraluminal fibrosis and ossification.
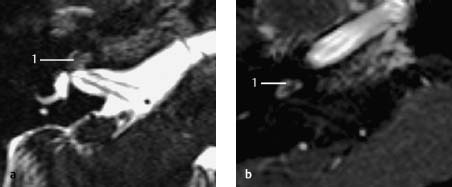
Fig. 5.5 a,b Patient presenting with sudden deafness on the right side.
a MRI, T2-weighted, axial. MRI is a standard investigation in sudden deafness and revealed lack of fluid inside the cochlea (1). The vestibular parts of the inner ear and the of infection clinically as well as on laboratory internal auditory canal were normal.
b MRI, T1-weighted with gadolinium enhancement. The entire cochlea shows slight enhancement (1). Since there were no signs of infection clinically as well as on laboratory testing, the findings are highly suggestive of an intracochlear schwannoma.
Schwannoma of the Cerebellopontine Angle
Differential Diagnosis
Vestibular schwannoma, facial schwannoma, vascular tumors, inflammatory processes such as meningitis, neuritis, and gumma. Rare: lipoma, metastases, lymphoma.
Points of Evaluation
• A vestibular schwannoma is the most frequent pathology (90%) in this area. Its initial clinical presentation will help to determine the origin of the lesion, that is of hearing problems (vestibulocochlear) or facial paresis.
• Meningioma may show the so-called dural tail, although this is not always present, and involvement of the internal auditory canal is less common.
• Epidermoid cysts have a more rounded appearance, with contents which may also be hyperintense on T1-weighted images, but show lack of enhancement after contrast administration.
• Arachnoid cysts in the CPA may be confused with cystic tumors.
• Anterior localization may also indicate a trigeminal neurinoma.
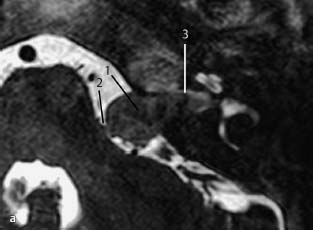
Fig. 5.6 a,b Patient with slowly progressive unilateral perceptive hearing loss.
a T2-weighted MRI, axial. Lesion of moderate size (1), partly within the internal auditory canal, and partly in the CPA, just touching the brainstem (2). Although the lateral part (fundus) of the internal auditory canal is not clearly filled with fluid, some still seems to be present (3) with the tumor restricted to the medial part of the canal.
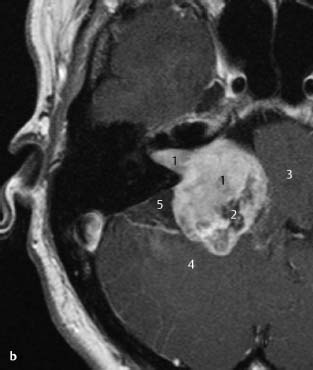
Fig. 5.6 b Patient presenting with subacute unilateral deafness.
b MRI, T1-weighted with gadolinium enhancement, axial. Example of a more extensive vestibulocochlear schwannoma. The enhancing tumor is filling the internal auditory canal with a large extension into the CPA (1). Due to the strong enhancement and location of the tumor, the findings are highly suggestive of a vestibulocochlear schwannoma. Nonenhancing areas (2) most probably represent cystic degeneration, which is often found in larger schwannomas. Note the compression of the brainstem (3) and cerebellum (4). A subtle dural tail sign is present, which is more characteristic of meningioma. Posteriorly, an arachnoid cyst may be present (5); this occasionally is the result of an accumulation of cerebrospinal fluid due to occlusion and mass effects by the tumor.
Fig.5.7 a–d This 9-year old boy with intellectual disability was seen by several otolaryngologists over many years, who ascribed the hearing losses to retraction pockets of the ear drum, until raised intracranial pressure caused neurological deficits.
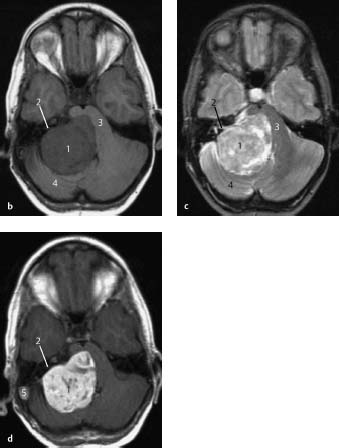
a T1-weighted MRI with gadolinium, coronal. Same schwannoma (1) with some cystic components, this image shows its superior extension and the severe compression and displacement of the brainstem (2). The dilated ventricles (3) indicate hydrocephalus due to obstruction with loss of the normal cortical appearance (4).
