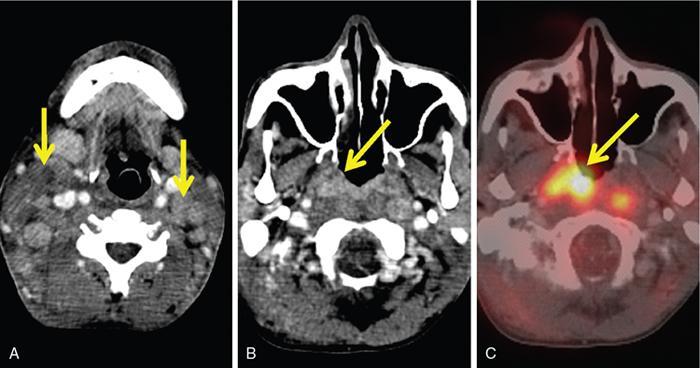
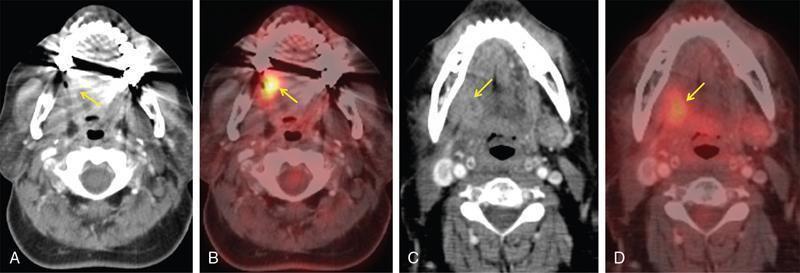
Chandramohan Sivanandam, Arun Ramraj PET-CT is a fusion of PET and CT imaging, providing both anatomical (CT) and functional (PET) details of the tumour. PET imaging is based on the coincident detection of two photons released when a positron annihilates an electron. The released photons travel in opposing directions (180 degrees to each other) to be detected by ring detector module containing scintillation crystals made up of lutetium oxyorthosilicate (LSO) or bismuth germinate (BGO). PET utilizes (F18)-fluoro-2-deoxy-d-glucose (F-18-FDG), a radiopharmaceutical analogue of glucose. Rapidly proliferating cells in a tumour actively take up the injected F-18-FDG. After phosphorylation, the trapped FDG-6 phosphate releases a positron which undergoes immediate annihilation with an adjacent electron to release two photons. The rate of uptake of F-18-FDG is proportional to the metabolic activity of the tumour. PET images are acquired approximately 60 min after injection of F-18-FDG (0.1 mCi/kg body weight3). Postinjection, restriction on patient movement and speech are imposed to minimize physiologic uptake from neck muscles and larynx. F-18-FDG uptake at a particular site is measured in maximum standardized uptake value (SUV-max). Usually, tumours have an SUV-max of more than 2.5 to 3.0. CT images are routinely acquired with iodinated contrast media, unless contraindicated. Three sets of images are produced PET, CT and fused PET-CT. Even though CT and MRI remain the primary imaging modalities for evaluating the pretreatment locoregional spread of cancer, PET-CT has a definite role in the following situations. Around 5%–10% of head and neck cancers present as cervical lymphnode metastases with unknown primary site of tumour, despite thorough clinical examination and endoscopy, CT/MRI evaluation. In such a clinical setting, PET-CT detection of primary tumour ranges from 5% to 73% with better detection rates for nonsquamous cell cancers (Fig. 3.38.1). False negative in PET-CT occurs when the primary tumour is very small (T1 disease) or when the primary tumour is situated in regions with high background physiologic uptake, i.e. tonsils, adenoid. PET-CT has revolutionized posttreatment tumour response assessment. As both surgery and radiotherapy cause tissue fibrosis, scarring and oedema with blurring of normal anatomy, it becomes difficult to differentiate tumour from posttherapy changes using conventional CT and MRI. Chemoradiotherapy and surgery produce inflammation at the tumour site. Inflammatory tissue has increased metabolic activity with resultant high FDG uptake. Ideally, posttreatment PET-CT is acquired 12 weeks after completion of treatment to avoid false positive from the inflammatory response to treatment (Fig. 3.38.2).
3.38: PET-CT in head and neck cancer
Role of PET-CT in head and neck cancer
Identifying unknown primary tumour
Assessing tumour reponse – postchemoradiotherapy or surgery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree