- •
The assessment of patients with new-onset stable chest pain includes a detailed history assessment and ECG.
- •
The current risk scores tend to overestimate the risk for CAD in patients with stable chest pain syndromes.
- •
In low-risk patients, exercise ECG and coronary CT angiography are excellent noninvasive approaches for evaluating patients with chest pain. The absence of plaque by coronary CT angiography has a very high negative predictive value for excluding the presence of obstructive CAD.
- •
In patients with intermediate to high clinical risk, radionuclide imaging (SPECT and PET) can be useful to delineate the extent and severity of myocardial ischemia. The use of quantitative myocardial blood flow with PET provides one of the most accurate noninvasive means for the evaluation of patients with suspected ischemic heart disease.
- •
The presence of normal coronary flow reserve on PET is associated with a very low likelihood of high-risk anatomy, multivessel disease, or left main disease.
- •
The addition of the CAC score to myocardial perfusion imaging helps to identify high-risk patients who otherwise have normal myocardial perfusion imaging.
Introduction
Chest pain remains one of the most common patient complaints both at the primary care level and in the specialized cardiology clinic. According to the American Heart Association’s heart disease and stroke statistics, 635,000 Americans have a new coronary event every year, of which 20% are silent myocardial infarction. Chest pain is also the most frequent chief complaint in the emergency room, causing more than 8 million visits a year (see discussion in Chapter 11 ). The evaluation of patients with chest pain is important and requires a detailed approach that takes into account multiple considerations, including the typicality of symptoms, pretest likelihood of coronary artery disease (CAD), and strengths and limitations of the ancillary tests used in the diagnostic workup. In this chapter, we discuss the role of radionuclide imaging in the assessment of patients with new-onset stable chest pain. We will focus on the role of single photon emission computed tomography (SPECT) and positron emission tomography (PET) in the evaluation of these patients. The value of alternative approaches to diagnosis, especially exercise treadmill testing (ETT) and cardiac computed tomography (CT), will also be discussed.
Initial assessment of patients with new-onset chest pain
The aim of the management of patients with stable chest pain in the clinic is to determine the likelihood of CAD and confirm the diagnosis via further testing. Thus the initial evaluation of these patients would include a history and physical examination to identify signs and symptoms of obstructive CAD.
In addition, an electrocardiogram (ECG) may guide the disposition of these patients. For example, the presence of ischemic changes or abnormal Q waves on the ECG would increase the likelihood of CAD and may prompt referral for noninvasive testing and, sometimes, direct coronary angiography.
The analysis of probability as an aid to the diagnosis of obstructive CAD in stable symptomatic patients has been standard practice in cardiology for many decades. Multiple CAD probability scores integrating age, sex, chest pain characteristics, and coronary risk factors have been proposed for the assessment of patients with stable chest pain syndromes. A strong evidence base has demonstrated that noninvasive imaging testing for obstructive CAD is most cost effective when applied to patients with an intermediate likelihood of CAD and is recommended by guidelines. These include the Diamond-Forrester risk score, the CONFIRM (COroNary CT Angiography Evaluation For Clinical Outcomes: An InteRnational Multicenter Registry) risk score, and the PROMISE (Prospective Multicenter Imaging Study for Evaluation of Chest Pain) risk score. Nevertheless, the predictive value of these scores is often dependent on the population the score is derived from, as well as the population it is applied to. Recent data suggest that CAD probability scores overestimate the risk and prevalence of CAD. For example, in the PROMISE trial, the prevalence of CAD as determined by coronary CT angiography or abnormal myocardial perfusion imaging (MPI) was significantly lower than predicted by the pretest score. Similarly, a study from the CONFIRM registry also showed that the prevalence of CAD was overestimated by the Diamond-Forrester risk score compared with the prevalence of CAD by coronary CT angiography. Part of the problem is that these scores have been validated in cohorts of patients referred for invasive coronary angiography or coronary computed tomography angiography (CCTA), which overestimates the prevalence of CAD, thereby increasing the sensitivity and decreasing the specificity of CAD probability scores. This overestimation of CAD probability may explain the relatively lower frequency of abnormal studies in recent reports. , It is important to keep in mind that as the prevalence of disease in the studied population decreases, the negative predictive value increases and the positive predictive value decreases (because of an increase in false-positives). This applies to both the CAD probability scores and imaging tests.
Incremental value of imaging tests
Exercise ECG remains an important test in the assessment of patients with stable chest pain syndrome, especially those with a normal baseline ECG. It is the initial modality recommended by the American College of Cardiology and American Heart Association guidelines for assessing patients with stable ischemic heart disease. It provides valuable information regarding exercise capacity and cardiorespiratory fitness, , thus providing important diagnostic and prognostic information that is useful in guiding management. More notably, the presence of chronotropic incompetence has been associated with a worse long-term outcome and hypertensive response during exercise has been associated with increased incidence of future comorbidities, including new incident hypertension. The Duke treadmill score can also be calculated using data gathered from the stress test and has widely recognized prognostic value. Nevertheless, exercise ECG has lower overall accuracy compared with functional and anatomic imaging tests. A meta-analysis including more than 24,000 patients with 22 years of follow-up has shown that stress ECGs have a sensitivity of 68% and specificity of 77% for the diagnosis of obstructive CAD.
Given the limitations of exercise ECG, further testing with imaging is often needed in different clinical scenarios including patients with
- •
Equivocal exercise electrocardiography;
- •
Abnormal resting ECGs, including left bundle branch block (LBBB) and left ventricular (LV) hypertrophy with repolarization abnormalities; and
- •
Certain populations where ECG ischemic changes may be falsely positive rather than indicative of obstructive CAD, such as in young women.
Diagnostic value of radionuclide imaging
SPECT imaging is the most commonly used stress imaging test for CAD diagnosis in the United States. Overall, the sensitivity and specificity for detection of obstructive CAD ranges between 75% and 85%. A limitation of SPECT MPI is that the test often uncovers only myocardial regions supplied by the most severe coronary stenosis. This can lead to underestimation of the extent of CAD, especially in high-risk patients with multivessel CAD. An important advantage of PET MPI is its unique ability to provide absolute measures of myocardial blood flow and flow reserve, which allows for improved delineation of flow-limiting CAD and also microvascular dysfunction. Recent meta-analyses , and the prospective multicenter EVINCI (Evaluation of Integrated CAD Imaging in Ischemic Heart Disease) study support the diagnostic advantage of PET. Furthermore, a recent meta-analysis using fractional flow reserve (FFR) as the gold standard for flow-limiting CAD demonstrated higher diagnostic accuracy for PET compared with SPECT MPI. Finally, the results of the PACIFIC (Prospective Comparison of Cardiac PET/CT, SPECT/CT Perfusion Imaging and CT Coronary Angiography With Invasive Coronary Angiography) study confirmed the superiority of quantitative PET MPI for the detection of flow-limiting CAD, including the combination of CCTA with and FFR derived from standard coronary CT angiography (FFR CT ).
A detailed discussion of stress testing and imaging protocols used with SPECT and PET imaging can be found in Chapter 4 , and common artifacts that may challenge image interpretation can be found in Chapter 5 .
Added value of coronary artery calcium score
The coronary artery calcium (CAC) score can be generated from gated noncontract chest CT. It has been extensively evaluated in multicenter studies and prospective registries. , The presence of coronary artery calcifications has been associated with an increased incidence of cardiovascular events and new incidence of CAD. Recent studies have suggested that adding the calcium score to MPI (both SPECT and PET) may improve its diagnostic accuracy and prognostic value. ,
Applications of radionuclide imaging in patients with new-onset stable chest pain syndrome
Case vignette 1: Assessment of a symptomatic low-risk patient
A 40-year-old female who has had human immunodeficiency virus (HIV) infection for 7 years presented to the cardiology clinic complaining of chest pain that is retrosternal, intermittent, lasting for a few minutes, and resolving on its own. The pain is not exertional but has been recurrent and concerning to the patient. She has no other comorbidities. Her lipid profile has been under good control with pravastatin 20 mg once daily. Her low-density lipoprotein cholesterol is less than 70 mg/dL. She is concerned about the chest pain, which prompted two prior emergency room visits. In both emergency room visits, she had a normal ECG and negative biomarkers.
Given her HIV infection and the recurrence of symptoms necessitating two emergency room visits, the patient was referred for pharmacologic PET MPI testing (primarily to reduce her radiation exposure, given her young age). The rest and regadenoson-stress 82 rubidium ( 82 Rb) myocardial perfusion images were normal ( Fig. 7.1 A). Her rest LV ejection fraction was normal at 67%. The rest and hyperemic myocardial blood flows and the coronary flow reserve were normal both regionally and globally (see Fig. 7.1 B).

The presence of normal stress myocardial blood flow and flow reserve excluded flow-limiting CAD and coronary microvascular dysfunction as potential sources of chest pain. It was suggested that the patient’s symptoms may be because of gastroesophageal reflux disease given the presence of a small hiatal hernia on the attenuation-correction CT scan. She was referred to gastroenterology who confirmed the diagnosis and started her on proton pump inhibitors with a significant improvement in her symptoms. The patient also agreed to participate in a research study where she had CAC scoring, as well as CCTA. Her CAC score was 0 and her CCTA did not show any noncalcified coronary plaque in her coronary vasculature (see Fig. 7.1 C).
This case illustrates the different options available for evaluating patients with stable chest pain. Currently, multiple tools can be used in the assessment of these patients, including clinical risk scores and high-sensitivity biomarkers such as troponin. In this patient, the clinical risk score suggested low risk of obstructive CAD. Nevertheless, her multiple episodes of chest pain and her HIV status promoted further investigations.
In this specific patient population with low pretest likelihood of CAD, the main goal of assessment is to exclude significant CAD. A test with high negative predictive value in the lower-risk population is usually appealing. Coronary CT angiography is now more widely available and is becoming an attractive tool in this patient population because of its high negative predictive value, which can reliably exclude the presence of obstructive CAD. In addition, a CAC score has been suggested as a good alternative in these patients. Indeed, a calcium score of 0 has been associated with a very low prevalence of significant CAD. , Nevertheless, the concern about the presence of noncalcified plaque that is not detected by the noncontrast CT scan used to measure CAC remains a limitation, especially in young patients who are unlikely to show significant calcified coronary plaque.
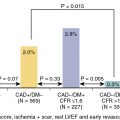
The relative utility of strategies using coronary CT angiography or ischemia testing as an initial test in symptomatic low-intermediate risk patients was studied in the PROMISE trial. Approximately 10,000 patients with stable chest pain were randomized to a strategy of initial anatomic testing with the use of CCTA or to functional testing (exercise ECG, nuclear stress testing, or stress ECG). The primary end point was the occurrence of all-cause mortality, myocardial infarction, hospitalization for unstable angina, or major procedural complication. Although the mean pretest likelihood of obstructive CAD was 53 ± 21%, the prevalence of positive studies was low in this population (10.7% in the CCTA group and 11.7% in the ischemia testing group; Fig. 7.2 ). Similarly, the event rate at a median follow-up period of 25 months was low in both groups (3.3% in the CCTA group and 3% in the ischemia testing group, P = 0.75; see Fig. 7.2 ). Compared with the ischemia testing group, the coronary CCTA–based strategy was associated with a higher catheterization rate within 90 days after randomization (8.1% vs. 12.2%) without significant differences in the presence of obstructive CAD. Thus, this landmark trial suggests that the choice of the initial test for the assessment of patients with stable chest pain does not seem to affect the outcomes of these patients.

Case vignette 2: Assessment of a symptomatic low-risk patient who can exercise
A 49-year-old man with a history of essential hypertension presented with chest pressure that was recurrent and lasting for a few minutes. The patient had no other comorbidities. The ECG revealed normal sinus rhythm and nonspecific ST-T wave abnormalities. The patient underwent a SPECT MPI study using a stress-first protocol (see Chapter 4 ). He exercised for 13:04 minutes of a Bruce protocol and achieved a maximal heart rate of 171 beats per minute, which is almost 100% of his maximal predicted heart rate (15.4 metabolic equivalents). Exercise was stopped because of fatigue and because he did not complain of chest pain. His blood pressure response was normal. His Duke treadmill score was 13, which has low prognostic risk. At peak exercise, the patient was injected with 16 mCi of 99m Tc tetrofosmin and was imaged 30 minutes postinjection. The stress myocardial perfusion images were normal, which avoided the need for rest imaging ( Fig. 7.3 ). The poststress LV ejection fraction was 59% with normal regional wall motion and thickening.