10
Percutaneous Needle Biopsy and Drainage
The use of needle biopsy for nonoperative diagnosis became an acceptable diagnostic procedure in the 1930s, but it gained wide popularity in the 1970s, when computed tomography (CT) and sonography became available to guide interventional procedures.1 The original needles were large (16- or 14-gauge) and often placed blindly for tissue diagnosis of diffuse liver disease and palpable masses. With recent innovations in imaging techniques, instruments, and cytopathology, percutaneous biopsy now plays a significant role in patient care. Today, needle biopsy is the most frequently performed interventional procedure in radiology practice.2,3 Similarly, in the last two decades, percutaneous drainage (PD) has become a widely accepted treatment for intraabdominal abscesses.
The advantages of percutaneous procedures include lower morbidity rates, the use of local rather than general anesthesia, the elimination of surgical stress, shorter hospitalization, and decreased cost.4 Many uncomplicated and some complicated abscesses can be completely and permanently cured by PD. Other lesions can be treated temporarily with resolved infection, but a curative surgical procedure still would be necessary to eliminate any underlying cause. PD may render palliation, achieving symptomatic relief and defervescene in patients with limited life expectancy who are not candidates for curative surgery because of underlying comorbid conditions.5
 Procedure Planning
Procedure Planning
Because most biopsies and drainages are done under CT, the following discussion concentrates on CT approaches. Many of these concepts also apply to ultrasound. Percutaneous biopsy and abscess drainage should be planned on the basis of a recent high-quality diagnostic CT performed with intravenous (IV) contrast, which helps to assess the vascularity of the lesion and to identify adjacent vascular structures. Based on the available information, diagnostic possibilities should be discussed with the referring physician to plan an appropriate procedure. If a vascular lesion, such as hemangioma, arteriovenous malformation, or aneurysm, is suspected, additional noninvasive studies may be necessary for confirmation. All other lesions can be safely biopsied using at least a fine needle.
At the time of the procedure, a needle trajectory is drawn on the chosen section, and the level is marked on the scout view. In general, the shortest distance between the skin and the lesion should be traversed. This rule, however, is not always feasible because the shortest distance to the lesion may cross anatomic structures that should be avoided. Obviously, major vascular structures should be avoided, as should large nerves. The lung should not be intentionally traversed for investigation of subdiaphragmatic abnormalities. It is advisable not to cross large muscle groups because they are vascular, and a spontaneous muscle contraction may deflect the needle.6 Unnecessary puncture of parenchymal organs, particularly the spleen, should be avoided. Liver parenchyma, however, often is traversed with a fine needle for sampling of porta hepatic lymph nodes and adrenal, pancreatic, or biliary lesions as well as for gaining access to intrahepatic collections. We avoid penetration of the large bowel, even with fine needles, because of the possibility of infection. Although the risk of infectious complications is low in the immunocompetent population, a higher risk may exist for immunocompromised patients.6,7 Small bowel, stomach, and duodenum can be traversed with relative impunity using a fine needle.6,8 However, penetration of a hollow viscous with a large needle is inappropriate for tissue sampling. Small bowel and transverse and sigmoid colon often may be moved out of the path of the needle simply by repositioning the patient from a supine to a lateral decubitus position.6
 Preprocedure Patient Evaluation
Preprocedure Patient Evaluation
Referring physicians and careful chart review by the radiologist usually provide patient history and determine the presence or absence of serious concomitant conditions, such as cardiovascular, pulmonary, or neurologic disorders, as well as the ability of the patient to cooperate. We do not perform biopsies or drainages in an uncooperative patient without general anesthesia. Aspirin and other medications that potentially could alter coagulation and platelets should be discontinued one week prior to the scheduled procedure. Percutaneous procedures can be performed safely at any hematocrit level when coagulation is normal. When the hematocrit is below 32% or coagulation is abnormal, the risk of bleeding has more serious consequences. Patients with a history of abnormal bleeding and those with known clotting abnormalities also pose a higher risk. Most radiologists screen all patients for prothrombin time (PT), partial prothrombin time (PTT) and a platelet count. An acceptable PT is within 2 seconds of normal, PTT within 25%, and a platelet count above 70,000. When these parameters deviate from the acceptable levels, hematology consultation and appropriate corrective measures are mandated.
The patient is required to fast after midnight before the procedure. When the patient arrives in the radiology department, the procedure, alternatives, possible complications, and benefits are discussed, and the patient signs an informed consent form. A brief medical history is obtained, and vital signs are recorded. Prior to the procedure a peripheral IV line is placed. Anxious patients are premedicated according to the institutional conscious sedation protocol; however, this is rarely required for biopsies and actually may alter the patient’s ability to cooperate. During the procedure, the patient’s pulse rate and oxygenation are monitored by means of a pulse oximeter. Prior to percutaneous abscess drainage, patients should intravenously receive broad-spectrum antibiotics.
 Percutaneous Needle Biopsy
Percutaneous Needle Biopsy
Indications for percutaneous needle biopsy include (1) diagnosis of primary or metastatic malignancy in a newly discovered mass, (2) diagnosis of tumor recurrence in patients with known malignancy, (3) diagnosis of infection, and (4) diagnosis of benign disease. Common contraindications include (1) uncorrectable coagulopathy, (2) inability of the patient to cooperate, (3) a patient with uncontrollable cough (lung biopsy), and (4) lack of a safe needle path (with large–gauge needles).
Procedures and instruments
Percutaneous needle biopsy requires the accurate positioning of a needle into a lesion to obtain an adequate sample representative of the lesion. A sample can be obtained by either aspiration of pathologic material or by the mechanical cutting of tissues without suction. Typically, aspiration biopsy is performed with fine needles, most commonly 20- to 22-gauge, and is referred to as fine-needle aspiration biopsy (FNAB). A nonaspiration fine-needle technique (i.e., cutting tissue without the use of suction) may play a role in the diagnosis of extremely vascular lesions; otherwise, the aspiration technique is preferred for abdominal biopsies.9
FNAB is performed using needles with a variety of tip and stylet designs intended to improve diagnostic yield (Fig. 10-1). Some needles have blunt or beveled tips without cutting edges (aspiration needles) and are suitable for sampling practically any lesion.2 End-cutting needles have sharpened tips that can be hooked, notched, spiraled, or trephined, and they often are better for recovering diagnostic material from firm hypovascular masses. Needles with a beveled tip tend to recover better samples, because the small angle of the bevel allows superior diagnostic material to be obtained.10 Such needles, however, tend to deviate along the direction of the slant. Chiba and spinal needles appear to be a viable compromise.
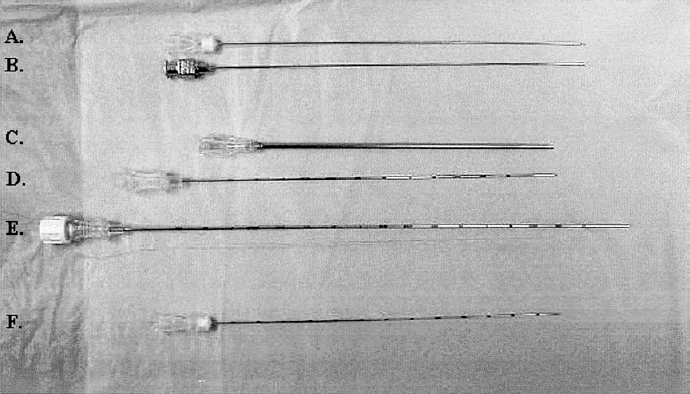
FIGURE 10-1. Various 22-gauge needles used for cytologic biopsies. (A) Chiba. (B) Spinal. (C) Turner. (D) Franseen. (E) Madayag. (F) Westcott.
The aspirated material then undergoes cytologic evaluation and occasionally is sent for histologic analysis when tissue fragments are present. Histologic material is more commonly obtained by using end-cutting rather than aspiration needles. Generally, the larger the needle, the greater the yield of diagnostic material.6,11 Several investigators reported higher diagnostic yields, without additional complications, using 20-gauge needles rather than 22- or 23-gauge needles.12,13 When overlying structures, such as liver, stomach, small bowel, and small vessels, are unavoidable, fine needles can be safely directed into the target lesion through these structures.8,14 The choice of a specific needle depends on the size, location, and vascularity of the lesion; the presence of intervening structures along the needle path; the amount of tissue required to satisfy diagnostic considerations; and the experience and preference of the operator. The Franseen and Westcott needles have the best overall performance, closely followed by the spinal needle.15
Usually, FNAB is sufficient for the diagnosis of carcinoma and recurrent malignancies as well as sampling of fluid. For the diagnosis of lymphoma, unusual tumors, or benign disease, however, large-bore cutting needle biopsies (LNB) are considered more accurate.16–18 This technique provides a sufficient histologic specimen while preserving the architecture of the lesion; however, the potential risks to the patient increase in quadratic proportion to the diameter of the needle.19 A variety of needles ranging from 14 to 19 gauge can be used for cutting biopsy and frequently are divided into end-cutting and side-cutting types. The former requires application of suction either by a syringe or a self-aspirating device, and the latter cuts along a gap in the inner stylet while an outer needle slides over the stylet, similar to a Tru-cut needle. Both the stylet and the outer needle can be moved manually or by using automated spring-loaded biopsy gun devices. In general, a superior specimen can be obtained by using side-cutting needles compared with end-cutting needles.
Automated biopsy devices consistently provide high-quality diagnostic tissue with minimal patient discomfort and no significant increase in the complication rate compared with FNAB.16,17,20 There is a variety of commercially available automated biopsy devices with different loading and safety mechanisms and with different throw lengths. Some devices have an adjustable throw ranging from 1 to 2 cm that can be tailored to the lesion size. Many automated biopsy gun devices are packaged with guiding cannulas for coaxial insertion of the needle. Instructions should be studied carefully before any new device is used. Some of these devices are unacceptably bulky and cumbersome, but overall automated devices are easy to use and consistently provide good-quality histologic specimens. We prefer an 18-gauge biopsy gun, which has a strong spring mechanism and is light weight, requiring no added support, with an optional feature of coaxial insertion and suitable for lesions of variable depths (Fig. 10-2).
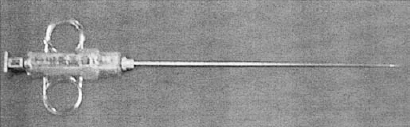
FIGURE 10-2. An example of a spring-loaded 18-gauge core biopsy needle.
Imaging guidance
Percutaneous biopsy can be performed with fluoroscopic, sonographic, CT or occasionally magnetic resonance imaging (MRI) guidance.21 The choice of imaging depends on the ability of the modality to visualize both the lesion and the needle with adequate depiction of the surrounding anatomy as well as the experience and personal preference of the radiologist and the availability of the equipment.
Fluoroscopy is a simple, fast, cost-effective, real-time technique used primarily for lung lesions that are well visualized in the frontal and lateral views. For small, difficult, ill-defined, or anatomically challenging lesions near the hilum or mediastinum, CT is the method of choice. Most abdominal biopsies are best performed with ultrasound or CT because these lesions cannot be visualized by fluoroscopy.
Previously limited to the liver and superficial lesion sampling, ultrasound guidance is currently being used with considerable success to biopsy lesions throughout the abdominal cavity and certain chest lesions.22,23 Ultrasound is less expensive and often less time-consuming than CT, and its multiplanar capability allows for needle passage in any plane in real time.
The procedure can be performed by using a freehand technique, a dedicated biopsy transducer, or biopsy guides attachable to a regular transducer.24 Motion and high-level echoes from the needle tip indenting adjacent tissues should be observed during the needle placement. A number of technical innovations and needle designs that improve visualization of the needle have been reported.25–27 Despite recent advances in ultrasonographic (US) guidance, the basic limitations still are related to difficulties in visualization of the needle tip, poor acoustic windows, interposed bowel gas, and large patient size.
In our experience and that of others,6,28 CT is the most effective modality for accurate needle biopsy, allowing visualization of most lesions and surrounding anatomy, therefore providing a safe biopsy route. The entire needle is readily visible on CT, allowing precise sampling of small and difficult lesions in complex anatomic regions such as the pelvis and retroperitoneum or near major vessels in the chest and abdomen. Repeat of previously failed biopsy should be performed with CT guidance to ensure the accuracy of needle placement. The disadvantages of CT guidance include high cost, often long procedure time, inability to scan in real time, and the limitation of a single scanning plane.
Biopsy techniques
Localization
The patient is placed on the CT table in a comfortable predetermined position that is appropriate for the planned needle insertion. Several axial sections are obtained that include the lesion. The proper level is marked on the skin with the gantry laser light, and the lesion’s projection on the skin is marked with a radioopaque marker (e.g., a paper clip or a commercially available, thin radioopaque grid). The position of the marker is verified on subsequent images and corrected if necessary to obtain the optimal entry point (Fig. 10-3). After sterile skin preparation, the entry site is infiltrated with 2% lidocaine to the level of the peritoneum, organ capsule, or pleura. All subsequent needle manipulations within the thoracic and abdominal cavity should be performed with suspended respiration to prevent a tearing effect of the needle tip.
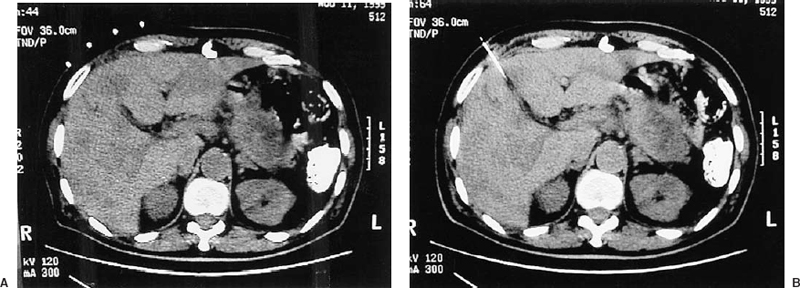
FIGURE 10-3. Single axial computed tomography image through the liver. (A) Radioopaque markers in preparation for percutaneous needle biopsy of a low-attenuation liver lesion. Note the mass in the pancreatic tail. (B) Needle tip is positioned well within the liver lesion.
A biopsy needle then is inserted into the lesion either by a single pass for superficial lesions or with incremental adjustment of depth and angulation for more difficult masses. To correct for inaccurate angulation, the needle should be withdrawn completely before any adjustment is made. After each adjustment, the position of the needle tip is radiographically verified. In-plane biopsies include lesions located at the same axial level as the skin entry plane. The procedure is simple; if any angulation is required, it is easily achieved in the same axial plane. In general, three 5- or 10-mm sections are obtained to verify the needle position.
Out-of-plane (angled) biopsies involve the sampling of lesions located above or below the skin entry point; thus, angulation in the longitudinal plane is required to reach the target. Often, additional angulation in the axial plane is also necessary. This procedure is more demanding and often lengthy because multiple adjustments of the needle are often required. Angulation of the scanning gantry may help to bring both the lesion and the needle in the same oblique plane, avoiding intervening structures.29,30
A longitudinal angle can be calculated using a “triangulation method”; however, it is difficult to implement precisely; therefore, this calculation is not practical.
Commercially available needle-guiding devices can be used for proper angulation. Increased accuracy and safety with these devices have been reported.31–33 Stereotactic devices for abdominal biopsy have shown a decrease in the number of needle manipulations by 75% and procedure time by 50% compared with hand guidance,34 but stereotactic systems are expensive and may be difficult to use.
Hand guidance, most commonly used for out of plane procedures, requires experience.6 We simply estimate the longitudinal angle evaluating sequential images. Once the angulation in the axial plane is correct, the needle is angled longitudinally and then moved incrementally toward the lesion. To verify the needle tip position, sequential images should be obtained from the needle entry point to at least 10 mm past the lesion. Sometimes four or more sections are needed to visualize the needle in its entirety. Sonographic guidance is often a better alternative for angled procedures.
To improve the efficiency and accuracy of multiple needle placements, a coaxial technique can be used for both FNAB and LNB, including automated devices.6,7 First, a short guiding cannula is inserted in the body wall and adjusted to achieve the proper direction. Then a biopsy needle is placed through the cannula to the desired depth.
FNAB sample
With the needle tip in satisfactory position, the stylet is removed, and a 20-mL syringe is attached to the needle; 5 to 10 mL of suction is applied while 1- to 2-cm quick, vigorous excursions are made through the lesion with some rotation of the needle. Suction can be maintained or slowly released during withdrawal of the needle. The aspirated material is expelled from the needle onto glass slides for cytologic smears and immersed in 95% alcohol for fixation prior to staining. The specimen should be examined by a cytopathologist in the biopsy suite. The aspirated syringe content is rinsed for cell-block preparation that is processed as a histologic specimen. Any tissue fragments are immersed in a 10% buffered formalin solution for histologic processing.
Multiple passes are often necessary to obtain diagnostic material.35,36 We limit the total number of passes to four. Regardless of the needle tip configuration, four passes with a 20-gauge needle yield diagnostic material in 95% of cases.15
Large-needle biopsy sample
At least one fine needle pass usually precedes LNB for obtaining cytology and as a test for lesion vascularity. Extremely vascular lesions are not sampled with large needles.
Once a large end-cutting needle is passed into the lesion, aspiration techniques are applied in a similar manner as FNAB. A side-cutting needle is placed at the margin of the lesion, and the position is checked. In some automated devices, the instrument is ready to fire at that time, and so the position of the cutting portion of the needle within the lesion cannot be verified. In other devices, the position of the inner stylet can be documented (and repositioned if necessary) after it is manually moved into the lesion. The obtained material is processed histologically.
Diagnostic yield
Image-guided percutaneous biopsy is an accurate procedure. The diagnostic accuracy varies because of differences in technique, the needles used, and the organ and lesions sampled. The range of sensitivities and specificities of CT-guided biopsies in general is 73 to 93% and 81 to 100%, respectively.37,38
Complications
The overall reported complication rates for abdominal needle biopsy range from 0 to 3%,6,39 with minor bleeding the most frequent and common complication; infection, pancreatitis, and pneumothorax are less common. Fatalities and needle-tract tumor seeding have been reported only rarely. One multiinstitutional survey of 16,381 biopsies reported 33 deaths related to FNAB,40 including 21 liver, 6 pancreatic, 2 adrenal, and 4 miscellaneous biopsies; the mean mortality rate was 0.031%. For cutting needles, serious complications are more common; however, a similar mortality rate of 0.027% was reported in more than 11,000 abdominal procedures.41 Seeding of malignant cells via the needle tract has been reported in 0.003 to 0.009% of FNAB, more commonly with renal cell carcinoma and pancreatic and musculoskeletal masses.40
Specific biopsy sites
Chest
Patient cooperation is absolutely essential when obtaining a chest biopsy because the patient must suspend respiration after a midexpiration. The goal of lung biopsy is to establish the presence of malignant cells, distinguish small cell from non–small cell tumor, and diagnose benign disease. Cytologic material is usually sufficient for nonlymphomatous malignancies; however, some common mediastinal masses (e.g., lymphoma and thymoma) and benign lung lesions often require large needle samples. Peripheral lung lesions are more commonly biopsied. Central lesions can be sampled percutaneously; however, a transbronchial approach is preferred to reduce the risk of significant hemorrhage and pneumothorax. An extrapleural (either anterior parasternal or posterior paravertebral) approach using CT or fluoroscopic guidance is preferred for mediastinal biopsy.42
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree