Anatomy, embryology, pathophysiology
- ◼
The pelvic floor consists of the levator ani, the pelvic sphincters, and fascia that support the rectum, bladder and urethra, as well as the vagina, cervix, and uterus in females and the prostate in males.
- ◼
These organs are divided into three compartments in females: anterior (bladder and urethra), middle (uterus, cervix, and vagina), and posterior (rectum and anus). In males, there is no middle compartment.
- ◼
Pelvic floor dysfunction is a broad term that includes dysfunction of any of the three compartments, including urinary incontinence, anal incontinence, defecation dysfunction, and pelvic organ prolapse.
- ◼
The risk of having at least one pelvic floor dysfunction in women of reproductive age is estimated to be at least 24% and as high as 46%, affecting a much smaller proportion of men.
- ◼
Approximately 10% of women undergo surgery for pelvic floor dysfunction.
- ◼
Fluoroscopic defecography (FDG) and magnetic resonance defecography (MDG), involving real-time relaxation of the levator ani and evacuation, contribute additional findings to physical examination in up to 65% of cases.
Techniques
Fluoroscopic defecography
FDG allows dynamic imaging of the pelvic floor and involves contrast opacification of the rectum and vagina with or without contrast opacification of the bladder and small bowel. Imaging is performed on a radiolucent commode and is therefore considered more physiological than other described techniques.
Magnetic resonance defecography
MDG offers similar benefits to FDG and provides additional anatomic information regarding the pelvic organs because of its high image contrast and triplanar imaging protocol; this allows easy identification of the pelvic organs, including the bladder, urethra, prostate, uterus, vagina, rectum, and anus and demonstration of their subsequent movement during defecatory maneuvers. MDG’s lack of radiation makes it the preferred imaging modality in younger patients. Open MRIs can also enable physiologic defecation positioning.
Translabial pelvic floor ultrasound
A relatively new, less established modality for the evaluation of pelvic floor disease in females, with high reported accuracy. This technique will not be covered in this chapter.
Protocols
Protocol considerations
Protocols for optimal evaluation of suspected pelvic floor dysfunction aim to image two or three compartments, depending on the gender and imaging protocol. Study of the pelvic floor involves dynamic imaging during provocatory maneuvers, including Kegel maneuvers, straining, and evacuation. Before any procedure, a detailed questionnaire inquiring about symptoms is important to reveal any previously unsolicited details that may be helpful in the diagnostic workup.
Suggested fluoroscopic defocography protocol
Organ and landmark opacification
- ◼
Perineum: tape a 1.3 cm Barium tablet in the perineum for both landmark and size reference for magnification correction.
- ◼
Proximal bowel: administer dilute oral contrast 45 minutes before the procedure to better identify peritoneoceles, omentoceles, and enteroceles.
- ◼
Anterior compartment (optional): in the supine position, at least 30 mL cystographic contrast is administered into the bladder through a Foley catheter.
- ◼
Middle compartment: at least 20 mL high density barium mixed with ultrasound gel is vaginally administered either by the patient or by an operator via a Foley catheter in the supine position.
- ◼
Posterior compartment: 200 mL of barium paste injected by hand via a large plastic syringe.
Images
- ◼
Sagittal rest.
- ◼
Sagittal dynamic images.
- ◼
Kegel.
- ◼
Strain.
- ◼
Evacuation.
- ◼
Other considerations
- ◼
Consider warming vaginal and rectal contrast for patient comfort.
- ◼
Remote fluoroscopic control is ideal for privacy during defecatory maneuvers.
- ◼
Images are usually acquired as fluoroscopic loops or 1 per second digital acquisitions.
Suggested magnetic resonance defecography protocol
Magnetic resonance imaging technique
- ◼
Sitting: patient assumes a sitting position in an open vertical bore magnet, simulating normal defecation and accentuating pelvic floor weakness by the effects of gravity, as is the case in FDG.
- ◼
Supine: patient assumes a supine position in a traditional horizontal bore magnet, which has been shown to have no significant difference compared with the sitting technique with regards to detection of clinically relevant pelvic floor abnormalities.
Contrast opacification
- ◼
Perineum and proximal bowel: not required, as these will be readily evident because of high contrast of magnetic resonance imaging (MRI).
- ◼
Anterior compartment: not required because the bladder is delineated by the presence of T2 bright urine contrasted with the T2 dark bladder wall. Avoidance of urination for at least an hour is advised to maximize distention of the bladder.
- ◼
Middle compartment: 50 mL of ultrasound gel (T2 bright) administered by the patient.
- ◼
Posterior compartment: 200 mL of ultrasound gel injected by an operator via a large plastic syringe.
Images
- ◼
Scout: T1 large field of view to identify the midline sagittal plane (including the pubic symphysis, bladder neck, vagina, rectum, and coccyx).
- ◼
Images
- ◼
Rest: T2 weighted sagittal, axial, coronal.
- ◼
Dynamic: T2 weighted or steady state sequence obtained around the midline sagittal plane (and possibly axial plane for better delineation of muscular defects), for high signal and temporal resolution.
- ◼
Kegel.
- ◼
Strain.
- ◼
Evacuation.
- ◼
- ◼
Normal appearance on all images is for the bladder neck, vaginal fornices, and anorectal junction to be at or above the pubococcygeal line (a line drawn between the inferior aspect of the pubic symphysis and the last coccygeal joint).
- ◼
Other considerations
- ◼
Warming the ultrasound gel will increase patient comfort.
- ◼
Covering the MRI bore with plastic sheets can help overcome any patient embarrassment or apprehension regarding evacuation.
Specific disease processes
Pelvic floor dyssynergy (anismus)
- ◼
A functional syndrome that is characterized by incomplete relaxation of the puborectalis muscle that limits normal defecation.
- ◼
This is thought to be psychological in etiology and does not typically respond to surgical treatment.
- ◼
FDG and MDG will show prolonged and/or incomplete evacuation of contrast. Findings of both prolonged and incomplete evacuation on FDG are reported to have a 90% positive predictive value for anismus.
Anterior compartment
Cystocele/urethrocele
- ◼
Cystocele is defined as descent of the bladder base below the pubococcygeal line.
- ◼
Urethrocele is defined as descent of the urethra into a horizonal orientation, as opposed to its normal vertical oblique orientation.
- ◼
FDG will demonstrate descent of an opacified bladder (below the pubococcygeal line if it can be drawn or otherwise inferred). If the bladder is not opacified, a cystocele is inferred by downward displacement of the vagina by an apparent extrinsic mass.
- ◼
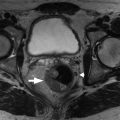
MDG will clearly demonstrate descent of the T2 bright bladder below the pubococcygeal line and straightening of the urethra into horizontal orientation ( Fig. 36.1 ).