Fig.5.7b–d MRI, T1-weighted (b), T2-weighted (c), and T1-weighted with gadolinium enhancement (d), axial. Huge mass in the CPA (1) hypointense on T1-weighted imaging, mainly hyperintense on T2-weighted imaging, with gadolinium enhancement. No contrast enhancement is observed in the internal auditory canal. Although this is less typical of a schwannoma, it does not exclude this diagnosis because of its characteristics and rounded appearance. There is severe compression of the brainstem (3) and cerebellum (4) and enhancement of the contents of the right sigmoid sinus (5) which, in combination with the hyperintense T1-weighted image, is suggestive of sigmoid sinus thrombosis.
Differential Diagnosis
Epidermoid cysts, cholesterol granuloma, cystic vestibular schwannoma. Rare: cysticercosis, congenital cysts.
Points of Evaluation
• Epidermoid cysts, which are also hypointense on T1-weighted sequences and hyperintense on T2-weighted sequences, can be differentiated with diffusion-weighted imaging (DWI).
• In contrast, lipomas are hyperintense on T1-weighted images and hypointense on spin-echo T2-weighted sequences.
• Cysticercosis is seen in endemic areas, and the lesions are often smaller in size.
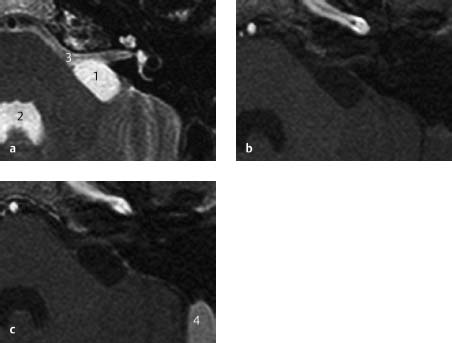
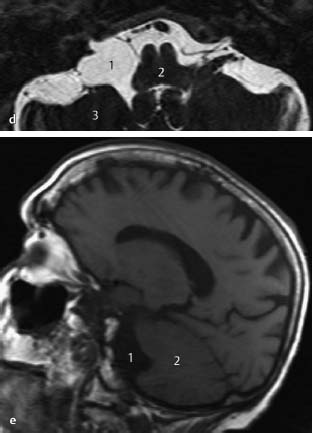
Fig.5.8 a–e Patients evaluated for complaints of disabling tinnitus.
a-c MRI, T2-weighted (a), T1-weighted (b), and T1-weighted with gadolinium enhancement (c), axial. There is a smooth-bordered ovoid lesion (1) in the CPA, just posterior to the internal meatus of the internal auditory canal. The signal intensity of this lesion is comparable with the fluid in the fourth ventricle (2) and cerebellopontine cistern (3) on both the T2- and the T1-weighted images. On T1-weighted imaging with gadolinium enhancement, the sigmoid sinus enhances (4) but there is no enhancement of the lesion. On the basis of these image characteristics, the differential diagnosis is restricted to an arachnoid cyst. Arachnoid cysts may compress structures, resulting in neurologic deficits, but an exact relation with the clinical symptoms remains unclear in most cases.
d MRI, T2-weighted, axial. Arachnoids cysts are frequently asymptomatic and noted as incidental findings on CT or MRI. They can be difficult to diagnose because of similar intensity of the cyst contents and the surrounding cerebrospinal fluid, as demonstrated in this figure on the right side (1): there is some asymmetry of the brain stem (2) and cerebellum (3) on the two sides, probably due to minor compression.
e MRI, T1-weighted, sagittal. Same patient as in Fig. 5.8d. The right-sided arachnoid cyst (1) is compressing the cerebellum (2) anteriorly. The lesion does not have solid components, as is sometimes seen in schwannomas with cystic degeneration (shown elsewhere).
Differential Diagnosis
Arachnoid cyst, cholesterol granuloma, cystic schwannoma, vascular tumors (hemangioma, endolymphatic sac tumor). Rare: cysticercosis, dermoid and congenital cysts.
Points of Evaluation
• Epidermoid cysts can be differentiated from other pathologies, such as arachnoid cysts, with DWI. Arachnoid cysts and other water-containing cysts and tumors have low signal intensity on DWI.
• On MRI, lipomas are hyperintense on T1-weighted and hypointense on T2-weighted sequences.
• Cysticercosis is seen in endemic areas and the lesions are often smaller in size.
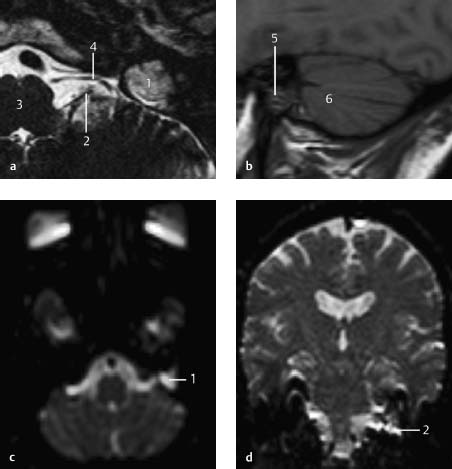
Fig.5.9 a–d Patient with progressive and asymmetrical perceptive hearing loss.
a, b MRI, T2-weighted, axial (a) and T1-weighted, sagittal (b). MRI revealed a small fundal schwannoma in the left internal auditory canal (not shown). However, on lower slices of the T2-weighted image, a hyperintense lesion in the skull base was observed as a coincidental finding (1). Note the glossopharyngeal and/or vagal nerves (2) arising from the brainstem (3), and the anterior inferior cerebellar artery (4). On the T1-weighted image, the lesion is isointense (5) and located anterior to the cerebellum (6).
c,d Diffusion-weighted imaging. The lesion is hyperintense, as demonstrated in the axial view (1) and coronal view (2). This is typical of cholesteatoma and epidermoid cysts. Note: The bright lines on the coronal image at the border of the temporal lobe are probably an artifact.
Cholesteatoma with Intracranial Involvement
Differential Diagnosis
Lesions in the mastoid region of the skull base: congenital or acquired cholesteatoma, epidermoid and dermoid cysts, mucocele, endolymphatic sac tumor, inflammatory or autoimmune lesions, meningo(encephalo)cele, meningioma.
Points of Evaluation
• Epidermoid cysts and cholesterol granulomas are more frequently located in the petrous apex.
• Endolymphatic sac tumor originates in the region between the posterior semicircular canal and the middle cranial fossa and sigmoid sinus, with typical imaging patterns (see separate sections).
• A meningo(encephalo)cele or meningioma demonstrates osseous destruction in the middle or posterior skull base, as well as continuity with the dural or intracranial structures.
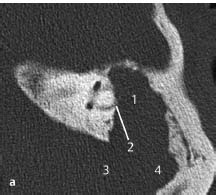
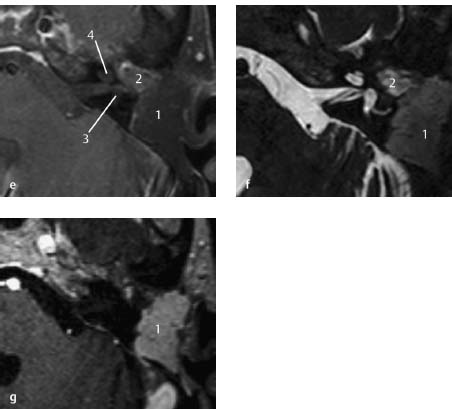
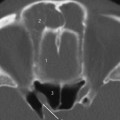
Fig.5.10 a–g Patient with chronic otitis media with purulent discharge.
a CT, axial. The middle ear was fully opacified with destruction of the ossicular chain. In this slice, the opacification of the epitympanic and mastoid spaces (1) is suggestive of a mass, with erosion of the horizontal semicircular canal (2) and bony destruction toward the posterior cranial fossa (3) and sigmoid sinus (4).
b–d MRI, T1-weighted, (b), T2-weighted (c), and T1-weighted with gadolinium enhancement (d), axial. MRI shows better details of the characteristics and the relation of the lesion with the surrounding structures. The mass (1) is hypointense on T1-weighted and hyperintense on T2-weighted images. The capsule (2) shows gadolinium enhancement, and probably consists of highly vascularized granulation tissue due to chronic inflammation. These findings are consistent with a cholesteatoma in which the intralesional keratin shows no enhancement with gadolinium. In the posterior part of the lesion (3), some air is probably trapped, demonstrated by the lack of signal on all sequences. There is contact between the lesion and the horizontal semicircular canal (4), as seen in Fig. 5.10a (label 2).
e–g MRI, T1-weighted, (e), T2-weighted (f), and T1-weighted with gadolinium enhancement (g), axial. Same patient as demonstrated on the previous figures, 5 years after surgical removal of the cholesteatoma by subtotal petrosectomy, closure of the external auditory canal, and obliteration of the cavity by abdominal fat. The abdominal fat is filling the cavity (1). Anteriorly, on the T1- and T2-weighted images, a slight hyperintense lesion (2) is observed, which may be a residual cholesteatoma. The inner ear structures with their fluid contents are best visualized on the T2-weighted image; there is partial destruction of the horizontal semicircular canal (3) but the cochlea is intact (4).
Cystic Degeneration in CPA Schwannoma
Differential Diagnosis
Arachnoid cyst, mucocele, hemangioblastoma.
Points of Evaluation
• An arachnoid cyst may be secondary to folding or inclusion of arachnoid membranes by compression from a schwannoma or meningioma. They are mostly located outside the margin of the causative lesion.
• A mucocele may be considered when the cyst is in located in a structure covered by mucosa.
• Although a hemangioblastoma only rarely presents as a CPA lesion, it may undergo rapidly progressive and massive cystic degeneration with partial enhancement of its solid parts, as is frequently observed in Von Hippel-Lindau disease.
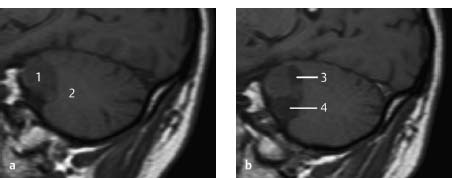
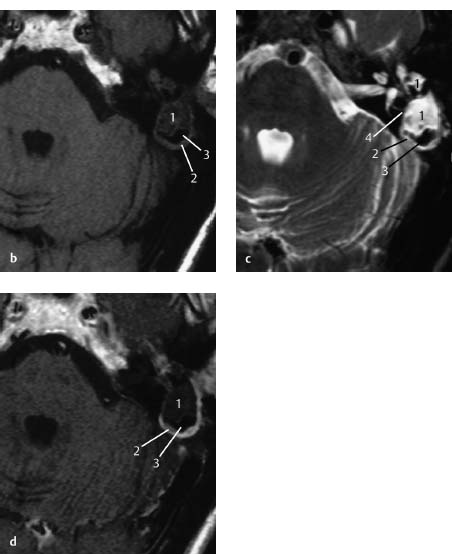
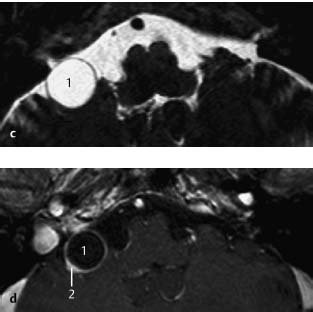
Fig.5.11 a–d Patient with a vestibular schwannoma evaluated by a wait-and-see policy.
a,b MRI, T1-weighted, sagittal. The left image shows a schwannoma (1) of the CPA with minor compression of the cerebellum (2). In the right image, 1 year after a wait-and-watch policy, the lesion has expanded rapidly due to cystic changes in the posterior cranial (3) and caudal (4) regions, while the primary (solid) part of the schwannoma has not enlarged in size.
c,d MRI, T2-weighted (c) and T1-weighted with gadolinium enhancement (d), axial. A caudal slice (left) demonstrates a round cystic lesion (1) with a thin capsule. The signal intensity is identical to the surrounding cerebrospinal fluid. No solid parts are visible at this level. To prevent misinterpreting the lesion as an arachnoid cyst, continuity of this cystic area with the solid part of the schwannoma should be established on adjacent sections. With gadolinium, the cystic part of the lesion is not enhanced (1), while in the solid parts enhancement is observed (2). Although there are therapeutic options available for rapidly expanding lesions, predicting their effect preoperatively remains difficult.
Effects of Radiotherapy on CPA Schwannoma
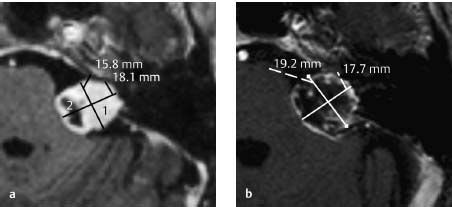
Fig.5.12 a,b Patient with a growing vestibular schwannoma treated with fractionated stereotactic radiotherapy.
a MRI, T1-weighted with gadolinium enhancement, axial. In an attempt to preserve residual hearing, the patient opted for fractionated stereotactic radiotherapy. Prior to treatment, a solid, enhancing tumor in the CPA (1) with a small cyst (2) was observed.
b MRI, T1-weighted with gadolinium enhancement, axial. After radiation therapy, the patient’s symptoms worsened, and repeat MRI showed some enlargement and severe vacuolization of the tumor. These signs are often encountered shortly after radiotherapy, but with time, the tumor shrinks because of fibrosis. The chances of preservation of hearing are difficult to determine before treatment.
Differential Diagnosis
Multiple lesions and involvement of organs are also seen in Von Hippel-Lindau disease and inflammatory disorders such as sarcoidosis and syphilis.
Points of Evaluation
• Neurofibromatosis may initially present as otologic deficits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree