PET/CT Imaging of Infection and Inflammation
Ora Israel
Nuclear medicine plays an important role in the assessment of a multitude of infectious and inflammatory processes. Functional scintigraphic procedures are part of the noninvasive diagnostic armamentarium for assessment of infection and inflammation and should be viewed by the referring clinicians and the imaging community as complementary to, and not as competing with, anatomic modalities such as x-rays, computed tomography (CT), magnetic resonance imaging (MRI), or ultrasound. A number of radiotracers using single-photon emitting radionuclides have served for decades as infection and inflammation-seeking agents. The widest experience has been gained with gallium-67 ([67Ga]) and leukocytes (white blood cells [WBC]) radiolabeled with either technetium-99m (99mTc) or indium-111 ([111In]). Immunoscintigraphy using various labeled antibodies has also been introduced in recent years using single photon agents and is in clinical use in many parts of the world
With the increasing use of fluorine-18-fluorodeoxyglucose ([18F]-FDG) for assessment of malignancies, uptake of this positron-emitting tracer in nonmalignant processes has also been described. FDG is a tumor-seeking, but not a tumor-specific, imaging agent. Accumulation of increased FDG uptake in benign, infectious, and inflammatory processes was initially described as an incidental finding, labeled as a pitfall and cited as a cause for false-positive results in imaging cancer patients (1). This initial observation was followed by the understanding that diagnosis and monitoring of infectious and inflammatory processes may represent an additional important indication for FDG positron emission tomography (PET) imaging.
The further technological development of the hybrid PET/CT technology (2,3) has given a new dimension to combined metabolic and anatomic evaluation of infection and inflammation, with a significant impact on patient care as currently demonstrated by an increasing number of publications in ever expanding clinical indications.
Mechanism of Fluorodeoxyglucose Uptake and Technical Aspects of PET/CT in Infection and Inflammation
The basis for FDG accumulation in malignant cells has been extensively described in other chapters of this book. However, cancer is not the only process characterized by increased glycolysis and glucose utilization. Inflammatory cells such as activated lymphocytes, neutrophils, and macrophages are present in infectious and inflammatory processes. Similar to malignant cells, they exhibit, high intracellular levels of hexokinase and increased expression of surface glucose transporter proteins with a high affinity for FDG, and sufficient intracellular adenosine triphosphate to allow phosphorylation of FDG to FDG 6-phosphate, and therefore develop a high cytoplasmic concentration of the phosphorylated product (4,5,6). Activated cells present in inflammatory and infectious processes also have a high capacity for accumulating FDG, probably due to their stimulation by large amounts of cytokines and growth factors among other factors (7).
The initial incidental clinical observation of FDG uptake in nonmalignant processes has been further evaluated in animal models, confirming the affinity of this tracer for benign hypermetabolic
processes (6,8,9). Experimental studies have demonstrated increased glucose uptake in inflammatory cells during the acute stage of the process (9,10). Abscess forming bacteria use glucose as their energy substrate (11). Furthermore, FDG uptake in experimental infectious processes, expressed as the lesion to background ratio, was higher when compared to that of [67Ga] (12).
processes (6,8,9). Experimental studies have demonstrated increased glucose uptake in inflammatory cells during the acute stage of the process (9,10). Abscess forming bacteria use glucose as their energy substrate (11). Furthermore, FDG uptake in experimental infectious processes, expressed as the lesion to background ratio, was higher when compared to that of [67Ga] (12).
The next step was the implementation of these experimental results to patient studies, specifically challenging the hypothesis that FDG PET may be used in the clinical setting for imaging and evaluation of infection and inflammation in humans. FDG is taken up by most infectious and inflammatory processes in a large variety of organs. This was documented first by case reports appearing in the literature over more than two decades, followed in recent years by studies involving larger number of patients. One of the early papers describing the use of FDG PET for detection of infection evaluated 11 patients with known or suspected infectious processes. FDG PET correctly diagnosed 10 of 11 patients (13).
The development of this field of clinical research and practice has progressed at a relatively slow pace for a number of reasons. Failure, at the time this chapter was written, to reimburse PET studies performed for assessment of infection has limited its use to a few academic centers with a specific research interest in the field. In addition, the relatively long list of differential diagnoses for FDG-avid sites and the low spatial resolution of early stand-alone PET imaging devices have made precise definition of suspicious lesions difficult. This raised concerns about the certainty of the reported findings, their etiology, and localization.
The use of hybrid imaging in general, and PET/CT specifically, in the evaluation of infectious and inflammatory processes, similar to their implementation for cancer imaging, has decreased the overall uncertainty and the number of equivocal readings (3,14). In order to improve the differential diagnosis between malignant and infectious or inflammatory processes, the use of threshold standard uptake value (SUV) measurements have also been recommended by some, as well as dual time point acquisition showing different dynamics of FDG retention in lesions with a different etiology (15,16).
A number of practical advantages make FDG PET/CT one of the procedures of choice for assessment of patients with infection and inflammation. [18F] has good physical properties and FDG has good tracer kinetics with rapid accumulation in infections, better than that of single-photon emitting radionuclides used in this clinical context. The short physical half-life is responsible for lower radiation doses delivered to patients who undergo, as a rule, a large number of imaging procedures using ionizing radiation. The fact that the physical characteristics of the agent require the procedure to be performed within an approximate time of 2 hours should not be viewed as a limitation, but rather represents an additional advantage by providing clinical results within a short time span. In addition, PET devices provide images with better spatial resolution and higher contrast as compared to single-photon emission computed tomography.
Limitations of FDG imaging of infection and inflammation are related in part to the normal tracer biodistribution of FDG. Lesions or suspicious FDG-avid foci located in organs with, or in close vicinity to areas of high physiologic tracer concentration may be misinterpreted as false-positive as well as false-negative findings. The recent addition of a CT component to PET in the form of PET/CT has lead to improvement in the spatial localization of findings and makes this less of a limiting factor both in patients with malignancy and in those assessed for the presence or the suspicion of an infectious process.
Infection is a major and severe complication of patients with diabetes mellitus. FDG imaging may have a lower sensitivity in the presence of high blood glucose levels (17). A decrease in FDG uptake in experimental inflammatory and infectious processes has been found in the presence of high serum glucose levels due to a decreased expression of glucose transporters (GLUT1 and GLUT3) and also due to direct competition with unlabeled glucose for tracer uptake (18). Preliminary patient studies suggest, however, that this factor does not represent a major limitation for assessment of infectious processes in the clinical setting (19,20).
An additional practical issue that has not yet received sufficient evaluation is the potential influence of prior antibiotic treatment on FDG uptake. Although relevant evidence in literature data is still lacking at present, it is suggested that the sensitivity of FDG imaging decreases in partially treated infectious processes.
Fluorodeoxyglucose PET/CT Imaging of Musculoskeletal Infection and Inflammation
The use of FDG PET for diagnosis and monitoring patients with suspected infectious or inflammatory processes involving the musculoskeletal system is one of the most extensively investigated noncancer-related areas of research for clinical PET/CT.
Diagnosis of Acute or Chronic Osteomyelitis
For decades, nuclear medicine techniques have played a role in diagnosis of acute and chronic osteomyelitis, mainly with the use of three-phase bone scintigraphy, labeled WBCs with or without bone marrow imaging, and [67Ga] scintigraphy. Although these procedures still are, at present, principal diagnostic tools in routine clinical scenarios, FDG has been shown to accumulate in infectious processes involving the bone. FDG PET imaging has been advocated for the more complicated diagnostic challenges, such as diagnosis of chronic osteomyelitis, frequently resulting from a continuing, insufficiently treated acute infection, vertebral osteomyelitis or discitis, and bone infection in diabetic patients, mainly the diabetic foot.
Chronic osteomyelitis is defined, as a rule, as an infectious process involving the skeleton that requires more than a single episode of treatment and persists for more than 6 weeks (21). Diagnosis is difficult since the prolonged infectious process, as well as previous treatment, can frequently alter the normal regional bone anatomy and physiology and also due to the low-grade nature of the disease (22). A variety of imaging techniques have been used for noninvasive diagnosis of chronic osteomyelitis, including plain x-rays, CT, MRI, general nuclear medicine techniques, and FDG PET.
Among the studies that assess the role of FDG PET for imaging chronic infection of the bone, most have demonstrated a high sensitivity and a specificity ranging between 88% to 92% (23,24). FDG PET was found to be superior to [111In] WBC for assessment of chronic osteomyelitis (25). FDG PET was also assessed in 60 patients with a suspected chronic musculoskeletal infection involving the central or peripheral skeleton. All patients with a final diagnosis of chronic infection were correctly identified. The sensitivity, specificity, and accuracy of FDG PET were 100%, 88%, and 93%, respectively, similar for suspected infections in the axial and appendicular skeleton (26).
A recent meta-analysis provided a systematic review of 23 clinical studies reporting on the accuracy of the different imaging modalities for diagnosis of chronic osteomyelitis (22). The pooled data demonstrated that FDG PET imaging had the highest sensitivity, 96%, compared to 78% for combined bone and WBC scintigraphy, and 84% for MRI. The specificity of FDG PET was 91% as compared to 84% for combined bone and WBC scanning and 60% for MRI. The authors concluded that based on this extensive peer-reviewed data FDG PET surges as the modality with the highest diagnostic accuracy for diagnosis or exclusion of chronic osteomyelitis, in particular in the axial skeleton (22).
Diagnosis of vertebral or disc space infection, with an incidence of 2% to 4% of all cases of osteomyelitis, is another diagnostic dilemma, even with the extensive use of MRI (27). Conventional nuclear medicine infection-seeking tracers also have a lower sensitivity in the vertebrae or spine as compared to other skeletal sites. FDG PET was successfully used in 30 consecutive patients for the differential diagnosis of degenerative spinal disease versus disc-space infection and showed better performance, with a reported 100% sensitivity and specificity as compared to MRI, which had a sensitivity of 50% and a specificity of 96%. Although FDG PET is not recommended as the first-line diagnostic modality in patients with back pain of unclear etiology, the authors suggest its use in cases with equivocal MRI findings (28).
Infectious processes represent a major complication in patients with diabetes. Angiopathy and neuropathy induced by severe diabetes lead to infectious processes that can involve the skin, soft tissues, and bone, mainly in the pedal region. Differential diagnosis of the “diabetic foot” is important for patient management with the goal of defining various pathological processes that require different therapeutic strategies (29). Current treatment of early stage Charcot neuroarthropathy in the diabetic foot includes surgery if it has not been performed previously. In a study of 39 diabetic patients FDG PET successfully diagnosed Charcot joint lesions and was superior to MRI (30).
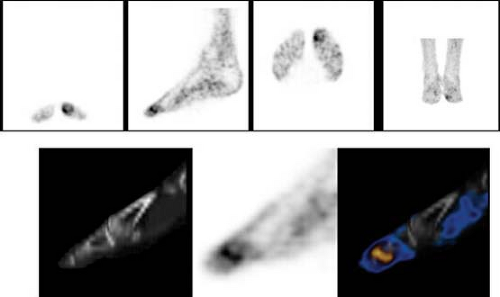
Clinical diagnosis of osteomyelitis in the feet of diabetic patients is important for further treatment planning, but difficult. Although PET can show the presence of an FDG-avid focus in sites of acute infection, PET/CT has been shown of value for differentiating between osteomyelitis and soft tissue infection (Fig. 12.1) (20). In a preliminary study involving 14 patients, FDG PET/CT correctly localized eight foci of abnormal tracer uptake to the bone and thus enabled the diagnosis of osteomyelitis. A single site of mild FDG activity was falsely interpreted as bone infection, while the final diagnosis indicated a Charcot joint. The precise localization provided by PET/CT with a subsequent correct diagnosis directed further treatment toward surgery in patients with osteomyelitis as compared to conservative treatment in patients with soft tissue infection (20).
Infection Involving Metallic Implants and Joint Prostheses
Pain is common in patients following implant of joint prostheses. The differential diagnosis of a painful joint transplant includes loosening as a result of mechanical failure or, in a smaller percentage of patients, periprosthetic infection (31). In spite of the similar clinical presentation, a preoperative differential diagnosis is essential, since they result in different treatment strategies, revision surgery as compared with long-term antibiotic therapy followed by surgery. Diagnosis of an infected joint prosthesis is made using a variety of laboratory tests, including microbiological cultures, imaging with conventional x-ray radiography, and general nuclear medicine procedures, which could include a combined approach of three-phase bone scintigraphy, an infectious-seeking agent, such as [67Ga] scintigraphy, or labeled WBCs associated at times with bone marrow scintigraphy (32,33,34). However, this complex battery of diagnostic tests provides suboptimal results with a low sensitivity and specificity (35).
Patients with metallic implants after trauma or bone surgery can also present with a clinical suspicion of infection. Diagnosis of osteomyelitis in the complicated postsurgical bone is important but impaired by the low specificity of laboratory data and the relatively low performance of conventional anatomic imaging and nuclear medicine procedures. MRI, one of the major tools for assessment of musculoskeletal pathology in general, is of limited use in the
presence of metallic devices due to technical artifacts and also to a variable and nonspecific imaging pattern (36).
presence of metallic devices due to technical artifacts and also to a variable and nonspecific imaging pattern (36).
Literature data with respect to FDG imaging of suspected infection of prosthetic joints has been accumulating. Initial studies have shown that FDG PET can differentiate loosening from infection of a joint transplant with variable accuracy (37,38). An early feasibility study evaluated FDG PET for diagnosis of 74 hip or knee prostheses suspected of infection. FDG PET had a sensitivity, specificity, and accuracy of 91%, 72%, and 78%, respectively, for assessment of knee prostheses, and 90% for all three indices in cases of hip arthroplasty, with an overall sensitivity of 91% and a specificity of 82% (38). In another study, FDG PET was evaluated and compared to three-phase bone scintigraphy in 92 hip joint prostheses in 63 patients (39). FDG PET had a sensitivity of 94%, and specificity and accuracy of 95%, significantly higher when compared with 68%, 76% and 74% respectively for bone scintigraphy. The authors, however caution that increased periprosthetic FDG uptake may be also found in patients with aseptic loosening due to tracer uptake in granulomatous tissue that develops around the implanted device. Indeed, the authors’ own experience and that of other groups has shown that some uptake of radiotracer around joint prostheses is relatively common.
Another recent study assessed the performance of FDG PET in 27 patients prior to surgical revision procedures of hip and knee endoprostheses (40). Aseptic loosening was diagnosed with high (96%) sensitivity. FDG PET diagnosed all cases of infected arthroplasty and approximately half of the cases that showed an aseptic inflammatory reaction. These authors also conclude that, while a negative PET study may spare revision surgery, a positive result cannot give a clear differentiation between a septic process or an aseptic inflammation, caused as a rule by a foreign-body reaction. Thus, it appears that false-positive results represent a current challenge with the FDG PET approach.
Overall, FDG PET has a diagnostic accuracy ranging between 68% to 100% for assessment of patients with prostheses of the hip joint and between 78% to 100% in evaluation of knee arthroplasty (35). Positive FDG PET studies in patients with lower limb joint prostheses should be interpreted with caution. False-positive results occur due to the presence, sometime for decades, of nonspecific increased tracer activity in sites of granulomatotic tissue developing around the implant (41).
The diagnosis of infection in the postoperative spine, as well as in complicated bones following fractures or surgery, remains a diagnostic challenge, and FDG PET imaging has been assessed in this group of patients. Although in most studies these patients are analyzed as part of a larger population with various clinical scenarios, without addressing the performance of FDG imaging in this specific group, authors agree that it represents a promising diagnostic imaging test. A study assessing FDG PET in 29 patients with a suspicion of metallic implant–associated infections after trauma indicated a sensitivity of 100%, specificity of 93%, and accuracy of 97%, higher for lesions in the axial skeleton. Furthermore, the referring physicians reported an impact of FDG PET reports on further patient care in almost two of three patients in this series (42).
Assessment of FDG PET in 57 patients suspected of having spinal infection after previous surgery of the vertebral column showed a sensitivity of 100%, specificity of 81%, and accuracy of 86%, with most of the false-positive studies occurring over a longer postoperative period and in the presence of metallic implants (43). Hybrid PET/CT will further improve the diagnostic capabilities of FDG imaging by reducing the number of false-positive reports (44).
Only a few studies have reported on the use of combined PET/CT devices in suspected infection after arthroplasty. Early studies have described the presence of metal artifacts that can decrease the accuracy of x-ray attenuation correction in the clinical context of assessing patients with arthroplasty (45,46,47). It is therefore recommend to routinely assess both corrected and uncorrected PET images in order to decrease the rate of false-positive reports related to artifactually increased FDG activity (35).
A recent study evaluated 33 patients after trauma with suspected osteomyelitis in the axial or peripheral skeleton using FDG PET/CT, with 18 of these patients having a metallic implant. The sensitivity, specificity, and accuracy were 94%, 87%, and 91%, respectively. The authors conclude that FDG PET/CT is an accurate method for the evaluation of chronic infection in patients after trauma, regardless of the presence of metallic devices. The use of fused images enables accurate diagnosis with precise anatomical localization of the suspicious site and precise delineation of the extent of the infectious process (48).
Inflammatory Joint Diseases
Inflammatory processes involving the joints, such as rheumatoid arthritis, degenerative diseases, or synovitis, have been reported to show increased FDG activity of moderate intensity (49). The whole-body capability of PET/CT and the ability to detect changes in the degree of metabolic activity make FDG imaging a potentially useful tool for defining the extent of disease and for monitoring response to treatment. If a site of increased FDG uptake is located on PET/CT in the periarticular synovia the potential of an active arthritic process should be raised.
In patients with rheumatoid arthritis the degree and extent of FDG uptake is related to the intensity of clinical symptoms such as pain, swelling, and tenderness (50). A study assessing over 300 joints in 21 patients showed that the degree of synovial FDG uptake is a good and reliable index of disease activity (51). Further studies are needed to define the role of FDG PET/CT imaging in patients with active arthritic processes, for diagnosis of early stage disease, for monitoring response to treatment, or when there is a suspicion of exacerbation with an acute or chronic process.
Fluorodeoxyglucose PET/CT Imaging of Fever of Unknown Origin and Focal Soft Tissue Infections
Fever of unknown origin (FUO) defines a large number of entities characterized by prolonged (more than 3 weeks) hyperthermia (over 38.3ºC/101ºF) of no specific etiology in spite of an extensive diagnostic work-up. Although some of the processes defined as FUO are self-limited and resolve without any specific treatment, a variety of diseases that have severe outcome consequences if untreated can present with this clinical picture. This is the reason
for the diagnostic effort invested by clinicians in finding the cause for FUO, a work-up that has major impact on patient care and also puts a substantial financial burden on the health system.
for the diagnostic effort invested by clinicians in finding the cause for FUO, a work-up that has major impact on patient care and also puts a substantial financial burden on the health system.
The differential diagnosis of FUO includes over 200 causes that have been reported and can be classified into four major categories: infectious, malignant, aseptic inflammatory processes, and miscellaneous (53). Infections represent the main etiology in up to 30% of patients (54,55), mostly of bacterial origin, and include diseases such as tuberculosis, abdominopelvic abscesses, endocarditis or osteomyelitis, and, less frequently, viral infections due to agents such as cytomegalovirus, Epstein-Barr virus, or human immunodeficiency virus (HIV). The second more common cause for FUO are malignancies, mainly lymphoma, leukemia, renal cell carcinoma, or metastatic tumors to the liver, followed by inflammatory processes such as arthritis, arteritis, or other vasculitic processes, inflammatory bowel disease, or systemic lupus erythematosus (54,55). Additional diseases that can cause FUO, include, among others, drug-induced fever and deep vein thrombosis (55).
Although diagnosis of the cause of FUO is difficult, the goal of extensive evaluation of patients with prolonged fever is to reach 90% of patients who should have a recognizable etiology (56). Diagnostic techniques involve a variety of laboratory, imaging, and invasive procedures. Imaging for FUO includes most anatomic modalities, conventional x-rays, ultrasound, CT, and MRI (57,58). General nuclear medicine procedures are also widely performed using tracers such as [67Ga], [111In], or 99mTc WBC-labeled antibodies, and antibiotics, however, with limited and variable rates of success (59,60,61).
The potential role of FDG PET in the work-up of patients with FUO was evaluated. FDG is taken up by many infectious processes and inflammatory entities, and imaging of the whole body is of greater importance when the unknown focus of infection can be localized in any region of the body. The overall capability of FDG PET to provide clinically useful information in patients with FUO ranges in the early literature data between 35% to 70% (62,63,64,65,66). The results reported, however, are based on studies performed in a small number of patients, using at times insufficient doses of FDG and imaging devices with variable technical performance capabilities.
One of the early studies reported that FDG PET diagnosed the etiology of prolonged hyperthermia in 11 of 16 patients with FUO, including mainly infectious and connective tissue processes, and one case of malignancy (64). PET was negative in two patients with further diagnosed rheumatic fever and in two patients for whom no final diagnosis could be established and then recovered within 3 months, spontaneously or with nonspecific antibiotic treatment. An additional study assessed the value of FDG PET in a group of 58 patients with FUO (62). In this group the final etiology of prolonged fever was established in only 69% of patients. FDG PET was positive in 79% and helpful for establishing the final diagnosis by correctly identifying the source of fever in 41% of the patients. In the same study the performance of FDG PET was compared and found to have a higher sensitivity than [67Ga] scintigraphy in a subgroup of 40 patients.
The performance indices of FDG PET were also evaluated in a study involving 35 patients with FUO (65). FDG PET had a sensitivity of 93%, specificity of 90%, positive predictive value of 87%, and a negative predictive value of 95% for defining the cause of FUO, with clinically helpful studies in 65% of patients. FDG PET correctly pointed to the source of fever in 13 patients, but was false positive in two patients, including one patient with focal colonic
tracer uptake and one patient with increased FDG activity in multiple lymph nodes. Histological tissue sampling was negative and fever resolved in both patients, with no further evidence of disease in the suspected sites. FDG PET was true negative in 94% of patients with no evidence of focal infection, and in those without a known cause of FUO. A study involving 74 prospectively collected patients, with a final diagnosis established in 53% of the group, indicated that FDG PET was positive in 53 of 74 patients (72%) (66). Based on the final diagnosis, 36% of the positive studies were considered to be clinically helpful.
tracer uptake and one patient with increased FDG activity in multiple lymph nodes. Histological tissue sampling was negative and fever resolved in both patients, with no further evidence of disease in the suspected sites. FDG PET was true negative in 94% of patients with no evidence of focal infection, and in those without a known cause of FUO. A study involving 74 prospectively collected patients, with a final diagnosis established in 53% of the group, indicated that FDG PET was positive in 53 of 74 patients (72%) (66). Based on the final diagnosis, 36% of the positive studies were considered to be clinically helpful.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree