Indications
Currently there is no standard protocol used in selecting patients for renal biopsy. The overall frequency of renal biopsies ranges from 75 to 250 per 1 million population, depending on the selection criteria used by the treating nephrologist. The decision for renal biopsy is made largely by weighing therapeutic benefit against potential complications. After the exclusion of pre- and postrenal causes, unexplained acute renal failure with rapid deterioration of renal function is considered an absolute indication for biopsy, especially if there is coexisting nephritic urinary sediment with suspicion of rapidly progressive glomerulonephritis.1
In nephrotic syndrome, defined as the presence of proteinuria greater than 3.5 g/24 h/1.73 m2, renal biopsy is generally advocated in adults due to the broad differential diagnosis and the value of biopsy findings in directing appropriate immunosuppressant therapy.2 Renal biopsy is usually withheld in children under age 6 years with initial manifestations of nephrotic syndrome due to the fact that minimal-change glomerulonephritis exists in more than 90% of these patients.
In transplantation medicine, renal biopsy is used both in the acute postoperative period (to distinguish acute renal failure from acute rejection) and in patients with chronic allograft dysfunction.
The principal indications for renal biopsy are listed below:
Acute renal failure with rapid deterioration of function after exclusion of pre- and postrenal causes, especially if rapidly progressive glomerulonephritis is suspected
Nephrotic syndrome (proteinuria >3.5 g/24 h/1.73 m2); decide case-by-case in patients with suspected diabetic nephropathy
Glomerular hematuria and associated proteinuria >1 g/day
Renal involvement by systemic disease, especially in lupus erythematosus, vasculitis, and amyloidosis
The need to assess disease activity in response to immunosuppressant therapy
Acute and chronic loss of renal function after renal transplantation
Severe acute renal failure during pregnancy (except preeclampsia)
Isolated microhematuria is not an indication for renal biopsy. If microhematuria is associated with persistent proteinuria >1 g/day, histologic evaluation is recommended at most centers. In patients with advanced chronic renal failure (glomerular filtration rate <30 mL/min, kidney size <9 cm), renal biopsy is generally withheld due to the lack of therapeutic implications and higher complication rate (bleeding risk). Selected references may be consulted for further considerations on renal biopsy indications.1–5
25.2 Contraindications
Absolute prerequisites for an elective renal biopsy are a cooperative patient and an intact hemostasis system with a normal prothrombin time and partial thromboplastin time and a normal platelet count. Platelet function should be tested in patients with a prior history of bleeding episodes and may be tested in patients who have been taking antiplatelet drugs or NSAIDs. Platelet function can be assessed by the determination of bleeding time or by performing a platelet function assay (PFA).6 The PFA-100 analyzer provides better sensitivity and specificity than in vivo bleeding time.7 Contradictory data have been published on the significance of a prolonged bleeding time or abnormal PFA in predicting bleeding complications after renal biopsy.8–11 More recent studies have shown, however, that even aspirin use does not increase the risk of severe complications after ultrasound-guided percutaneous renal biopsy.12,13
On the other hand, we believe that antiplatelet drugs and NSAIDs should be stopped whenever possible prior to an elective renal biopsy. In some cases a prolonged bleeding time can be corrected by treatment with fast-acting desmopressin (0.3 μg/kg IV).14
Relative contraindications are hydronephrosis, pyelonephritis, renal abscess, uncontrolled hypertension (upper limit 150 mm Hg systolic and 95 diastolic), anomalies of renal shape and position (horseshoe kidney), large renal tumors, and small kidneys (increased bleeding risk). A single kidney does not contraindicate renal biopsy in carefully selected patients.2,14
25.3 Materials and Equipment
Special biopsy transducers (linear-array transducers) with an integrated biopsy channel as well as curved arrays with a side-mounted adjustable needle guide have proven effective for ultrasound-guided renal biopsies. Linear-array transducers provide high near-field resolution and stable contact with the skin, allowing for more accurate needle guidance. Both the transducer and needle guide are sterilized before each use.
The sector transducer has a smaller footprint and a more variable scan angle, which may be helpful in dealing with rib shadows or overlying bowel, for example. It also provides the cost-effective ability to convert an existing 3.5-MHz probe to a biopsy transducer by adding a biopsy attachment (▶ Fig. 25.1 and ▶ Fig. 25.2).

Fig. 25.1 Curved-array transducer with an adjustable needle guide.
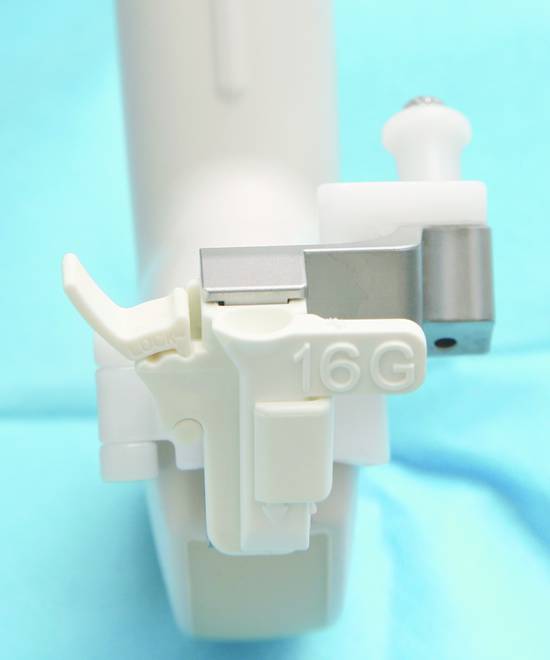
Fig. 25.2 Curved-array transducer with an adjustable needle guide, close-up view.
Most ultrasound manufacturers offer adjustable needle guides for their transducer systems. We use a sterile, disposable procedure kit that includes a needle guide and inserts for 14-gauge to 18-gauge needles, sterile ultrasound gel, and a sterile transducer cover (▶ Fig. 25.3).

Fig. 25.3 Sterile, disposable procedure kit with needle guide and inserts, ultrasound gel packet, and a sterile disposable transducer cover (Ultra-Pro II needle guide [Civco]). A Max-Core automated sterile disposable biopsy device (Bard) and other materials are also shown.
A core biopsy technique using special 14- to 18-gauge Trucut needles (length 16 or 20 cm) has become widely practiced for percutaneous renal biopsies. Larger needles yield a greater number of glomeruli per core. Recent prospective randomized studies have shown no difference in the rate of bleeding complications with 14-gauge or 16-gauge needles in native kidneys or with 14-, 16-, or 18-gauge needles in renal allografts.9,15 We generally use a 16-gauge needle for biopsies of native and transplanted kidneys (or an 18-gauge needle in selected cases).
Various suppliers offer both sterile disposable biopsy systems and sterilizable biopsy guns with sterile biopsy needles available separately.
25.4 Preparations
Informed consent should cover all the steps in the procedure, possible complications, and postbiopsy patient instructions. For forensic reasons, informed consent should be obtained on the day before the procedure and should be documented in writing. For a native kidney we generally biopsy the lower pole of the left or right kidney through a posterior approach in the prone patient. Most modern ultrasound systems have special biopsy programs that can superimpose the needle path on the screen. The patient should be fasted for 6 hours before the procedure but is allowed to drink liquids. Morning medications, especially for blood pressure, should be taken as usual. A prolonged cessation of fluid intake should be avoided in freshly transplanted patients. Laboratory values should include current coagulation status, simple blood count, creatinine, urea, and urinary status. Intravenous access should always be established. Body hair should be shaved over a wide area around the puncture site.
25.5 Procedure
25.5.1 Native Renal Biopsy
After all necessary instruments have been laid out on a sterile table, the patient is positioned prone for biopsy of the native kidney. A foam roll is placed beneath the abdomen at the level of the umbilicus. With the patient in this position, the kidney should again be imaged sonographically prior to sterile draping and a suitable entry site marked on the skin with a permanent felt marker. At full inspiration the entry site should be as close to the lower renal pole as possible with adequate clearance from the lower ribs. Biopsy through the intercostal space should be avoided due to the risk of pneumothorax. If access is obstructed by ribs or bowel, the procedure should be switched to the contralateral kidney. The distance from the renal capsule to the skin should be determined to make sure that the biopsy needle, which has a centimeter scale, is not advanced too deeply.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








