Hip disorders are a wide range of conditions commonly affecting patients in the pediatric age group. Reaching an accurate diagnosis of these conditions in children may be challenging. The optimal use of image modalities in the approach of a child with possible hip pathology is essential, which allows radiologists and clinicians to narrow the differential diagnosis and reach a definitive diagnosis, which can consequently result in early and appropriate interventions leading to improved outcomes. Therefore, this article aims to provide practicing radiologists and clinicians with up-to-date and evidence-based imaging spectrum guidelines and recommendations for common pediatric hip disorders.
Key points
- •
Ultrasound is the imaging modality of choice for the detection of joint effusion.
- •
Developmental dysplasia of the hip screening is recommended only to children older than 4–6 weeks with risk factors or abnormal physical examination.
- •
MR imaging is recommended when radiography and ultrasound fail to identify a specific disorder.
Introduction
Hip disorders are common in the pediatric population. Affected children usually present with nonspecific symptoms such as pain and/or limp. Establishing an early diagnosis and treatment is crucial to avoid long-term complications such as growth disturbance and degenerative disease. Clinical history combined with physical examination and laboratory tests help in establishing a differential diagnosis. However, clinical and laboratory findings can overlap, making imaging evaluation crucial in the diagnosis. To date, there is a lack of evidence-based imaging approach to pediatric hip disorders. Therefore, the main purpose of this article is to provide: (1) up-to-date evidence-based imaging algorithm for diagnosing pediatric hip disorders; and (2) overview of imaging spectrum of common pediatric hip disorders with an emphasis on imaging recommendations and guidelines for practicing radiologists and clinicians managing pediatric patients with various hip disorders in daily clinical practice.
Imaging modalities
Radiography
Radiography is the initial image modality used for the assessment of hip disorder in pediatric patients. It is preferred to be used by imaging the whole pelvis rather than the hip unilaterally. This allows the comparison between both hips and the detection of bilateral disease. Radiography is used in anteroposterior (AP) and frog-leg position views because of the great variability of the hip according to different ages. In patients with clinical examination demonstrating an absence of localized disease, bilateral lower extremities radiography is preferred, whereas when a localized disease is detected, AP and lateral unilateral radiography is indicated.
Ultrasound
Ultrasound (US) is the imaging modality of choice for the evaluation of hip disorders in infants because of the unossified nature of their bony structures. It is useful in screening and diagnosing developmental dysplasia of the hip (DDH) in infants, diagnosing bursal and periarticular fluid collections and hip joint effusion, and guiding hip aspiration and injections. If hip effusion is suspected, US is more sensitive than radiography and should be used first. In addition, US-guided aspiration should be performed if high clinical suspicion for septic arthritis (SA) is present.
MR Imaging
MR imaging is recommended when radiography and US fail to identify a specific disorder. MR imaging has a great sensitivity for the detection of early hip disorders in pediatric patients. Its greatest advantage is its ability to accurately demonstrate the presence of bone marrow edema, evaluate for acetabular cartilage and labral abnormalities, and to detect soft tissue inflammation and joint effusion. MR angiography (MRA) with intra-articular gadolinium injection provides a more accurate evaluation of the joint anatomy and pathologies affecting the acetabular labrum and articular cartilage. It is mainly used for the assessment and follow-up of DDH, diagnosis of slipped capital femoral epiphysis (SCFE) and osteomyelitis, diagnosis and staging of LCPD, diagnosis of radiologically occult traumatic and stress-related bone injuries and tumor staging.
Bone Scintigraphy
Bone scintigraphy is indicated when US radiography failed to detect pathology and MR imaging is contraindicated or not available. It is used for the evaluation of osteomyelitis, Legg-Calve-Perthes disease (LCPD), osteoid osteoma (OO), stress fractures, and metastatic disease. Its major disadvantage is the radiation exposure, poor anatomic details, and its nonspecific nature.
Evidence-based imaging algorithm
A meta-analysis by the American Academy of Family Physicians (AAFP) provides key recommendations for imaging and management of limping children with a C evidence rating indicating consensus and disease-oriented evidence :
- 1.
Plain radiography is recommended in limping pediatric patients with no localized pathology on physical examination.
- 2.
Anteroposterior and lateral radiography is recommended when localized pathology is detected on physical examination.
- 3.
If joint effusion is suspected, ultrasound (US) is recommended because of its high sensitivity.
- 4.
In patients with normal or equivocal physical examination, radiography, US and bone scintigraphy are recommneded.
- 5.
The presence of elevated oral body temperature (>101.3°F), erythrocyte sedimentation rate (ESR; >40 mm/h), white blood cell (WBC) count (>12000/mm 3 ), or C-reactive protein (>20 mg/L) raises the suspicion of septic arthritis (SA) over transient synovitis (TS).
A diagnostic algorithm with the first imaging modality recommended in limping children with and without pain is provided in Fig. 1 .

The spectrum of neonatal and pediatric hip disorders
Congenital Pediatric Hip Disorders
Developmental dysplasia of the hip
Developmental dysplasia of the hip (DDH) consists of a wide spectrum of developmental abnormalities affecting the hip of infants and young children. It ranges in severity from abnormal acetabular morphology to hip dislocation. , Previously published studies have shown that female gender, third trimester breech position, positive family history, and prolonged postnatal swaddling are 4 main factors associated with increased risk for DDH. , The prognosis of DDH is proportionate to the severity of hip disorder at the time of diagnosis and treatment. Physical examination is the main screening method for DDH. , Although imaging evaluation plays a fundamental role in screening, the American Academy of Pediatrics (AAP), American Academy of Orthopedics (AAOS), and American College of Radiology (ACR) recommend against universal imaging screening for DDH.
Currently, selective imaging screening is recommended when an infant has risk factors or abnormal physical examination. , However, no screening imaging is recommended to neonates because studies have shown spontaneous resolution of radiological and physical abnormalities in the vast majority of cases. To avoid overtreatment and iatrogenic complications, AAP recommends only starting imaging screening in patients older than 4 to 6 weeks.
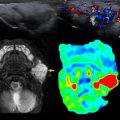
US is the initial imaging modality of choice for DDH evaluation in infants aged less than 6 months because, in contrary to radiography, it allows visualization of the nonossified femoral head (FH) and acetabulum. According to the Graf system, classification is made by evaluating maturity of bony acetabulum, degree of FH coverage by corresponding acetabulum, and determination of alpha angle. A normal hip has angular or slightly rounded acetabulum, a FH coverage greater than 50%, and an alpha angle greater than 60° ( Fig. 2 A). Stress maneuver may induce instability of FH ( Fig. 2 B, C).

In infants older than 4 months, anteroposterior (AP) pelvis radiograph with hips in neutral position is the preferred image modality to diagnose DDH complemented by frog-leg lateral view if any subluxation or dislocation is seen to determine reducibility. Radiographic evaluation includes measurement of acetabular index, size, and proper location of ossified FH. Proper position of FH is assessed by Perkins’s line and Shenton arc ( Fig. 3 ). In normal hips, the FH is located in the inferomedial quadrant formed by the intersection of the Perkins and H lines and Shenton arc is continuous (see Fig. 3 ). Radiographic characteristics of DDH consist of increased acetabular index for age, and/or delayed appearance or small ossified FH, and/or lateral and superior position of FH ( Fig. 4 ).

MR imaging has no role in screening or diagnosing DDH, as outlined by ACR. It is a robust tool for confirming concentric reduction independent of ossific FH or hardware artifact following closed hip reduction and Spica cast placement or open reduction/osteotomy and hardware placement. Concentric reduction is achieved when FH points toward corresponding triradiate cartilage in all planes ( Fig. 5 ). MR imaging allows identification of obstacles to concentric reduction which can be extra-articular (tightening of iliopsoas tendon) or intra-articular (limbus, labral inversion, enlarged pulvinar, and ligament hypertrophy). Following intravenous gadolinium, FH perfusion is assessed for geographic areas of hypoenhancement or global nonenhancement; only the latter has been associated with a high risk for osteonecrosis. Sedation is generally not necessary for postreduction MR imaging because residual sedation following anesthesia administered during surgical reduction is sufficient for diagnostic imaging.

In pediatric patients with delayed diagnosis of DDH, MR imaging is advocated in presurgical evaluation because it delineates FH morphology, femoral acetabular coverage, chondral surfaces, and labrum which help dictate timing for surgical intervention. MR arthrography (MRA) following intra-articular administration of gadolinium is indicated in patients with DDH-induced femoroacetabular impingement.
Similar to MR imaging, computed tomography (CT) plays no role in screening or diagnosis of DDH. Multidetector CT with 3-dimensional reconstruction can be used for preoperative planning and postoperative assessment of hip reduction. Because of its ionizing radiation and poor soft tissue details and because repeat imaging may be required if unsuccessful initial reduction, it is only obtained when MR imaging is contraindicated or not available.
Fluoroscopic arthrography is used intraoperatively to assess successful hip reduction and detect obstacles for hip reduction ( Fig. 6 ). More precise intraoperative localization can be obtained with cone-beam CT (O-arm), which adds cross-sectional imaging to fluoroscopic evaluation.

Meyer dysplasia (dysplasia epiphysealis capitis femoris)
Meyer dysplasia (MD), also known as dysplasia epiphysealis capitis femoris, is an asymptomatic rare condition characterized by delayed and irregular ossification of FH. It commonly affects both hips, more often in boys, with a mean age of 2.5years. Although MD requires no treatment, its accurate diagnosis is crucial because it is commonly mistaken for Legg-Calve-Perthes disease (LCPD) potentially resulting in unnecessary intervention.
In asymptomatic infants, MD is suggested radiographically by a small, irregular, or cystic FH, which resolves spontaneously after 2 to 4 years without subchondral fracture, collapse, or instability. MR imaging is used to differentiate MD from LCPD when a definitive diagnosis cannot be performed by radiography. The absence of marrow signal abnormality is the main finding excluding LCPD.
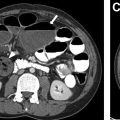
Proximal femoral focal deficiency
Proximal femoral focal deficiency (PFFD) is an uncommon congenital malformation characterized by partial or complete hypoplasia of proximal femur and abnormal development of the hip. PFFD occurs in 0.5 to 2 cases per 100,000 live births and is 90% unilateral. PFFD is 50% associated with other congenital lower extremity abnormalities with ipsilateral fibular hemimelia being the most common ( Fig. 7 A). Congenital short femur is related to PFFD, characterized by anterolateral bowing and shortening of the femur with valgus deformity of the knee. This condition is also associated with fibular hemimelia and foot deformities.

Radiography is obtained in infants after antenatal US detection of femur abnormality. Radiography allows characterization of PFFD by the Aitken classification into 4 groups (A to D) depending on the degree of proximal femoral deficiency and acetabular dysplasia (see Fig. 7 A). However, radiographs are unable to show non-ossified FH or fibrocartilaginous connections between FH and shaft for accurate classification of PFFD. Therefore, MR imaging and US are indicated for the determination of type and prognosis of PFFD.
MR imaging provides a more comprehensive evaluation for preoperative planning. It allows to determine which portion of the acetabulum is deficient (posterior in PFFD vs anterior in DDH), size of cartilaginous acetabulum and FH, and detection of subtrochanteric pseudoarthrosis, femoroacetabular impingement, and labral hypertrophy , ( Fig. 7 B). In congenital short femur, MR imaging evaluates the extent of hamstring shortening and absence of anterior cruciate ligament. Contrast-enhanced MRA is indicated to assess vascular anatomy when amputation or limb-salvage surgery is contemplated.
Developmental Pediatric Hip Disorders
Legg-Calve-Perthes disease
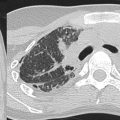
LCPD is idiopathic avascular necrosis of FH which results in cessation of growth. Boys are 5 times more likely affected than girls and 85% to 90% of cases are bilateral. Affected pediatric patients typically present with hip pain and/or limp between 3 and 12 years of age with peak incidence at 5 to 7 years. LCPD is a diagnosis of exclusion; other causes of osteonecrosis should be initially excluded.
Radiography is the imaging modality of choice for diagnosis, classification, and follow-up of LCPD. In the initial stage of LCPD (first 6 months), radiography can be normal or equivocal ( Fig. 8 A). AP radiograph with neutral and frog-leg lateral position of the hips are essential for the diagnosis and staging. Radiographic findings of early LCPD consist of apparent joint space widening and subchondral fracture, whereas the late radiographic findings consist of sclerosis, fragmentation, and subchondral collapse of the FH.